This study aims to determine the effectiveness of combining acceptance and commitment therapy with family psycho education on increased insight, diminished symptoms, and the client's improved ability to control violent behavior.
MethodThe design of this study was a quasi-experimental pretest-posttest utilizing intervention and control groups. The intervention group consisted of 33 people, and the control group was composed of 33 people. Data was collected before and after respondents received both acceptance and commitment therapy and family psycho education.
ResultsThe study showed that patient insight improved significantly, the signs and symptoms of violent behavior decreased, and the client's ability to control such behavior improved with a p value < 0.05 in the intervention group after they received acceptance and commitment therapy and family psycho education. In the control group, patient insight did not improved significantly, showing a p value > 0.05. Therefore, our study recommends that acceptance and commitment therapy and family psycho education should be given to patients with schizophrenia to improve insight into their disease, decrease signs and symptoms of violent behavior and improve their ability to control violent behavior.
Schizophrenia is a severe mental disorder. The prevalence of schizophrenia is high, with approximately 24 million people worldwide suffering from the disease1. In Indonesia, it is found that 1.7 people per mile are diagnosed with schizophrenia2. While the causes of the disorder are not exactly known, factors believed to contribute to the incidence of it include abnormal neurotransmitter activity in the brain, a brain virus infection3, or genetic factors4. Scientists believe that environmental and behavioral factors may also increase one's chances of developing schizophrenia.
Symptoms of poor insight into one's illness and violent behavior are dominant characteristics of patients with schizophrenia. The majority of patient swith schizophrenia had poor insight5.The Mental Hospital of Malang states that 92% of their patients diagnosed with schizophrenia experience poor insight6. Further, studies have found that 8.4% of patients with schizophrenia display violent behavior7.
Both of these symptoms significantly impact a patient's quality of life. Poor insight into the disease results in a decrease of cognitive abilities, causing patients to reject their diagnosis since they are not aware of the signs and symptoms of the disease that they display. Patients who display this rejection typically do poorly in treatment programs, increasing their risk of recurrence and diminishing their quality of life9. Violent behavior brought on by schizophrenia often results in clients injuring or even killing themselves and others10.
Efforts to treat schizophrenia typically include treatment and care. The administration of either typical or atypical antipsychotic group therapy is not able to increase patient insight or decrease positive and negative symptoms in those diagnosed with schizophrenia11. This difficulty is partly because patients often exhibit non-compliance in taking their medication, requiring nursing actions to help maximize the function of medicine.
This research was conducted at the Soeprapto Psychiatric Hospital of Bengkulu Province, a facility at which the prevalence of clients with schizophrenia who experience violent behavior has increased from year to year. The Soeprapto Psychiatric Hospital's 2014 records showed that out of 1663 patients diagnosed with schizophrenia, as many as 1247 (75%) had poor insight into their disease and 1080 (65%) exhibited violent behavior12. A combination of acceptance and commitment therapy and family psycho education was administered to patients with schizophrenia to improve insight, decrease signs and symptoms of violent behavior, and increase the patient's ability to control such behavior.
MethodThis study used quantitative methods with the design of a quasi-experimental pretest-posttest with a control group. The study involved 66 respondents without randomization who were selected by accidental sampling. Measurements were performed twice on the respondents; the pre-test was performed before respondents were given acceptance and commitment therapy and family psycho education, and the posttest was given after respondents are given acceptance and commitments therapy and family psycho education. The samples in this study were patients with schizophrenia who have displayed violent behavior and were being treated at the Soeprapto Psychiatric Hospital in Bengkulu province at the time of the study.
The instrument used in this study was a questionnaire taken from the Birchwood Insight Scale that was translated into Bahasa Indonesia and tested for validity with the value of r results of < r table (0.396). The reliability test showed a value of 0.876. Questionnaires designed to measure signs of violent behavior in patients and their ability to control that behavior were developed by the Department of Mental Nursing at the Universitas Indonesia in 2014 and used in this study. The validity of signs and symptoms of violent behavior in the cognitive, affective, physiological, behavioral and social aspects of each component had a value of r results < r table (0.396). The reliability test showed that the value of symptoms in each area varied slightly: cognitive=0.908, affective=0.882, physiological=0.925, behavioral=0.923 and social=0.788. The validity test regarding the patient's ability to control his or her violent behavior had a value of r results < r table (0.396). The reliability test showed that value to be 0.895.
In the intervention group, patients were given acceptance and commitment therapy for two sessions, each lasting 45-60 minutes, and the patients’ families were given psycho family education for three sessions, each lasting 45-60 minutes. In the control group, patients were enrolled in a patient education program only. The data was collected and analyzed using a computerized program. Data collection was done after the researcher offered a detailed explanation of the study's procedures to the Soeprapto Psychiatric Hospital's staff and prospective respondents. Research was undertaken only after respondents agreed to participate in the study and gave their informed consent. Furthermore, the proposal of this study was validated by the Ethics Committee of Faculty of Nursing, Universitas Indonesia.
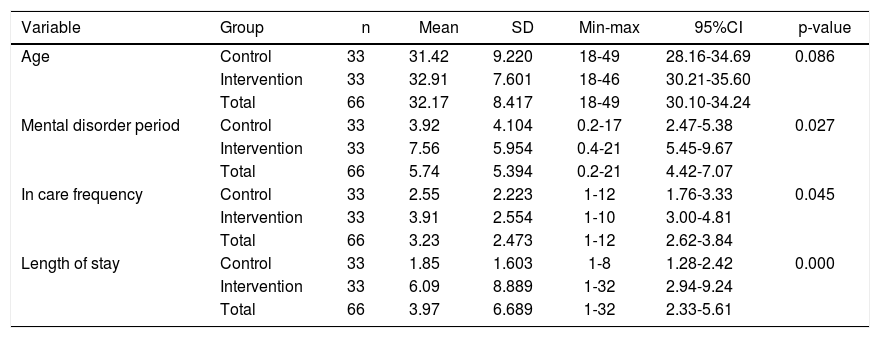
ResultsCharacteristics of patientsThe results of this study showed the value of central tendency on the variables of age, sex, length experience of mental illness, frequency of hospitalizations, and current length of stay before getting therapy (Table 1). The average age of patients participating in the study was 32.17 years, with the youngest being18 and the oldest being 49 years of age. The average length that respondents had been experiencing mental illness was 5.74 years, ranging from 0.2 years (6 months) to 21 years. Among participants, the average frequency of hospitalization was 3.23 times, with respondents experiencing from 1 to 12 hospitalizations in their lifetimes. The test results showed that variables of age, mental disorder period, and hospitalization frequency between the intervention and control groups were similar with p value > 0.05. The average length of stay when the therapy was given was 3.97 weeks with a minimum stay of 1 week and a maximum stay of 32 weeks. The results showed that the lengths of stay between the intervention and control groups were not similar with p value < 0.05.
Characteristics of treated clients with violent behavior in inpatient room of Soeprapto Psychiatric Hospital in Bengkulu Province (n=66).
| Variable | Group | n | Mean | SD | Min-max | 95%CI | p-value |
|---|---|---|---|---|---|---|---|
| Age | Control | 33 | 31.42 | 9.220 | 18-49 | 28.16-34.69 | 0.086 |
| Intervention | 33 | 32.91 | 7.601 | 18-46 | 30.21-35.60 | ||
| Total | 66 | 32.17 | 8.417 | 18-49 | 30.10-34.24 | ||
| Mental disorder period | Control | 33 | 3.92 | 4.104 | 0.2-17 | 2.47-5.38 | 0.027 |
| Intervention | 33 | 7.56 | 5.954 | 0.4-21 | 5.45-9.67 | ||
| Total | 66 | 5.74 | 5.394 | 0.2-21 | 4.42-7.07 | ||
| In care frequency | Control | 33 | 2.55 | 2.223 | 1-12 | 1.76-3.33 | 0.045 |
| Intervention | 33 | 3.91 | 2.554 | 1-10 | 3.00-4.81 | ||
| Total | 66 | 3.23 | 2.473 | 1-12 | 2.62-3.84 | ||
| Length of stay | Control | 33 | 1.85 | 1.603 | 1-8 | 1.28-2.42 | 0.000 |
| Intervention | 33 | 6.09 | 8.889 | 1-32 | 2.94-9.24 | ||
| Total | 66 | 3.97 | 6.689 | 1-32 | 2.33-5.61 |
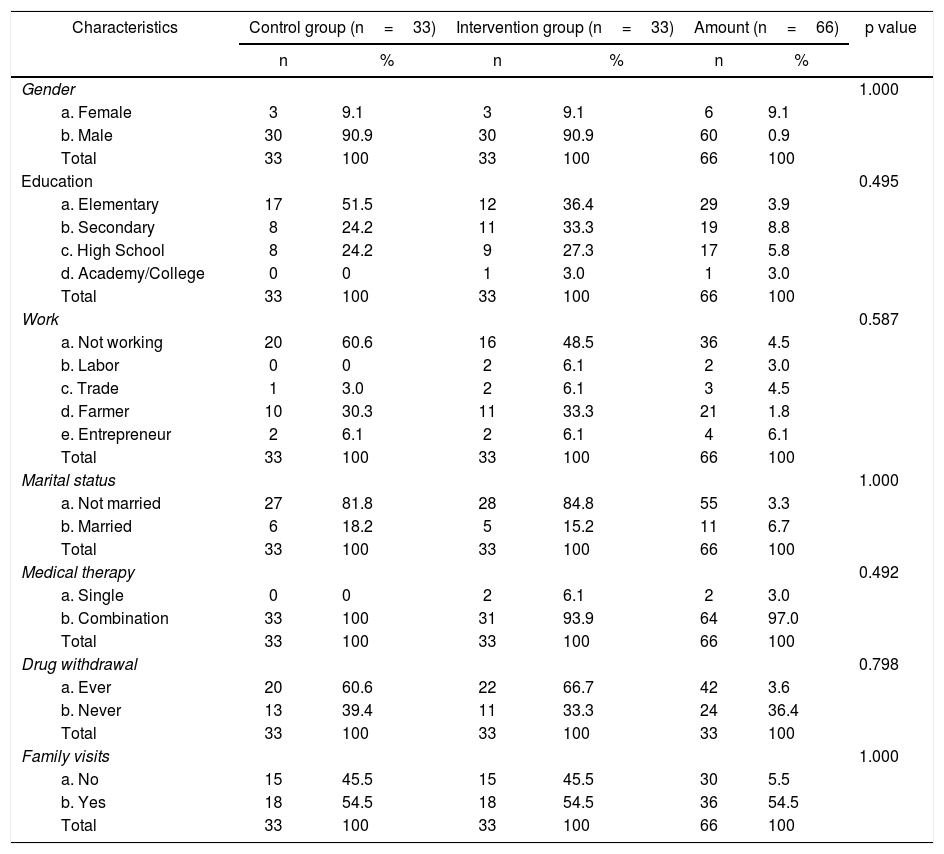
The results of the study also showed a data distribution of the variables of sex, education, occupation, marital status, medical therapy, drug withdrawal and family visit history (Table 2). Males made up 60, or 90.9%, of the study's participants, and 29, or 43.9%, of respondents stated that their highest level of education was the primary or elementary level. Most of the patients studied were not working, with 36 (54.5%) of participants claiming to be unemployed. Fiftyfive patients, or 83.3% of respondents, were single and, as many as 64 people, or 97% of participants, accepted a combination of medical therapies. A history of drug withdrawal was experienced by 42 people, while a history of family visits during the process of hospital care was experienced by 36 people (54.5%).
The characteristics of treated clients with violent behavior in inpatient room of Soeprapto Psychiatric Hospital, Bengkulu Province (n=66).
| Characteristics | Control group (n=33) | Intervention group (n=33) | Amount (n=66) | p value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender | 1.000 | ||||||
| a. Female | 3 | 9.1 | 3 | 9.1 | 6 | 9.1 | |
| b. Male | 30 | 90.9 | 30 | 90.9 | 60 | 0.9 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
| Education | 0.495 | ||||||
| a. Elementary | 17 | 51.5 | 12 | 36.4 | 29 | 3.9 | |
| b. Secondary | 8 | 24.2 | 11 | 33.3 | 19 | 8.8 | |
| c. High School | 8 | 24.2 | 9 | 27.3 | 17 | 5.8 | |
| d. Academy/College | 0 | 0 | 1 | 3.0 | 1 | 3.0 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
| Work | 0.587 | ||||||
| a. Not working | 20 | 60.6 | 16 | 48.5 | 36 | 4.5 | |
| b. Labor | 0 | 0 | 2 | 6.1 | 2 | 3.0 | |
| c. Trade | 1 | 3.0 | 2 | 6.1 | 3 | 4.5 | |
| d. Farmer | 10 | 30.3 | 11 | 33.3 | 21 | 1.8 | |
| e. Entrepreneur | 2 | 6.1 | 2 | 6.1 | 4 | 6.1 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
| Marital status | 1.000 | ||||||
| a. Not married | 27 | 81.8 | 28 | 84.8 | 55 | 3.3 | |
| b. Married | 6 | 18.2 | 5 | 15.2 | 11 | 6.7 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
| Medical therapy | 0.492 | ||||||
| a. Single | 0 | 0 | 2 | 6.1 | 2 | 3.0 | |
| b. Combination | 33 | 100 | 31 | 93.9 | 64 | 97.0 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
| Drug withdrawal | 0.798 | ||||||
| a. Ever | 20 | 60.6 | 22 | 66.7 | 42 | 3.6 | |
| b. Never | 13 | 39.4 | 11 | 33.3 | 24 | 36.4 | |
| Total | 33 | 100 | 33 | 100 | 33 | 100 | |
| Family visits | 1.000 | ||||||
| a. No | 15 | 45.5 | 15 | 45.5 | 30 | 5.5 | |
| b. Yes | 18 | 54.5 | 18 | 54.5 | 36 | 54.5 | |
| Total | 33 | 100 | 33 | 100 | 66 | 100 | |
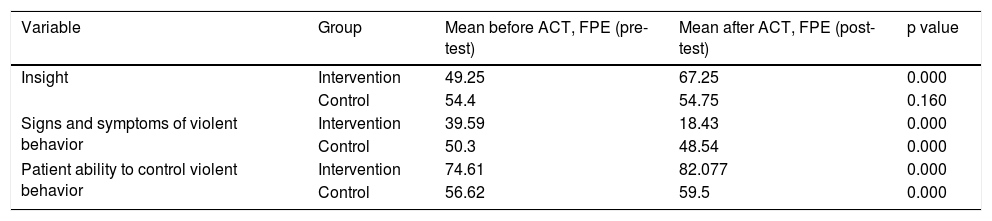
Changes observed in patient insight, signs and symptoms of violent behavior, and patients’ ability to control violent behavior before and after being given acceptance and commitment therapy and family psycho education can be seen in Table 3. In the intervention group, patient insight grew from 49.25% before acceptance and commitments therapy and family psycho education was given to 67.25% after such treatment. Signs and symptoms of violent behavior prior to therapy was 39.59% and decreased to 18.43% after therapy. The patient's ability to control his or her violent behavior prior to acceptance and commitment therapy and family psycho education was74.61% and increased to 82.077% after therapy. The results of the analysis clearly show significant improvement in patients after acceptance and commitment therapy and family psycho education were given to the intervention group (p value < 0.05).
Changes ininsight, signs and symptoms of violent behavior, and patientability to control violence before and after being given acceptance and commitment therapy (ACT) and family psycho education (FPE) in the intervention and the control groups (n=33).
| Variable | Group | Mean before ACT, FPE (pre-test) | Mean after ACT, FPE (post-test) | p value |
|---|---|---|---|---|
| Insight | Intervention | 49.25 | 67.25 | 0.000 |
| Control | 54.4 | 54.75 | 0.160 | |
| Signs and symptoms of violent behavior | Intervention | 39.59 | 18.43 | 0.000 |
| Control | 50.3 | 48.54 | 0.000 | |
| Patient ability to control violent behavior | Intervention | 74.61 | 82.077 | 0.000 |
| Control | 56.62 | 59.5 | 0.000 |
The average age of patients participating in this study was 32.17 years, and the average age at diagnosis was 38 years old4. We found that respondents in this study experienced schizophrenia for an average of 5.74 years. The period of clients experiencing mental disorders is 11.22 weeks13. The average frequency of clients treated at the psychiatric hospital is 3.23 times while a study shows the average frequency of clients treated at Mental Hospital is 4.37 times6. Previous studies shows certain characteristics of clients with schizophrenia: have low and middle educational background (60%)14, do not (64%)8, and are not married (70)%14. The study showed that 97% of patients with schizophrenia receive atypical and antipsychotic typical drugs, while as much as 6% of patients continued to receive a combination of typical and atypical antipsychotics drugs13.
The effectiveness of acceptance and commitment therapy and family psycho education on insightAs we have seen, patient insight in the intervention group increased after receiving acceptance and commitment therapy and family psycho education, rising from 49.25% to 67.25%. Many unpleasant incidents related to a schizophrenia diagnosis were reported by patients involved in this study; such experiences included being restrained or isolated, confined at home, handcuffed, abandoned, abused by a family member, and neglected by family while hospitalized. Patients also reported past suicide attempts, drug withdrawals, and drug relapses directly or indirectly caused by their schizophrenia diagnoses. These traumatic events create feelings of depression, anger, and isolation in patients, resulting in rebellious behavior like tantrums and the refusal to take prescribed psychiatric medication. Many patients also reported feelings of powerlessness regarding the treatment they receive. In acceptance and commitment therapy, therapists help patients understand that family members often behave out of fear or frustration regarding the patient's disease; the therapy ultimately reinforces the value of family for the patient by exploring relatives’ inadvertently hurtful behavior. Therefore, we saw an improvement in patient insight after acceptance and commitment therapy wasadministered15. Acceptance commitment therapy helped patients’ better deal with unpleasant events, increase psychological flexibility, and make a commitment to overcome problems encountered while establishing new good behaviors16. This process also improved how patients rated themselves so that they were slowly able to create new behaviors in an effort to improve themselves and their abilities to resolve the problems encountered.
Poor patient insight inhibits management of schizophrenia9. Patients who received acceptance and commitment therapy experienced a significant decrease in the severity of psychiatric symptoms, improved quality of life, and betterment in the self-awareness component17. The combination of ACT (Acceptance and Commitment Therapy) and Family Psycho Education (FPE) for patients with violent behavior aims to train clients to stop releasing or nurturing anger that makes them feel inferior in their daily routines18.
The effectiveness of acceptance and commitment therapy and family psycho education on the signs and symptoms of violent behaviorSigns and symptoms of violent behavior decreased from 39.59%to 18.43% after patients received acceptance and commitment therapy and family psycho education. Family stands as one of the most important factors in providing support to patients with schizophrenia. Additionally, most families desire to support a relative with schizophrenia, though they often feel that they lack knowledge of the disease and how to care for those suffering from it. Most families expressed confusion regarding the diagnosis and care of those with the disease and report bringing afflicted relatives to the hospital only after alternative and traditional medicine has failed. The resulting delay of medical treatment for the patient aggravates symptoms of the disease. Therefore, knowledge is a key in helping patients avoid misguided treatment by their own families.
Family psycho education seeks to change a family's way of dealing with a relative who suffers from schizophrenia. Therapists teach families that patients are not to blame for their disease and help the family understand signs of relapse so that the patient's illness can be better controlled19. Family psycho education can effectively lower the frustration of family members when caringpatients20. An increase in the family's knowledge and understanding of the disease and diagnosis will improve their ability to care for patients, increasing his or her quality of life and raising the standard of his or her care by family. The decrease in frustration and violent behavior directed at patients by family members will significantly reduce resulting violent behavior shown on the patient's part.
The effectiveness of acceptance and commitment therapy and family psycho education on patient ability to control violent behaviorThe patient's ability to control violent behavior in the intervention group increased from 74.61% to 82.077% after the administration of ACT and FPE. Family psycho education was seen to positively impact both on families and patients21. Benefits obtained by patients included getting optimal care from family members, improved treatment adherence by patients, and improved patient mental status. The study found that while positive signs and symptoms seen in patients did not directly increase the burden on family members, a patient's negative signs and symptoms directly impacted families by increasing patient dependency. This dependency resulted in a disruption in family economic circumstances, changes in habits, and a decrease in social functions22. Therefore, adequate information is required in order for a patient's family to adequately cope with the burdens experienced by caregivers.
Acceptance and commitment therapy accommodated cognitive and behavioral changes for patients. These changes occurred through recognizing unpleasant incidents which have been experienced and finding the values of such unpleasant associated event. Patients then chose which value was good and not, decided on actions for good and bad values, chose which values to take, and made a commitment to change and become better.
Based on the discussion above, the researcher concludes that the acceptance and commitments therapy and family psycho education effectively improve insight, lower the signs and symptoms of violent behavior and improve the client's ability to control violent behavior. Suggestions that can be submitted through this study is that the acceptance and commitments therapy and family psycho education can be used as choice to overcome insight and violent behavior in schizophrenia clients.
Thanks are given to the Suprapto Psychiatric Hospital in Bengkulu Province for the assistance in this study, to the patients and families who have been willing to become respon-dents in this study, and to DRPM of the Universitas Indonesia who have provided financial assistance to conduct this study.