To review the effectiveness of a clinical care pathway on interprofessional collaboration and quality of health service.
MethodA review was performed of literature published from 2000 to 2015, with the following keywords: clinical pathway, care pathway, and interprofessional collaboration.
ResultsEvidence depicted the positive results of nursing care for clients, health care professionals and facilities. The research results were implemented at different facilities using several research designs, from descriptive to experimental. A clinical pathway was used as a tool in various clinical situations including in emergency, elective surgery, and pre-post-surgery, as well as in common clinical cases. It was administered by the health care professionals in providing care, encompassing the comprehensive process from diagnosis to clinical audit. Health care professionals should engage in active collaboration during the implementation of a clinical care pathway. In implementing the standard of input, process, and outcome of care to clients, health care professionals should emphasize the process and outcome of care and eliminate unnecessary or inefficient treatments.
ConclusionsA clinical care pathway could reduce the average length of stay for patients, increase cost effectiveness, and, consequently, improve the quality of service. To optimize the care process, the pathway should be implemented of multidisciplinary health care team.
Health care services must be continuously improved in terms of quality and cost effectiveness. The quality, efficiency, and accessibility of health care services is one of the research priorities in health care management1. Hospitals commonly skip giving thorough and evidence-based information regarding treatments to patients and their families because the patients response is different2.
A clinical pathway is a strategy to support evidence-based practice and is efficient to guide the implementation clinical treatment for various patient conditions. It comprises the algorithms which are illustrated by flow charts, a set of decisions, and complete treatment3,4 aimed at an optimal treatment process through systematic and timely interprofessional decision-making and interventions5. A clinical pathway is a strategy to improve collaboration between physicians, case managers, nurses, pharmacists, physiotherapists, and other health professionals6.
It is necessary to discern to what extent a clinical pathway affects the collaboration between health care professionals and the quality of health care services. Therefore, in this paper, we present our findings based on a review of literature related to clinical pathways.
MethodLiterature relevant to clinical pathways published from 2000 to 2015 was reviewed. Articles were searched through electronic databases, including Medline, Clinical of Nursing, Advanced Nursing, Elsevier, BMC Medicine, Implementation Science, Trials, and EMA. We used the following search terms: clinical pathways, care pathways, and interprofessional collaboration. Articles were collected and selected according to predetermined keywords, without restriction on the study method of the articles. The review included the title, abstract, research objectives, research methods, instruments used, and research results7.
The selected literature consisted of original articles from countries in Asia, Europe, and the USA. These articles consisted of quantitative and qualitative research related to clinical pathways, care pathways, and interprofessional collaboration to improve the quality of service. Research was carried out in health facilities, and study designs comprised the following: cluster randomized clinical trials (cRCT), quasi-experimental, cohort, case-control, case studies, and focus group discussions.
ResultsA total of 44 articles were obtained from the search. Of these, 20 articles were excluded as they did not meet the criteria of the original paper. We finally reviewed 24 articles with the following designs: 4 cluster randomized clinical trial (cRCT), 6 quasi-experiments, 6 cohorts, 1 case-control, 4 case studies, 1 interview, and 2 focus group discussions.
The quantitative samples of the reviewed articles covered of a variety of clinical conditions: pneumonia, heart disease, chronic obstructive pulmonary disease, and post-surgery. The reviewed articles also reported response on health care team related to clinical pathway. The articles were categorized into interprofessional collaboration and clinical care pathways.
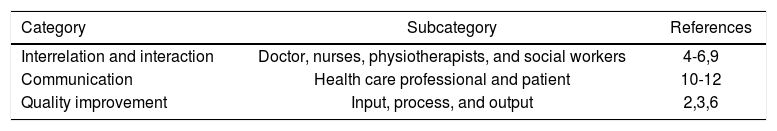
Interprofessional collaborationInterprofessional collaboration is the service provided by a team of different health care professionals and is essential to ensure effective clinical treatment8. The health care team performs interrelation and interaction throughout the input, process, and output of patient care6. Members actively collaborate in implementing comprehensive nursing care. The process involves multidisciplinary interventions with a focus on predetermined outcomes9.
Patients as a service centered care should be elaborated in the implementation of the nursing process to boost patient recovery and to improve efficiency and service quality10. The key to successful interprofessional collaboration is communication, which should be carried out continuously between the health care team and the patient. Patient satisfaction is an indicator of the success of the interprofessional collaboration. The health care team should have the same perception of the quality of service11 (Table 1).
Clinical care pathwayA search for “clinical pathway” turned up many terms in the collated published literature: clinical pathway, care pathway, integrated clinical pathway, integrated care pathway, and wellness pathway. Evidence-based clinical pathway could be defined as a strategy4, standard, diagnosis, and procedure for health personnel when performing comprehensive patient care13.
A clinical pathway can be used in all types of clinical settings, ranging from emergency, elective surgery, pre- and post-surgery, or general health facilities. It can identify the condition of the patient at the hospital, clinic, or the patient's home. A clinical pathway is a standard of care delivery that begins with assessment, diagnosis, information support, rehabilitation, and clinical audit13. The pathway can also help to identify the critical components impeding patient care or supporting facilities3.
A clinical pathway provides detailed instructions for each part of patient management according to the specific condition within a certain period, patient progress, and the expected outcome. The pathway generally describes the types of clinical treatment based on patient needs, in the form of algorithms for planning and systematic management of patients with specific diseases and diagnoses14. The flow of the clinical pathway must be brief and concise to guide all health professionals in care delivery. Nurses play an important role in comprehensive patient care by conducting nursing assessment, monitoring, intervention, evaluation, and rehabilitation10,15.
In one study we reviewed, a clinical pathway was used in thrombolytic treatment for patients with acute myocardial infarction (AMI) in rural areas. The AMI mortality rate in rural areas is remarkably high since the administration of thrombolytic therapy is not considered the emergency treatment. Clinical pathway administration of thrombolytic therapy is the best practice for patients with AMI, leading to better and timely outcomes, thereby reducing mortality4.
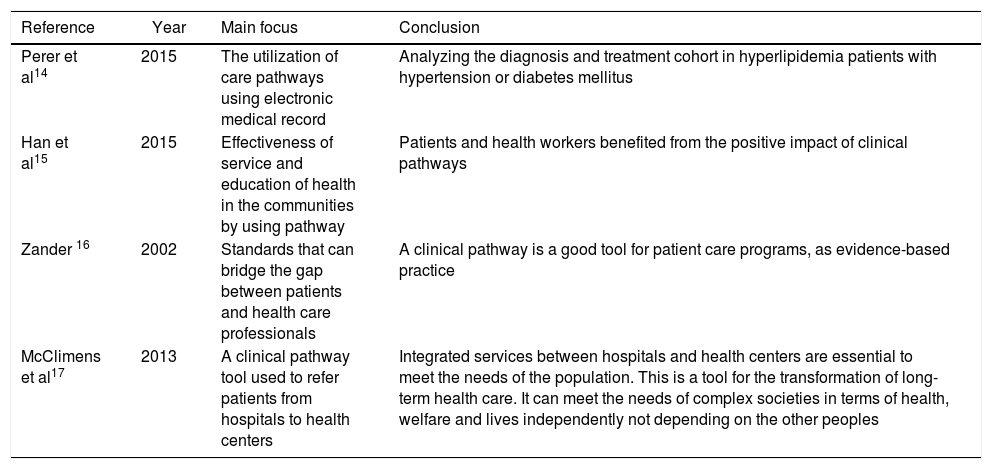
Another study assessed the implementation of clinical pathway for patients with multi-system disorders such as paraplegia and tetraplegia. Paraplegia and tetraplegia are multi-system disorders that affect several organs and physiological functions due to spinal cord or bone marrow injury. Patients who are not treated properly are at higher risk of death. The management of this case covers the inpatient care during the acute phase to the phase of rehabilitation in the outpatient or home setting16 (Table 2).
Overview of the papers on clinical pathway for different cases.
| Reference | Year | Main focus | Conclusion |
|---|---|---|---|
| Perer et al14 | 2015 | The utilization of care pathways using electronic medical record | Analyzing the diagnosis and treatment cohort in hyperlipidemia patients with hypertension or diabetes mellitus |
| Han et al15 | 2015 | Effectiveness of service and education of health in the communities by using pathway | Patients and health workers benefited from the positive impact of clinical pathways |
| Zander 16 | 2002 | Standards that can bridge the gap between patients and health care professionals | A clinical pathway is a good tool for patient care programs, as evidence-based practice |
| McClimens et al17 | 2013 | A clinical pathway tool used to refer patients from hospitals to health centers | Integrated services between hospitals and health centers are essential to meet the needs of the population. This is a tool for the transformation of long-term health care. It can meet the needs of complex societies in terms of health, welfare and lives independently not depending on the other peoples |
A clinical pathway provides guidance with the multidisciplinary approach of patient management. With the help of this tool, health care providers can estimate the duration of treatment for each case. They can also determine the length of the queue of patients according to the number of patients being treated, and, with that information, they can calculate the total time required for the health care system9.
A clinical pathway assists health care providers to deliver more effective and efficient care, as the treatments for the specific cases are standardized. This could lead to fewer complications and shorter average length of stay (ALOS) at the hospital10. ALOS, however, is not only influenced by clinical or rehabilitation outcomes but also by supporting aspects such as logistics, a patient's social and cultural factors, individual factors, and health insurance. Health insurance is set up on a relative diagnosis group basis, which calculates the fixed budget of the patient per day, fluctuating each year5,21.
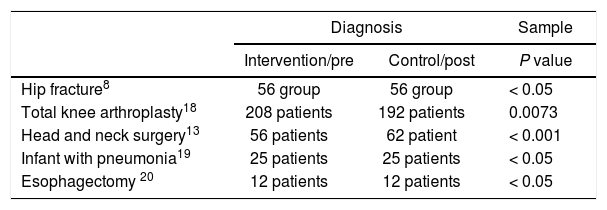
Treatments of patients with carcinoma of the head and neck are the most expensive among all malignant cancer care in the health care system. The hospitalization expenses make up the highest cost, especially in the post-surgery treatment. Post-operative care is a complex process and requires long ALOS12. Collaborative care involving physicians, nurses, physiotherapists, and respiratory specialists is necessary in the recovery phase of head and neck carcinoma cases. This treatment requires continuity to achieve cost-effective clinical interventions. A clinical pathway provides guidelines for specific diagnosis and intervention in the particular time frame and condition (Table 3). This can minimize delays, mistreatments, and duplications of interventions, and maximize the effectiveness and efficiency of care11,22,23 (Table 4).
Comparison of average length of stay and cost effectiveness for patient intervention with clinical pathway and control.
| Diagnosis | Sample | ||
|---|---|---|---|
| Intervention/pre | Control/post | P value | |
| Hip fracture8 | 56 group | 56 group | < 0.05 |
| Total knee arthroplasty18 | 208 patients | 192 patients | 0.0073 |
| Head and neck surgery13 | 56 patients | 62 patient | < 0.001 |
| Infant with pneumonia19 | 25 patients | 25 patients | < 0.05 |
| Esophagectomy 20 | 12 patients | 12 patients | < 0.05 |
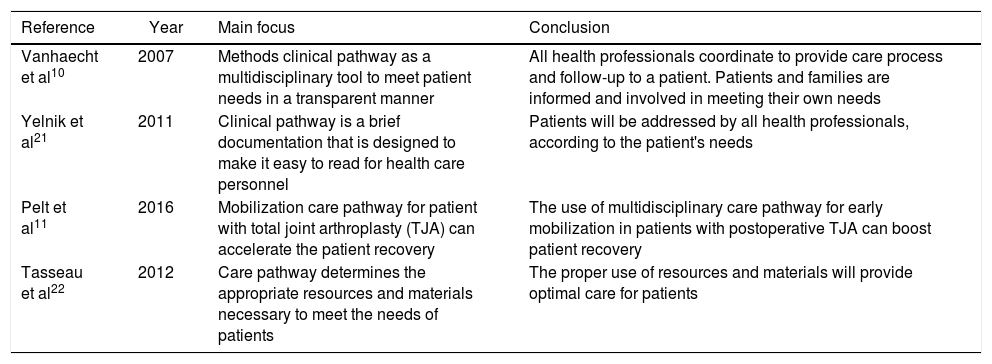
Overview of the papers on interprofessional collaboration and clinical pathway and their relations to quality of health service.
| Reference | Year | Main focus | Conclusion |
|---|---|---|---|
| Vanhaecht et al10 | 2007 | Methods clinical pathway as a multidisciplinary tool to meet patient needs in a transparent manner | All health professionals coordinate to provide care process and follow-up to a patient. Patients and families are informed and involved in meeting their own needs |
| Yelnik et al21 | 2011 | Clinical pathway is a brief documentation that is designed to make it easy to read for health care personnel | Patients will be addressed by all health professionals, according to the patient's needs |
| Pelt et al11 | 2016 | Mobilization care pathway for patient with total joint arthroplasty (TJA) can accelerate the patient recovery | The use of multidisciplinary care pathway for early mobilization in patients with postoperative TJA can boost patient recovery |
| Tasseau et al22 | 2012 | Care pathway determines the appropriate resources and materials necessary to meet the needs of patients | The proper use of resources and materials will provide optimal care for patients |
Interprofessional collaboration embraces all health professions—physicians, nurses, physiotherapists, and social workers—in an equitable responsibility and accountability according to each role. Health care teamwork is a dynamic process consisting of two or more health professionals with different educational backgrounds and skills4,9. It can minimize the duplication of interventions to attain the best outcome for the patient in an effective and efficient manner, leading to patient satisfaction. Interprofessional collaboration allows for interdisciplinary sharing to resolve health problems, to perform assessments, and for planning and treatment. Effective communication is key in implementing interprofessional collaboration to improve the quality of health services10. Interprofessional collaboration should be developed and given ongoing support by the management of health care facilities. It must be implemented transparently and evaluated continuously by the management of health care facilities so as to increase efficiency and effectiveness. Health care facilities should create equality and encourage the cooperation of all healthcare professions.
A clinical pathway can be stored in a hospital database to be used as a source for further analysis in diagnosis or treatment-related studies. An exploratory study on the utilization of medical records showed that clinical pathways are more meaningful and beneficial for deeper studies if they are consistently and thoroughly documented23. Basic monitoring, such as blood pressure, temperature, pulse, height, and weight monitoring should be well-recorded. This analysis can be used to evaluate the activities carried out by health workers14.
A qualitative study to examine the effectiveness of service and education of health care in the community was also reviewed in this study. The study was conducted for six months by interviewing 25 patients aged 60 years and over15. Patients and health professionals reported positive impacts of clinical pathways. Patients received continuous health education which contributed to the maintenance of their condition and compliance with follow-up care24.
A clinical retrospective study found that a clinical pathway is the key for health care professionals to carry out care activities. Each patient has different needs and requires different treatments16. Clinical pathways bridge the gap between patients and health care professionals. They provide directions to the health workers to determine the patient outcomes, which range from attaining comfort to dying with dignity. It is an easy tool to be implemented without consultation to the other health care professional so that the results are more faster20.
Clinical pathways are not only carried out at hospitals but in all healthcare facilities—for example, in community healthcare settings. Quasi-experimental studies and focus group discussions have reported that patients who require further treatment need to be referred to the health center. Clinical pathways are required to integrate care from hospitals to health centers to facilitate patient recovery17.
Some RCTs assessed the decrease in ALOS and financing after implementation of a clinical pathway on several patient diagnoses. A study was conducted in 112 patients with hip fracture at an American hospital, with the result of decreased ALOS8. In 400 patients with total knee arthroplasty, clinical pathway contributed to an average decrease in ALOS to 26 days, less pain, and fewer complications. Patients with head and neck surgery had ALOS 7.2 days shorter than the patient group with no clinical pathway13. Meanwhile, infant patients with pneumonia who received clinical pathways had less antibiotics, oxygen, and IV fluid therapy than patients in the conventional intervention. However, the esophagectomy patients showed no significant difference of ALOS19.
A retrospective study on clinical pathways was conducted among postoperative patients. The researchers reported that clinical pathways facilitate early mobilization, which could reduce complications, decrease hospital acquired infections, improve patient safety, speed recovery, and decrease ALOS25. Mobilization of the patient must be identified early in a multidisciplinary approach21.
Clinical pathway implementation may lead to lower ALOS. Health care personnel should coordinate and communicate with patients and their families throughout procedures the care process26. Health care professionals should perform a critical analysis of the patient to determine good and proper care. Additionally, all healthcare personnel should work together and be committed to meet the needs of patients, thus increasing the quality of services and cost effectiveness12. A clinical pathway is an indicator for the improvement of service quality. It can help reduce the incidence of nosocomial infection and improve patient safety.
The authors would like to thank Dr. Junaiti Sahar, SKp., M App.Sc., Ph.D., who has led us to participate in this study, Mrs. Dessie Wanda, SKp., MN, Ph.D., who has facilitated and continues to motivate us to achieve optimal results, and Miss Chairun Nisah Ardiantari who helped us to conduct this programme review smoothly and correct our report.