Indonesia Medika has established “Garbage Clinical Insurance” (GCI), which enables the population below the poverty line (BPL) to obtain health insurance by donating their garbage to pay the premium. The objective of this paper was to critically examine the implementation of GCI in Indonesia by reviewing the background, effects, and sustainability of this program.
MethodA literature search of studies related to GCI, other types of micro health insurance, and their applications in developing countries was conducted. Recent news (post 2014) related with the implementation of GCI was also consulted.
ResultsThe literature revealed that the foundation of GCI was informed by the Declaration of Alma Ata with the ideal of making health care services accessible to everyone. Unlike most health insurance, the mechanisms of GCI seem less likely to trigger moral hazard among its beneficiaries. However, as a micro insurance program, the sustainability of GCI continues to be called into question.
ConclusionsThe critical analysis of the present study has highlighted the application of GCI, a micro health insurance initiative, and its relevance to Indonesia. GCI tended to work well as it was able to utilise Indonesia's social capital. However, GCI should aim to increase the benefits package available to its members in order to maintain the sustainability of the program
The health system in Indonesia has been rapidly changing over the last two decades, especially after the 1997 economic crisis, which was followed by a political crisis one year later in 1998. These events caused health services to be unaffordable for the Indonesian population living below the poverty line (BPL)1. To tackle this problem, the government tried to reduce the prices of medical services at point of use in order to improve access to health services and also to restructure the health care financing system by implementing social health insurance2. Many recent studies from developing countries have indicated that the expansion of health insurance has had a positive impact on the utilization of health care services3–5. In Indonesia, the government rolled out social health insurance for the BPL population (namely Askeskin) in 20052,6. However, in January 2014, a new type of contributory-public insurance, called the Government Public Health Insurance (BPJS, labeled as such for the corresponding government department in Indonesia) was launched, which covered the general Indonesian population7. However, the sustainability of BPJS has become a concern due to to the limited funds available to support and maintain this program8. Moreover, unlike Askeskin, to be covered by BPJS, residents have to pay a premium starting from Indonesian Rupiahs (IDR) 25,000 (U.S. dollars [USD] 2) per month, which is still too high for the BPL population who live with less than USD 1.25 a day to afford9. Thus, the need for micro health insurance (MHI) in Indonesia cannot be denied, and Indonesia Medika (IM), one of the “healthpreneur organizations” in Indonesia, has established a new MHI scheme called “Garbage Clinical Insurance” (GCI). GCI enables the BPL population to obtain health insurance by donating their garbage to pay the premium10. Therefore, the object of this paper is to critically examine the implementation of this local program in Indonesia.
MethodThe present study was designed as a literature review. This study aimed to critically analyze the implementation of a health improvement program in Indonesia: Garbage Clinical Insurance. A literature search was conducted using five databases: ProQuest, Science Direct, SpringerLink JSTOR, and Scopus.
In order to retrieve relevant articles, the period for the literature search on this topic was delimited from the January 2000 to April 2015. The author decided to start the search in 2000 because a number of studies on the implementation of micro health insurance in other low- and middle-income countries were published in this year and the following years. The selection was limited to the following inclusion criteria: a) articles focused on topics surrounding the implementation of micro health insurance in low- and middle-income countries; b) articles published from 2000 to 2015; c) articles in the English language, and d) title and abstract of the articles mentioned “micro health insurance”.
ResultsThe findings of the literature review on the implementation of GCI in Indonesia were structured according to the main themes that were found with respect to the background, effects, and the sustainability of the program. Nevertheless, a brief explanation about neoliberalism and the healthcare situation in Indonesia will first be presented to provide a context for this study.
Neoliberalism and the healthcare situation in IndonesiaAfter the monetary crisis (krismon) in 1997, Indonesia had to accept a USD 43 billion bail-out from International Monetary Fund (IMF) and the World Bank (WB), which required Indonesia to adhere to Structural Adjustment Programmes (SAPs)11. The SAPs, which have been argued to be based on neoliberal economic principles12, primarily aim to reduce the role of the state and let the market flow naturally through the balancing effect of the price mechanism13. Reducing the role of the state has been translated as reducing the financial and managerial responsibilities of the central government for public goods, including health care, through decentralizing its roles at the district level and privatization1. The IMF and WB, as supranational organizations, have tended to believe that the private sector can produce and manage health care services more efficiently than government and can generate extra resources so that existing government resources can be redistributed to the urban and the rural poor13.
According to the World Bank14, Indonesia is a low-middle income country with a GDP of USD 868.3 billion and a total population of 249.9 million. About 18% of its inhabitants live on less than USD 1 per day, and about half live on less than USD 16.6 per month15. About 15 years after the implementation of SAPs, the economic growth of Indonesia has improved significantly, as shown by the increasing gross national income per capita from USD 2200 in the year 2000 to USD 3563 in 201215. In the area of health care, after the passage of Law No. 40 (2004) that ratified the National Social Security System, the government has shown a great concern for expanding health insurance coverage in Indonesia by promoting nationwide social health insurance6. In 2005, the government successfully provided health insurance for the poor and vulnerable groups (Askeskin) that was funded by the public budget16. Furthermore, in 2014, the government introduced the largest health insurance scheme in the world, offered by BPJS, to cover the total population of Indonesia by 20198.
However, there are many concerns about the sustainability of this scheme, especially with respect to the availability of funding. As the architect of the scheme, Thabrany, has stated: “This scheme is badly underfunded”8. Even though the government recently increased health spending, public health expenditure remains low at less than 3% of GDP, which is less than average in comparison to other countries17. Moreover, the premium for membership in the scheme starts at IDR 25,000 (USD 2) per month, which is still unaffordable for poor people in Indonesia9. Besides these challenges, collecting regular contributions from poor communities has been difficult because people living in these communities often perceive the payment of a premium as a loss, as they are paying for potential care that may not be necessary18.
Micro health insuranceMHI is a kind of low budget insurance that enables the poor to access health services without the threat of financial impoverishment18–20. According to Schneider19, the objective of MHI is to improve the access of its members to health care by lowering their out-of-pocket expenditures. A number of stakeholders are involved in MHI, such as clients, healthcare providers, regulators, insuring companies, and also Third Party Administrators (TPA), making MHI complex in comparison to other micro insurances21.
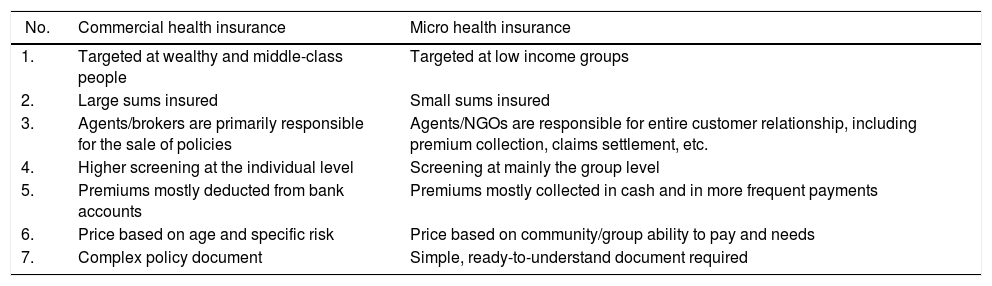
Differences between micro health insurance and commercial health insurance (Table 1)Despite the complexity of MHI in comparison to other micro insurances, MHI also offers several advantages, as described below:
- •
According to Ruchismita et al22, MHI enables low income groups to afford health services and also provides them with economic and social security by reducing expenditure shocks or dividing costs into smaller payments.
- •
MHI can increase the utilization of health services, as many empirical studies show that insured patients tend to use health services five times more in comparison to non-insured patients23.
- •
MHI makes health services more affordable through formulating cost effective-ways and more efficient ways to deliver health services18.
- •
MHI helps to improve the standardization of health services and to increase awareness among clients of healthrelated issues18.
Distinctions between commercial and micro health insurance.
| No. | Commercial health insurance | Micro health insurance |
|---|---|---|
| 1. | Targeted at wealthy and middle-class people | Targeted at low income groups |
| 2. | Large sums insured | Small sums insured |
| 3. | Agents/brokers are primarily responsible for the sale of policies | Agents/NGOs are responsible for entire customer relationship, including premium collection, claims settlement, etc. |
| 4. | Higher screening at the individual level | Screening at mainly the group level |
| 5. | Premiums mostly deducted from bank accounts | Premiums mostly collected in cash and in more frequent payments |
| 6. | Price based on age and specific risk | Price based on community/group ability to pay and needs |
| 7. | Complex policy document | Simple, ready-to-understand document required |
NGOs, non-governmental organizations.
GCI is a micro health insurance program established by a non-governmental organization (NGO) named Indonesia Medika9,24. The founder and also CEO of this organization is Gamal Albinsaid, who calls it a “healthpreneur organization”. He proposed the establishment of IM in 2013 to facilitate the creation of innovative programs to promote health care through the involvement of medical students and individuals who are concerned with public health9. The major program provided by this organization is GCI.
GCI is a micro-health insurance that uses garbage as a financial resource. In order to meet the premium, which is IDR 10,000 (USD 0.83) per month, members of this scheme must deposit their organic and non-organic waste at a GCI collection site every week in order to receive a card that guarantees them free access to a medical clinic8,24. Through this program, members can obtain free access to quality health services, including primary care at local clinics, family planning, in-school health advocacy, nutrition consultations, home visits for patients with chronic diseases, and even telemedicine with licensed doctors24.
To run this program, the collected garbage is recycled through two ways10. The founder further explained that the organic garbage is processed to be fertilizer and sold through a fertilizer salesman pivot system, while non-organic items are sold to the government-owned Malang Waste Bank. Afterward, the money is transferred into the health fund and given back to the GCI members in the form of holistic health care, including as primary care (curative), health improvement programs (health promotion), illness prevention programs (preventive), and rehabilitation programs10,24.
According to Albinsaid10, GCI has four standards of excellence. First, GCI promotes social entrepreneurship by facilitating an innovative solution for tackling social problems. In addition, the entire profit generated by the program is used to finance clinics and health programs for members. Second, this program uses garbage as the source of profits by building a system for the management of garbage in communities. This provides an effective solution for two problems by improving access to health care and also challenging the waste problem that is a frequent source of infection and disease in Indonesia, especially in poorer areas. Third, GCI utilizes a holistic health care system. Finally, this program is broadly accessible by the community since only garbage is used as the premium, making every family eligible to join.
In 2014, five clinics formed part of IM, with 300 to 500 members per clinic9,24. Four of them were located in Malang, while the other one was in a village outside the city limit. All clinics are open Monday to Saturday from 7 am to 9 pm and are operated by 88 volunteers and intern, 15 doctors, 12 nurses, and midwives9. Forty-seven staff members were paid based on standard payment in Indonesia from the profits generated by garbage collection24. Each member of GCI receives access to the clinic twice a month for premier treatment9. According to Albinsaid9, in limiting the access to health care to twice a month, he hopes to optimize health education, promotion, and prevention. So far, the system has been successful, as only 10 to 15 percent of people who bring in garbage use the service9. Thus, enough money is left over to run the centers and to fund their development. Although this program tries to provide holistic health care to its members, it does not include surgery or hospitalized treatment because they are too expensive to be covered.
In order to expand the impact of this project, GCI collaborates with four private clinics in Malang24. The clinics receive incentives to provide treatment to large numbers of GCI members and are paid per beneficiary treated. GCI pays IDR 15,000 to the clinic for one member for premier treatment and also covers prescribed medicine9. Through this collaboration, GCI makes health services more affordable for poor families and also funds small private clinics more than government public insurance. Moreover, people in the cities of Medan, Jakarta, Banjarmasin, Jember, Sidoarjo, Blitar, Denpasar, and Manado have replicated the GCI system via cooperation with private clinics9. In addition, GCI is also in the process of forming a collaboration with BPJS so that members can receive better health services that include surgery and hospital treatment. Meanwhile, this project can also serve as a model for other BPL communities and allow them to pay their BPJS premium through recycling their garbage.
DiscussionNeoliberal versus social capitalism and viability of health services for the poorNeoliberalism as an economic ideology has penetrated developing countries through the application of SAPs initiated by the IMF and the WB11. Indonesia, as one of many countries that has been prescribed by both the IMF and the WB to implemented SAPs, has shown economic growth by increasing its gross national income per capita from USD 2200 in the year 2000 to USD 3563 in 201215. However, neoliberal policies have caused lower income individuals to be left behind without adequate support from the government, thus disabling their ability to survive under free market conditions25. D’Ambruoso25 further argued that such conditions have created inequality to the extent that the BPL population is unable to afford public goods, including health care services. In the study of Kristiansen et al1, a significant decline in the use of public health services was identified in Indonesia after the implementation of decentralized and privatized programs. However, after the passage of Law No. 40 that ratified the National Social Security System in 2004, Indonesia has been developing an alternative to this neoliberal trend by introducing Askeskin, which provides health insurance coverage to the BPL population6.
By introducing Askeskin, which was then followed by the creation of BPJS, a nation-wide health insurance initiative, Indonesia has been showing a transition in its economic philosophy away from neoliberal capitalism and toward a more social capitalism. As a low middle-income country, in which more than 28 million people live below the poverty line15, social capitalism can be argued to be a more appropriate economic model for Indonesia. As an economic philosophy, social capitalism tends to provide more benefits for lower income individuals since, unlike neoliberal capitalism, in social capitalism the government is involved in helping BPL individuals raise their earning potential and living standards26. Thus, they will be more likely to survive in the free market economy. Meanwhile, the employment of social capitalism in the health sector now signifies that the government plays a significant role in running social programs, such as low-cost medical care and mandatory public health insur-ance schemes.
However, in Indonesia, the success of government efforts to enable wider access to health services for the BPL population is still arguably related to funding availability8. Therefore, more strategies need to be applied in order to bridge gaps in funding, such as empowering communities to work together in order to solve their health problems27, one of which is gaining open access to health care services. Eriksson26 further argued that in order to expand access collective social capital will be needed. Social capital is believed to have a positive, albeit indirect, effect on health through the development of communities and in this sense refers to “features of social organization, such as trust, norms, and networks; that can improve the efficiency of society by facilitating coordinated actions”28. Social capital has also been proposed as a missing link in the application of neoliberalism, as it can mediate some of the worst effects of neoliberalism and, at the same time, enable a society to take advantage of the economic opportunities that come from cohesive and stable social conditions29. Therefore, a project like GCI, with a community development approach, perhaps can be seen as a more effective way of tackling some, if not all, of the public health problems in Indonesia. The GCI program is supported under these principles, as it tends to make good use of social capital by ensuring broad participation from the community10.
Garbage Clinical Insurance based on the Declaration of Alma AtaDespite the prior decentralization and privatization of public health services in Indonesia, the nation's health system has become increasingly publicly focused and reportedly continues to be based on the principles and features of the Declaration of Alma Ata17. The paradigm of the Declaration of Alma Ata is “Health for All,” which is explained as universal access to public primary health care. As previously described, Indonesia's government currently provides two mandatory public health insurance schemes17: Askeskin and BPJS. The justification for introducing such mandatory schemes is to assure a more stable funding base for health care so that modern health services become, at least in theory, widely accessible13. Despite the government's effort to make public health services more accessible through mandatory public health insurance, more than 60% of Indonesia's population in 2007 remains uncovered6. Furthermore, half of health expenditure is private, mostly out of pocket, as nearly half of those who are ill are more likely to seek health services from private providers17.
Based on this context, the founder of IM, who believes that health care is a fundamental human right, has tried to bridge the gaps in care by introducing GCI24. According to Patel8, the GCI scheme expands access to health services and simultaneously represents a solution for the sanitation problem, as improper waste management is a frequent source of disease. In this sense, the CGI system has created a link between waste management, health insurance, and health care. In other words, this program uses the provision of primary health care (PHC) and the transformation of garbage to cover health insurance premiums as a foundation for organizing the health care system, thereby creating a link between improved sanitation, a healthier environment, and greater health8. Also, PHC involves numerous factors that play a role in health, providing health services in addition to preventative programs focused on lifestyle or the environment30. A primary care-based model is arguably the most effective and efficient way to manage a health system according to the stipulations of the Declaration of Alma Ata.
Does Garbage Clinical Insurance trigger moral hazard among its members?Some economists and policy analysts have argued that one of the central problems surrounding the provision of health insurance is moral hazard31. Moral hazard has been defined as the condition wherein people increase their demand for health services more than the optimal amount when they do not have to pay the full cost of the care but rather carry only a marginal cost burden32. In Indonesia, after the implementation of Askeskin, or insurance for poor and vulnerable groups with non-contributory premiums6, the health care utilization rates increased nearly 50% for outpatient and inpatient services33. This result appears to be consistent with the principles of moral hazard that Askeskin triggered “ex post moral hazard” following its implementation6.
However, Sihare et al32 argued that increasing demand on health services cannot be concluded as a moral hazard, particularly for people who live in chronic poverty. The real problem may be that they tend to neglect immediate treatment due to its high cost, which in the end leads to higher costs and longer or more serious illness. Sihare et al32 further argue greater provision of health care can represent a golden opportunity and one step in the right direction toward a healthier and more equitable world.
Based on Sihare et al32 explanation of health insurance and the moral hazard, the mechanism of GCI seems less likely to trigger its members to experience moral hazard. Unlike Askeskin, the members of GCI have to pay a premium each month in the form of a garbage donation, and their access to health services is also limited to twice a month9. Moreover, GCI health services are not only focused on PHC (curative) but also on preventive and rehabilitative care24. This program is thus consistent with Sihare et al32 argument that the inclusion of preventive care is covered in health care schemes can prevent moral hazard.
The Sustainability of Garbage Clinical InsuranceIn spite of extensive interest in expanding the principles of micro insurance programs, their sustainability continues to be questioned34, particularly their financial sustainability. For instance, the financial viability of MHI tends to depend on enrollment and the claim payment process35, and finding a sustainable business model appears to be an important prerequisite for organizations that choose to run this kind of program34. Otherwise, such organizations more likely to experience high loss ratios and high lapse rates in their early years that will decrease their credibility among the donors who subsidize their programs34.
GCI, as a micro health insurance initiative organized by an NGO, is, according to Bennett13, more likely to face problems of financial sustainability. To ensure its sustainability, GCI has prepared financial resources and also human resources and has even built a basis of structural and cultural support10. According to Albinsaid9, the organization and projects of IM are funded from prizes for social innovation, GCI premiums, and also non-member patients. So far, the founder of this project claims that the system has been successful, with only 10 to 15 percent of the members actually using the health services per month; as a result, more than enough money is left over to run the center and to fund its development. However, those members do not realize the benefits of their membership could appear to be an early warning, leading them to quit the scheme35. In addition, one of the intrinsic factors that can reduce the membership of any MHI initiative from the provider is offering an inadequate benefits package. As GCI does not cover surgery and hospital treatment, there is a possibility that the current members see the benefit package as inadequate and thus stop their membership. Therefore, the plan to merge GCI with BPJS appears to be an effective way to improve the benefits package of GCI, which is believed to help MHIs maintain their sustainability35.
Conclusions and recommendationsThe paper aimed to critically analyze the implementation of CGI in Indonesia by examining the background, effects, and sustainability of this program. Although the neoliberal economic model has led to the privatization of health care services in Indonesia, the Indonesian government has played a significant role in protecting the rights of the BPL population through efforts to introduce a nationwide health insurance scheme. In this article, an explanation of SAPs was presented in addition to how liberal economic principles have affected Indonesia and, in particular, how they have impinged upon the nation's health care system. A brief explanation was provided on the differences between micro health insurance and commercial health insurance in order to provide context for the application and the relevance of GCI, a micro health insurance initiative, in Indonesia. In addition, the implementation of GCI in Indonesia was discussed in detail. In the Indonesian context, GCI has worked well and has taken advantage of Indonesia's social capital, which is in line with the findings of Pargal et al36 that concluded that the introduction of public-private partnerships or self-help schemes are more likely to be successful in neighborhoods where the level of social capital is high. The foundation of GCI was informed by the Declaration of Alma Ata, whose ideal is to make health care services accessible to everyone. As an MHI, there are no indications that GCI will provoke a moral hazard among its members. This is notable considering that MHIs tend to cause a moral hazard when members do not contribute toward paying the premium. A consideration of the hazards that may be driven by MHI could help policy makers redesign the Government Public Health Insurance scheme, directed by BPJS, by adopting GCI's system. In addition, adopting or improving the GCI system may help the government create a better link between improved sanitation and health, which could serve as a stepping stone from solely curative practices to those of health promotion and prevention.