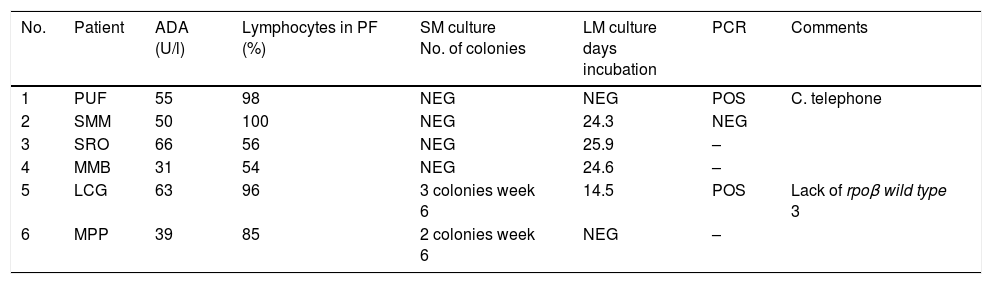
Pleural tuberculosis (PT) is a significant cause of tuberculosis (TB) in our region of Castile and León and, along with genitourinary tuberculosis, is the most common cause of extrapulmonary TB. With respect to all positive cultures for Mycobacterium tuberculosis (MT), the proportion of positive cultures in pleural fluid (PF) ranged from 5.18% in 2013 to 6.54% in 2016. The number of cases of PT has remained around 14 annual cases confirmed by culture, while over the same time there was a decrease in the number of cases of pulmonary TB. A previous 17-year study conducted in our Bierzo health board area1 revealed that only 2.5% of PF samples are positive for MT culture. In view of this situation, we decided to look for a system for selecting PF samples to improve the performance of mycobacterial cultures and optimise the use of molecular techniques on those samples. We assessed a total of 200 PF samples collected from 2015 to 2018. The adenosine deaminase (ADA) value was determined in all of the samples, establishing the cut-off point at 30U/l, above which PT is suspected in our health board area. All samples were seeded in solid culture media (Coletsos and Middlebrook 7H11) and automated liquid media (BacT/ALERT® MP) and incubated for at least 6 weeks. When ADA was found to be above the cut-off point, the automated liquid medium was re-seeded at the end of the incubation period and incubation of all the bottles was prolonged for at least three more weeks. Identification of MT was performed by molecular techniques (GenoType® MTBC and GenoType® MTBDR, Hain) and the PCR on direct sample was performed with GeneXpert® MTB-RIF (Izasa®). When the ADA value is dispensed with, MT growth/PCR+ is only obtained in 3% of the PF samples. When an ADA value of 30 U/l or above is used (51 cases, 25.5% of PF), the rate of growth/detection by PCR increases to 11.76% (6 cases). As shown in Table 1, there was no doubt that the pleural effusion was predominantly lymphocytic in all the samples, with figures ranging from 54% to 100%. MT growth was obtained in solid media in only two cases, and only two to three colonies grew after the first six weeks of incubation. The growth of MT in liquid media occurred in four cases, with a mean of 22 days; growth was negative in two cases. No MT growth was obtained in any of the 149 PF samples with ADA values below 30U/l. According to a recent review, the method of determining ADA values and establishing cut-off points adapted to regions with a high TB rate has a high discriminatory power; in contrast, in low-incidence regions, it would have a high negative predictive value.2
Cases of pleural tuberculosis in which growth of mycobacteria was obtained, and in which the ADA value, the percentage of lymphocytes in the PF, the result of the culture in solid and liquid media and the detection by PCR in direct sample were specified.
| No. | Patient | ADA (U/l) | Lymphocytes in PF (%) | SM culture No. of colonies | LM culture days incubation | PCR | Comments |
|---|---|---|---|---|---|---|---|
| 1 | PUF | 55 | 98 | NEG | NEG | POS | C. telephone |
| 2 | SMM | 50 | 100 | NEG | 24.3 | NEG | |
| 3 | SRO | 66 | 56 | NEG | 25.9 | – | |
| 4 | MMB | 31 | 54 | NEG | 24.6 | – | |
| 5 | LCG | 63 | 96 | 3 colonies week 6 | 14.5 | POS | Lack of rpoβ wild type 3 |
| 6 | MPP | 39 | 85 | 2 colonies week 6 | NEG | – |
ADA: adenosine deaminase; LM: automated liquid culture medium for mycobacteria (BacT/ALERT® MP, bioMérieux); NEG: negative; PCR: detection of Mycobacterium tuberculosis complex by genome amplification (GeneXpert®, Hain Lifescience); PF: pleural fluid; POS: positive; SM: solid culture media for mycobacteria (Coletsos, Middlebrook 7H11).
The main disputable factor is the determination of the cut-off point which enables differentiation of TB from other processes, and varies widely according to the following parameters: (1) the prevalence of TB in the geographical area studied; (2) the age of the patients, as in patients over 55, the cut-off point would drop to 26IU/l, while in the under-55s it would rise to 72IU/l,3 and (3) the number of cases studied. In a study of 2413 cases of pleural effusion duly classified according to aetiology and with a mean age of 65, the mean cut-off point was set at 28.26IU. Values above 100IU/l were related to lymphoproliferative processes, carcinomas, para-malignant effusions and empyema.4 In 2015, the average incidence of TB in Castile and León was 9.93 cases per 100,000 population, with an average incidence of PT of 0.77 cases per 100,000 population.5 The province of León, and especially the county of Bierzo, continue to be the areas with the highest incidence of TB in the region. The selection of PF samples for TB detection could be established initially through the use of ADA, accompanied by other markers, particularly the percentage of lymphocytes and other biochemical parameters. We would need to start by studying a larger number of samples in order to determine the most appropriate cut-off point in our health area. In our study, if we had used 40IU/l as the cut-off point, we would have missed two cases. Pleural fluids tend to be paucibacillary samples, and greater sensitivity would raise the limit of microbiological and molecular detection. In view of the fact that in most of the PF samples studied (74.5%) the ADA value was below 30IU/l, that alone would enable us to select the remaining 25.5% (with ADA >30IU/l) for application of the microbiological and/or molecular techniques, obtaining both a higher diagnostic yield and cost savings. Based on these preliminary results and in the absence of a more exhaustive study, we conclude that the use of molecular techniques for the detection of MT in PF with ADA values below 30IU/l does not appear to be reasonable in our area.
Please cite this article as: López-Medrano R, Fuster Foz C, Burgos Asurmendi I, Raya Fernández C. Uso de adenosin deaminasa como indicador para seleccionar líquidos pleurales para cultivo y/o técnicas moleculares para detección de micobacterias. Enferm Infecc Microbiol Clin. 2019;37:208–209.