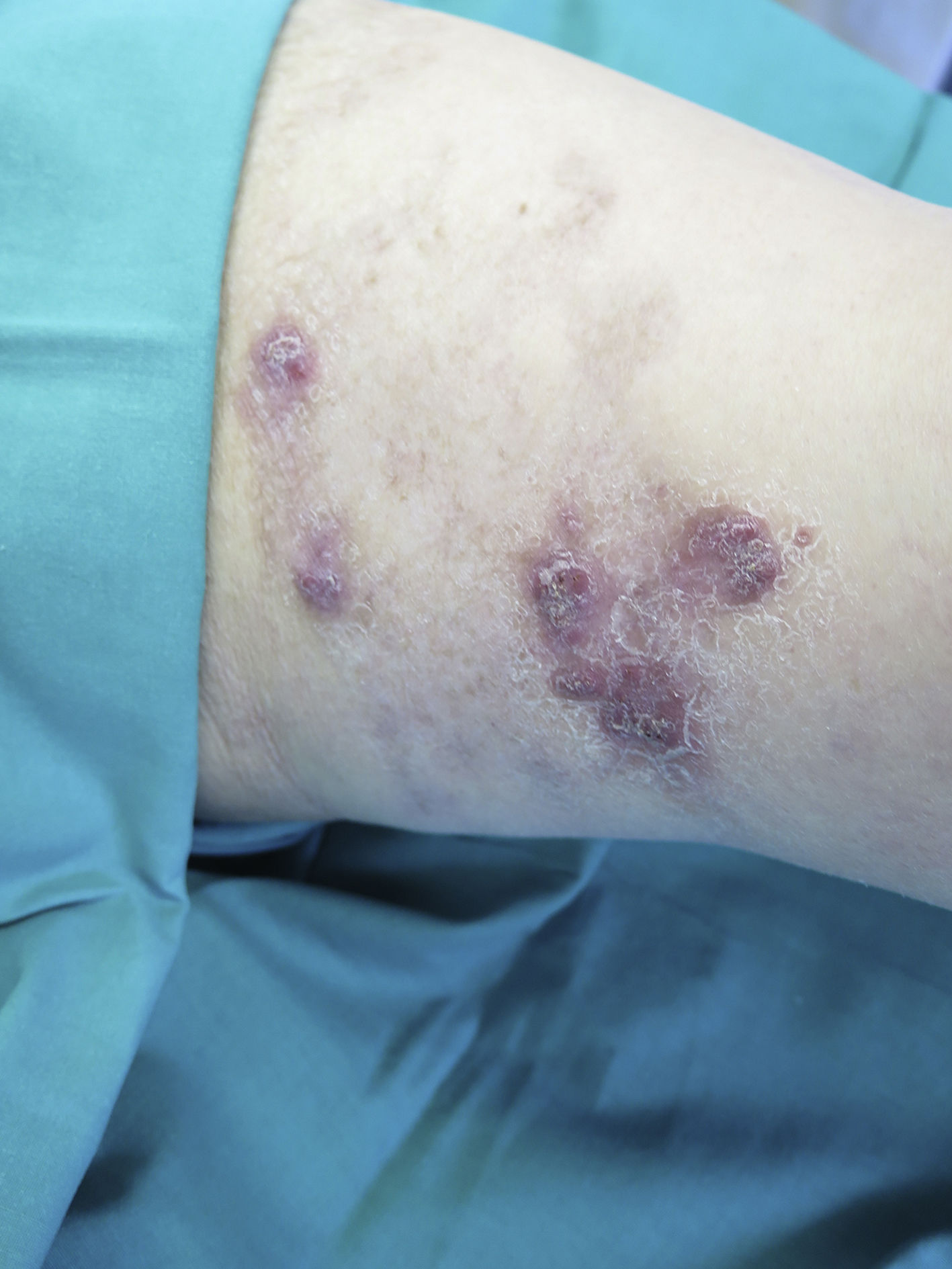
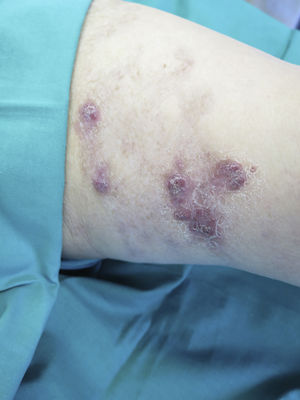
An 89-year-old woman visited the dermatology clinic, having been “forced” by her granddaughter, due to a lesion on her left thigh which had been present for years (the patient reported that she had had the lesion her entire life, since during the war “the Italians treated it”). An examination revealed an extensive plaque on the dorsal and inner lateral aspects of the left thigh with areas featuring a scarred appearance combined with areas with infiltrated and erythematous nodular lesions (Fig. 1). She reported no other symptoms such as fever, chills, cough or shortness of breath. A punch biopsy of the lesion was done and sent to pathology and microbiology for culture.
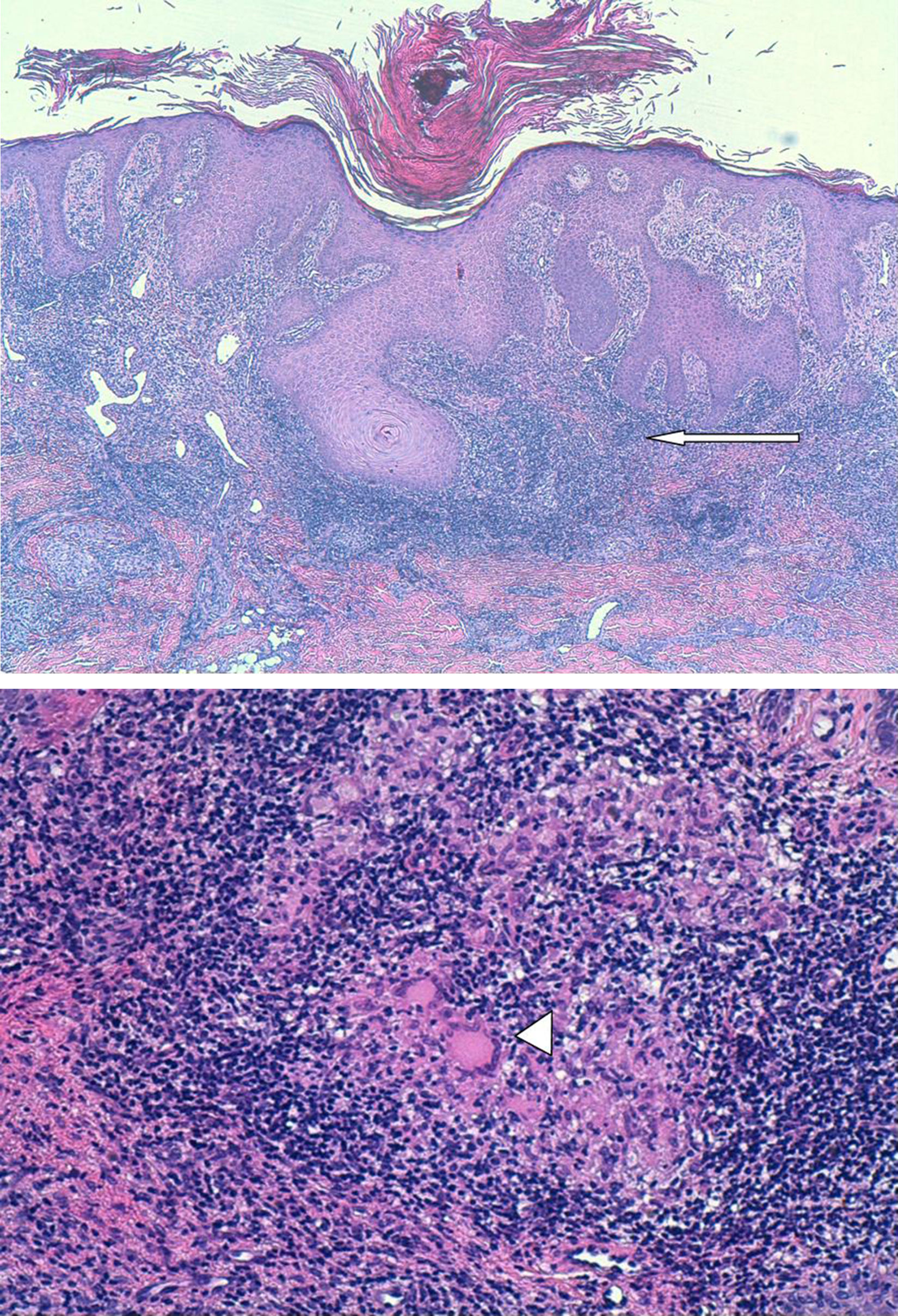
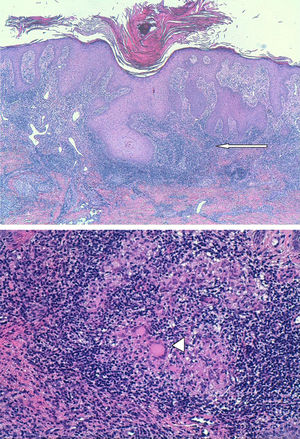
Clinical courseThe pathology report indicated that the biopsied tissue exhibited pseudoepitheliomatous squamous hyperplasia. The superficial and medial dermis showed a dense lymphocytic inflammatory infiltrate with the formation of frequent granulomas consisting of histiocytes and Langhans multinucleated and foreign-body giant cells surrounded by a crown of lymphocytes. No central necrosis thereof was seen (Fig. 2). The primary diagnosis was non-necrotising granulomatous dermatitis consistent, in its appropriate clinical context, with lupus vulgaris cutaneous tuberculosis (TB).
Punch biopsy with pseudoepitheliomatous squamous hyperplasia. A dense lymphocytic inflammatory infiltrate is observed in the superficial and medial dermis with the formation of frequent granulomas (arrow) consisting of histiocytes and Langhans multinucleated and foreign-body giant cells which are surrounded by a crown of lymphocytes (tip of arrow). No central necrosis thereof was seen.
In the microbiological culture, a mycobacterium grew that was identified as Mycobacterium tuberculosis complex sensitive to rifampin, isoniazid, streptomycin, pyrazinamide and ethambutol. In addition, at the same time, a sample of whole blood was sent for QuantiFERON® determination; the result was positive.
The patient was referred to the infectious diseases clinic to complete the study. A chest X-ray was taken in which lesions consistent with recent TB were ruled out. The patient declined to start treatment for tuberculosis given how old she was and how long she had had the lesion. Her family was informed and accepted her decision.
Final comments/discussionMycobacteria, the agents causing TB, are intracellular pathogens which have developed this strategy to escape damage by serum antibodies and which granulocytes cannot eliminate.1 TB is a disease that has been known since ancient times. It has been one of the primary infectious problems for human beings, has had devastating morbidity and mortality rates, and remains a global health problem.2 At present, it has gained significance due to the HIV pandemic, the growing number of people on immunosuppressive treatment for various reasons, immigration and the emergence of multi-drug-resistant strains.3
Cutaneous TB is a disease with a low incidence, representing just 1–4% of extra-pulmonary forms of TB.4 It accounts for a small proportion of all cases of TB, 1–2%,5 but in countries with a high prevalence of the disease, the number of cases is gaining significance. Its frequency is linked in 28% of cases to systemic TB and is very strongly linked to pulmonary TB in particular.6
Cutaneous TB may be classified as one of several different forms7:
- -
Primary TB, which includes the cutaneous primary complex and TB subsequent to BCG.
- -
Post-primary TB types: miliary disseminated, cutis orificialis or tuberculous ulcer, cutis colliquativa or scrofuloderma, lupus vulgaris and verrucosa cutis.
- -
Tuberculids, which may be papulo-necrotic, nodular, erythema induratum of Bazin, tuberculous erythema nodosum or lichen scrofulosorum.
Scrofuloderma and lupus vulgaris are the 2 most common forms.6
Lupus vulgaris is a chronic, progressive form of cutaneous TB that presents in previously sensitised patients. It is clinically characterised by brownish asymptomatic erythematous plaques most commonly located on the face. One prominent characteristic is the presence of tuberculoid granulomas, usually in the upper dermis, consisting of epithelioid cells, Langhans multinucleated giant cells, mononuclear cells and lymphocytes in the peripheral area.6,8
For treatment, the same treatment regimens as for pulmonary TB are recommended. Therapy with multiple drugs (at least 3) is pursued to decrease the possibility of resistance. It is also important to take non-pharmacological measures such as patient isolation to prevent spread and contagion.9
Notably, the patient's condition progressed for years without her seeking the care of a medical specialist. Other authors have reported similar situations. This may be due to the fact that the slow progression of lesions plus the absence of other symptoms do not provoke alarm in patients.10
Please cite this article as: Morilla Morales E, Morales Callaghan A, Vicente Arregui S, Viñuelas Bayón J. Lesiones cutáneas de muy larga evolución. Enferm Infecc Microbiol Clin. 2019;37:135–136.