The purpose of this study was to identify factors that may influence strategies for increasing nurse retention.
MethodThis research is descriptive research using a cross-sectional approach. The study used a total sampling of a head nurse who works in a general hospital in Jakarta. The instrument used was a modification of the nurse's retention strategy instrument developed by Al-Zayyer (2003).
ResultsThe results showed that there is a significant relationship between retention strategy and organizational structure, leadership support, planning function, staffing function, and controlling function (p=0.002–0.044, α<0.05). The most dominant factors that influenced retention were leadership support (p=0.032, OR=2.817, 95% CI) and staffing function (p=0.042; OR=2.714, 95% CI).
ConclusionsNurse retention strategies employed by the head nurse need strong support from hospital management to achieve success in improving nurse retention international databases.
Nurses require support from the head nurse in carrying out their duties. The ability of nurses to perform their duties can be influenced by their relationship with the head nurse and the commitment of the head nurse to maintaining the stability of the work environment. Research on the relationship between leadership roles and staff's desire to leave positions found that those in leadership roles have a significant influence on organizational success in reducing turnover and increasing staff retention.1–4 Nurse turnover is one of the causes of a shortage of nurses in the hospital. Nursing turnover results in losses for the hospital, both financially and in terms of treatment quality. The shortage of nurses because of resignation, a problem often faced by government-owned public hospitals, exceeded the standard of 10% turnover in 2016 and 2017. Reasons for resignation include workload, compensation, supervisory guidance, relationships with colleagues, family reasons, and opportunities for self-development.
General Hospital's accreditation standard states that hospital management ensures a mutual program for staff retention that maintains qualified and competent staff for the upbringing process.5 The retention program requires further development because the shortage of nurses is projected to increase significantly between 2025 and 2030.6,7 The hospitals should devise robust strategies for retaining nurses. An appropriate retention strategy can increase job satisfaction, improve performance, reduce turnover, strengthen discipline, and can have other positive effects such as growth in innovation, fewer incidents, and decreased work stress. The study found that a supportive work environment exerted a significant positive influence on nurse job satisfaction and performance.8,9
Head nurses employ several retention strategies in guiding the staff in work adaptation process and day-to-day tasks. The nurse's retention strategy has been discussed in several studies resulting in several strategies to improve nurse retention through developing an organizational culture and creating a positive work environment.10 This strategy provides comfort and job safety for nursing staff, creates harmonious relationships between staff and superiors, and provides opportunities for unconstrained opinion.11 Another strategy is to apply effective leadership, guidance and optimal orientation, work flexibility, and certain professional career development.3,12–14
Strategies implemented by the head nurse are often less successful due to several factors such as hospital policy, individual factors, and organizational factors. Factors affecting the head nurse retention strategy have not been widely discussed and proven in the study. This research needs to be done to identify the problems faced by the head nurse in implementing strategies to improve nurse retention. This research can be a basis for making improvements in the management of the nursing resource.
MethodThe study employed descriptive research with a cross-sectional approach that aimed to identify the relationship between individual and organizational factors and retention strategy. This study used total sampling with a sample group of 99 head nurses working in general hospitals in Jakarta. The research instrument consisted of four questionnaires. Questionnaire A concerned the demographics of head nurses. Questionnaire B measured the knowledge of nurse retention. Questionnaire C measured the effectiveness of retention strategies developed from the “Nursing Administrator Survey Recruitment and Retention in Nursing” questionnaire.15 The result of the validity test of questionnaire C determined that all statements were valid (r=0.338–0.744). Questionnaire D measured factors affecting retention strategies developed by the researcher based on the literature review. The result of the validity test of questionnaire D obtained r>0.202. Cronbach's alpha for questionnaires categorized consistency to be almost perfect (0.781–0.957).
The research was conducted following an ethical review and approval by the Health Research Ethics Committee of the Faculty of Nursing, University of Indonesia (number: 57/UN2.F12.D/HKP.02.04/2018, March 22nd, 2018). Data were analyzed descriptively using frequency distribution, while a chi-square test was used to identify the relationship between dependent and independent variables. A logistic regression test was used to identify factors affecting the head nurse retention.
ResultsRetention strategies employed include positive organizational culture, positive work environment, effective leadership, guidance and orientation, career development, compensation, and work flexibility. Leadership obtained the largest percentage of perceived effective implementation by the head nurse (69.7%). The strategies that obtained the second-largest percentage were, jointly, a positive work environment and compensation (56.6%), while work flexibility received the lowest percentage of perceived effective implementation (35.4%) (see Table 1). The implementation of retention strategies is considered effective by the average head of the nurse, except for work flexibility.
Nurses’ retention strategy at General Hospital in Jakarta, Mei 2018 (N=99).
| Variables | Category | n (%) |
|---|---|---|
| Head nurse retention strategy (composite) | Less effective | 41 (41.4) |
| Effective | 58 (58.6) | |
| Positive organizational culture | Less effective | 40 (40.4) |
| Effective | 59 (59.6) | |
| Positive work environment | Less effective | 43 (43.4) |
| Effective | 56 (56.6) | |
| Leadership | Less effective | 30 (30.3) |
| Effective | 69 (69.7) | |
| Guidance/orientation | Less effective | 48 (48.5) |
| Effective | 51 (51.5) | |
| Career development | Less effective | 44 (44.4) |
| Effective | 55 (55.6) | |
| Compensation | Less effective | 43 (43.4) |
| Effective | 56 (56.6) | |
| Work flexibility | Less effective | 64 (64.6) |
| Effective | 35 (35.4) |
Of the head nurses surveyed, 56.8% and 62.5% of those younger than 40 and 40 to 50 years old, respectively, had implemented effective retention strategies, while 54.5% of head nurses older than 50 had implemented such strategies (Table 2). The results of the analysis showed no significant difference in the proportion of effective retention strategies implemented by head nurses with less than 10 years of experience, those with 10–20 years of experience, and those with more than 20 years of experience. There was also little or no significant difference between the proportion of effective retention strategies implemented by head nurses with less than five years of experience and those with more than 5 years of experience.
The relationship between head nurse characteristics and retention strategies in General Hospital in Jakarta, Mei 2018 (N=99).
| Variables | Retention strategy | |||||
|---|---|---|---|---|---|---|
| Less effective | Effective | Total | χ2 | OR (95% CI) | p | |
| n (%) | n | n | ||||
| Age | ||||||
| <40 years old | 16 (43.2) | 21 (56.8) | 37 (100) | 0.452 | 0.985(0.581–1.670) | 0.798 |
| 40–50 years old | 15 (37.5) | 25 (62.5) | 40 (100) | |||
| >50 years old | 10 (45.5) | 12 (54.5) | 22 (100) | |||
| Length of work | ||||||
| <10 years | 4 (44.4) | 5 (55.6) | 9 (100) | 0.051 | 1.070(0.583–1.963) | 0.975 |
| 10–20 years | 13 (41.9) | 18 (58.1) | 31 (100) | |||
| >20 years | 24 (40.7) | 35 (59.3) | 59 (100) | |||
| Length of time as a head nurse | ||||||
| ≤5 years | 23 (43.4) | 30 (56.6) | 53 (100) | 0.051 | 1.193(0.534–2.664) | 0.822 |
| >5 years | 18 (39.1) | 28 (60.9) | 46 (100) | |||
| Educational background | ||||||
| Diploma degree | 2 (25.0) | 6 (75.0) | 8 (100) | 1.151 | 0.591(0.211–1.650) | 0.562 |
| Bachelor's degree | 35 (42.2) | 48 (57.8) | 83 (100) | |||
| Master's degree | 4 (50.0) | 4 (50.0) | 8 (100) | |||
| Level of competency | ||||||
| 8 (66.7) | 4 (33.3) | 12 (100) | 2.502 | 3.273(0.914–11.723) | 0.069 | |
| ≥Clinical nurse 3 | 33 (37.9) | 54 (62.1) | 87 (100) | |||
| Nursing services type | ||||||
| Outpatient | 13 (44.8) | 16 (55.2) | 29 (100) | 1.139 | 1.329(0.707–2.498) | 0.566 |
| Inpatient | 24 (42.9) | 32 (57.1) | 56 (100) | |||
| Specific ward | 4 (28.6) | 10 (71.4) | 14 (100) | |||
| Knowledge | ||||||
| Less | 19 (42.2) | 26 (57.8) | 45 (100) | <0.001 | 1.063(0.476–2.372) | 1.000 |
| Good | 22 (40.7) | 32 (59.3) | 54 (100) | |||
Seventy-five percent of the head nurses with diploma degrees implemented effective retention strategies, while 57.8% of those with a bachelor qualification and 50% of those with a master's degree in nursing did. The result showed that the difference in the proportion of effective retention strategies among head nurses with a diploma and those with a bachelor's degree was 17%, while the difference in proportion between those who have D3 nursing qualifications and S2 nursing is 25%.
The difference in the proportion of effective retention strategies among head nurses with a level of competence below Clinical nurse 3 and those with a level of competence above Clinical nurse 3 was 29%. The proportion of effective retention strategies between head nurses in outpatient and inpatient units was virtually the same, while between the outpatients and special ward there was a difference of 16%. The proportion of difference in knowledge of effective retention strategies was not statistically significant between the head nurses with more knowledge and those with less. The result of the statistical tests for all characteristics of the head nurses was obtained as p>0.05, from which it can be concluded that there was no significant relationship between age and retention strategy.
Good staffing functions obtained the largest proportion of perceived effectiveness (76.7%) in supporting retention strategies, while 76.1% assessed good leadership support as an effective retention strategy. The average perception among the head nurses of the effectiveness of good organizational factors in implementing an effective retention strategy was more than 70%, with only two factors receiving less than 70%, organizational structure and organizing function (Table 3).
The relationship between organizational factors and head nurse retention strategies in General Hospitals in Jakarta, Mei 2018 (N=99).
| Variables | Retention strategy | |||||
|---|---|---|---|---|---|---|
| Less effective | Effective | Total | χ2 | OR (95% CI) | p | |
| n (%) | n (%) | n (%) | ||||
| Organizational structure | ||||||
| Less | 17 (58.6) | 12 (41.4) | 29 (100) | 4.502 | 2.715(1.117–6.603) | 0.044* |
| Good | 24 (34.3) | 46 (65.7) | 70 (100) | |||
| Leadership support | ||||||
| Less | 30 (56.6) | 23 (43.4) | 53 (100) | 9.541 | 4.150(1.742–9.890) | 0.002* |
| Good | 11 (23.9) | 35 (76.1) | 46 (100) | |||
| Planning function | ||||||
| Less | 26 (54.2) | 22 (45.8) | 48 (100) | 5.267 | 2.836(1.240–6.490) | 0.022* |
| Good | 15 (29.4) | 36 (70.6) | 51 (100) | |||
| Organizing function | ||||||
| Less | 30 (46.2) | 35 (53.8) | 65 (100) | 1.230 | 1.792(0.752–4.271) | 0.267 |
| Good | 11 (32.4) | 23 (67.6) | 34 (100) | |||
| Staffing function | ||||||
| Less | 31 (55.4) | 25 (44.6) | 56 (100) | 9.050 | 4.092 | 0.003* |
| Good | 10 (23.3) | 33 (76.7) | 43 (100) | (1.694–9.886) | ||
| Actuating function | ||||||
| Less | 30 (50.0) | 30 (50.0) | 60 (100) | 3.773 | 2.545(1.075–6.026) | 0.052 |
| Good | 11 (28.2) | 28 (71.8) | 39 (100) | |||
| Controling function | ||||||
| Less | 28 (53.8) | 24 (46.2) | 52 (100) | 5.940 | 3.051(1.317–7.068) | 0.015* |
| Good | 13 (27.7) | 34 (72.3) | 47 (100) | |||
The result of the statistical test showed that there was a significant relationship between organizational structure, leadership support, planning function, staffing, and control function and head nurse retention strategy (p=0.002–0.044). Organizing function and guiding function showed no significant relationship with retention strategy (Table 3).
Multivariate analysis was performed to determine the most dominant factors affecting nurse retention strategies. Eight variables were included in the modeling. These were the length of work, competency level, organizational structure, leadership support, planning function, organizing function, staffing function, actuating function, and controlling function.
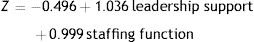
The initial model of logistic regression was obtained after the variable with p>0.05 was released one by one. The result of preliminary modeling obtained two variables with p<0.05; these were leadership support (p=0.032) and staffing function (p=0.042). Furthermore, the interaction test between leadership support and staffing function was used to identify the interaction between the two variables. The interaction test results obtained p=0.150 (p>0.05), which means there was no interaction between the two variables.
The result of the final model showed that the variables most related to a successful retention strategy were leadership support (p=0.032, OR=2.817, 95% CI: 1.094–7.252) and staffing function (p=0.042; OR=2.714, 95% CI: 1.037–7.106). Based on these results it can be concluded that good leadership support is 2.817 times more likely to support effective implementation of retention strategies than less effective leadership support after being controlled by the staffing function. Good staffing function provides 2.714 times the support of effective retention strategies provided by less effective staffing function after being controlled with leadership support (Table 4).
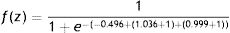
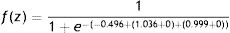
Based on the results of the analysis on the final model of logistic regression, the multivariate model equation is as follows:
The application of the generated model can be used to calculate the probability of an effective retention strategy. Below is the result of the probability calculation.
Based on the above calculation, good leadership support and good staffing functions are 82.33% more likely to produce an effective retention strategy than poor leadership support and staffing functions.
Based on the above calculation, less leadership support and less effective staffing functions are 37.84% to produce an effective retention strategy than good leadership support and staffing functions.
DiscussionThe measured retention strategy is a combination of several retention strategies, such as positive organizational culture, positive work environment, effective leadership, guidance/orientation, career development, compensation, and work flexibility. The proportion of effective head nurse retention strategies is 58.6%. Effective leadership achieved the largest percentage of effectiveness (69.7%) compared with the proportion of other retention strategies. The leadership of the head nurse is the main factor that staff considered when deciding whether to continue working in a hospital.3,16,17 A systematic review found that leadership was most of the most discussed element in 22 studies on nurse retention strategies.18
Effective leadership creates a positive work environment through staff empowerment, team work and harmonious collaboration, inter-staff caring relationships, ethics, and support for fellow staff. This is supported by a study that found that employees’ desire to change jobs was closely linked to staff empowerment and leadership roles.19 The leadership of the head nurse can be used to guide staff and apply an appropriate leadership model. The results showed that the leadership model and the guidance of the head nurse had a significant relationship with nurse retention.4 The most effective leadership model was the transactional leadership model.4
Age, length of work, length of work as a head nurse, educational background, competency level, nursing services type, and knowledge were not significantly related to effective retention strategies. Contrasting to some articles discussing the characteristic relationship of managers with staff management and leadership style, related research results showed that younger and older managers had different leadership styles. Older managers can be a source of broader consultation and more supportive of staff participation than younger managers. Likewise, the length of work was associated with the situational ability and performance of managers.20 The absence in this study of a significant relationship between the characteristics of the head nurse and the nurse's retention strategy may be influenced by the distribution of data on each characteristic of the head nurse, which is almost equal, especially in the length of work, level of education, and level of competency.
The organizational structure is significantly related to the retention strategy (p=0.044). This result is supported by the research about the relationship between organizational structure and performance, which found that the most dominant factor affecting the performance was coordination and unity of command of the organizational structure. Other studies also support the result of this study that found a significant relationship between the organization process and effectiveness of the organization, both according to the centralized and decentralized approach (p<0.05, α=0.05).
Analysis of the data found a significant relationship between leadership support and the effectiveness of the nurse retention strategy of the head nurse (p=0.002). Good leadership support had 4.150 times greater impact on the effectiveness of the retention strategy than less effective leadership support. Good perception of a head nurse's leadership support increased when a head nurse had greater interactions with the hospital's leaders. Hospital management support is pivotal in implementing staff retention strategies, support, and leadership commitments to improve individual performance and retain staff.11
A harmonious relationship between the hospital leaders and the head nurse could increase the confidence of the head nurse in managing nursing care and services. The head nurse needs to establish a harmonious relationship with staff, peers, and leaders. Therefore, the head nurse needs to improve his or her interpersonal competency because interpersonal skills are essential for the head nurse in carrying out management functions. The study found that the increased knowledge gained from interpersonal skills training significantly influenced the interpersonal and leadership role of the head nurse (p<0.05).21
The hospital's leaders established the programs to improve nurse retention discussed in the hospital's strategic planning by including it in annual performance planning. Leadership support for nursing care can be provided through the approval of the retention program budget, including the development of career path systems, the establishment of appropriate compensation, the provision of equipment and facilities for the security and the comfort of staff in the workplace, and support for workplace programs prepared by the head nurse for creating positive work environments.1,16,22–25
This study also found a significant relationship between the planning function and retention strategy (p=0.022). This aligns with the results of research indicating a significant relationship between planning and organizational performance.26 The planning function is essential in the nursing management process cycle. The planning of the staff retention program prepared by the hospital management became the reference for the head nurse in implementing the staff retention strategy in the ward.
The staffing function has a significant relationship with the head nurses’ retention strategies (p=0.003). The result of bivariate analysis on the independent and dependent variables has important significance, so it can be assumed that the better the management function of the hospital management, the more effective the nurse retention strategy implemented by the head nurse.
The staffing functions of hospital management include recruitment, selection, orientation, and retention.17,23 Hospitals should create requirements for selection, orientation programs, and staffing for each position, including the head nurse. These requirements are beneficial for support a hospital's performance. This conforms with the results of research indicating that the training provided by a hospital influences individual performance and can improve the performance of individuals and hospitals.27 A head nurse who meets the qualification and competency requirements set by a hospital is expected to have a greater ability to implement and direct staff retention strategies in the ward.
Excellent staffing function can support the head nurse to improve staff retention in the ward. The hospital faces challenges in fulfilling these needs and its allocations. Staffing management is affected by the complexity of the patient, the competency of nurses, the physical condition of the ward, and the availability of technology.28 However, hospitals should strive to fulfill their needs by addressing the factors influencing them. An optimal management system is essential for improving professional nursing services, decreasing incidents, and improving staff satisfaction and retention.28
The result showed no significant correlation between the guiding function and the head nurse's retention strategy (p=0.052). The result of the analysis showed that the proportion of effective retention strategies of good directing functions is much greater than the lack of directing function. In carrying out the guiding function, hospital management provided motivation, support, direction, and adequate provision for the head nurse. Head nurses need support in performing their duties correctly, including opportunities to develop and increase their knowledge and ability to create a positive and constructive work environment. This is supported by the results of research that found that empowerment structures (opportunities, information, support, resources, formal strength, natural forces) are significantly related to climate.29
The controlling function was significantly correlated with retention strategies (p=0.015). The controlling function helps to monitor and evaluate hospital and individual performance results. The implementation results of the controlling function can be used as an evaluation tool for the hospital to identify and make needed improvements. Hospital management, the head nurse, and staff can learn from the results of performance monitoring as the indicator. Staff management including nurse retention implementation will be more effective when measured every year. Quality indicators related to staff management are monitoring of nurse turnover, nurses’ skill mix, and nurses’ satisfaction surveys.23,30,31 The achievement of quality indicators in nursing staff management can be a source of continuous learning and inspiration to improve workplace comfort and increase nurse retention.
The final modeling results showed that two factors influenced head nurses’ retention strategies, namely leadership support and the staffing function. The analysis showed the probability of effective retention strategy implementation with excellent leadership support and excellent staffing function was 82.33% compared with a lack of leadership support and lack of staffing function. Good leadership support and staffing function had the potential to increase the effectiveness of a retention strategy as much as 37.84% compared with less effective leadership support and staffing function.
The standard turnover rate is 10%, so a good standard for nurse retention is 90%. Based on these standards, the probability of obtaining a successful retention strategy from excellent leadership support and staffing function is still below 90%. Other factors that influence the effectiveness of a retention strategy are organizational factors and performance of the head nurse as discussed above. Individual nursing staff factors may also be relevant.
The individual factors of the nursing staff can relate to staff retention as well as the retention strategy exercised by the head nurse. These factors include workload, saturation, leadership, opportunities for improvement, role clarity, achievement, recognition, and work environment.3,32–34 Age, attitudes, health conditions, and length of work of nursing staff could also be significant.32 These factors must be identified to improve the success of nurse retention strategies and prevent nurse turnover.
Nursing retention strategies conducted by the head nurse need strong support from hospital management. Support can be provided by giving particular attention to the ward, support for work programs and activities that have been prepared by the head nurse, and appreciation for the improvement of team performance. Hospital management can also create a program to identify the outstanding ward in a given year by conducting routine evaluations and encouraging continuous developments and improvements. The opportunity for a head nurse to express ideas for innovation is also dependent on the support of hospital leaders, who can increase motivation and boost the creativity of the head nurse in team management.
Further research can be done to explore manager nurse perceptions at all levels, from low and middle to upper management, to identify nurse retention issues in hospitals. Research can also be carried out with numerous research samples using nurse staff as respondents to explore the perceptions of nursing staff regarding the implementation of retention strategies in the wards of several hospitals.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2018 funded by Department of Research and Community Engagements, Universitas Indonesia No. 1852/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.