Health professionals are unable to solve the family problems. Practically, health professionals are encouraged to make collaboration. One effort to improve health professional readiness is by joining the interprofessional education (IPE). Poltekkes Kemenkes Surakarta is implementing one Team One Family-Community Internship Program Interprofessional Education and Collaboration (OTOF-CIPIPEC).
This research aims to examine the effect of OTOF-CIPIPEC Implementation within the health students on readiness, teamwork, perception to the other professions and participants’ satisfaction.
MethodThis research is a quasi-experimental design with a pre-post without control research approach. The research population covers all students registered joining OTOF CIPIPEC at Poltekkes Kemenkes Surakarta with a total number of 1061 of students. The samples are collected using a total sampling technique. The samples for this research are those registered joining the OTOF CIPIPEC at Poltekkes Kemenkes Surakarta meeting the inclusion and exclusion criteria with a total number of 1031 of students. This research utilizes the Readiness for Interprofessional Learning Scale (RIPLS) questionnaires as its measuring instruments. This study was conducted in Mojosongo sub-district, Jebres district, Surakarta. This research involves 38 Community Units (In Indonesia known as Rukun Warga/RW) with a total number of 1066 of family heads and the Sibela Community Health Center. The data are analyzed using the Wilcoxon test and multiple linear regression test.
Result of the studyThe research results showed that there is a significant difference of readiness improvement, teamwork, and perception on other professions and satisfaction of the research subjects before and after joining OTOF-CIPIPEC (ρ<0.001). The average improvement scores of students’ readiness, teamwork, perception, and satisfaction are 63.2%, 62.5%, 62.57%, and 113.04% respectively. The results of the multivariate analysis show that teamwork and perception significantly influence the students’ readiness in their collaboration with the other professions (ρ<0.001) with the influence value of 0.93%.
ConclusionThis research concludes that OTOF-CIPIPEC implementation may improve readiness, teamwork, and perception of other professions and students’ satisfaction in interprofessional education (IPE).
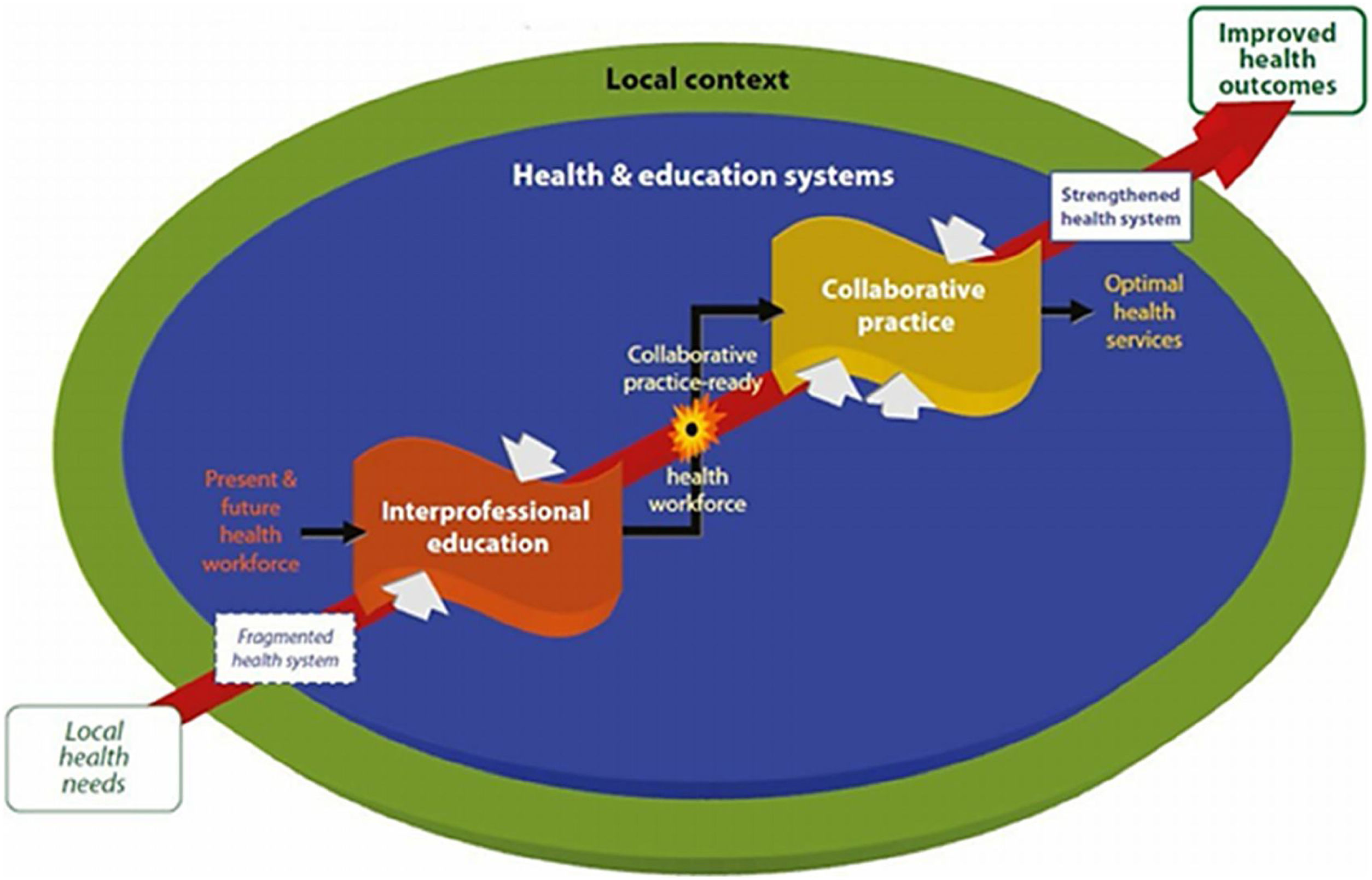
Nowadays, health problems increasingly become more complex in the society. Thus, the government has conducted a program of Sustainable Development Goal's (SD G's).1 Therefore, health professionals are required to work together in developing health in community.2,3 Health care now pays more attention to patients and families. Interprofessional education may provide the best treatments for patients.4,5 The collaboration process of health workers requires readiness, teamwork, and good perception to ensure that the students may obtain the knowledge and skills required for interprofessional practice.6 Thus, education is the key to improve the quality and satisfaction of health workers to practice collaboration with the other health workers.3 Interprofessional education (IPE) was introduced by the WHO to improve the quality of students for their readiness to collaborate with the other health workers.4,7 IPE is implemented by providing patient-centered care, safety, high-quality, and affordable services.8 The Health Polytechnic of the Ministry of Health of Surakarta (in Indonesia known as Poltekkes Kemenkes Surakarta) is an Institution which produces competitive health workers for health development programs through community empowerment. Poltekkes Kemenkes Surakarta has 8 (eight) health departments which collaborate each other in Community Internship Program activities with the Interprofessional Education and Collaboration (CIP-IPEC) model: “One Team – One Family & Community Based”. The Community Internship Program with the Interprofessional Education and Collaboration (CIP-IPEC) model is the development of an integrated program that has been conducted periodically.
The program may also examine the students’ readiness in facing professional collaboration in the working world, improvement of teamwork, as well as students’ perceptions and satisfactions with IPE implementation. This program is oriented to family services as clients with the concept of “One Team One Family – Community Based” in the working area of Surakarta Health Office, especially Mojosongosub-district, Jebres district, Surakarta. This study aims to determine the implementation effect of a team one family on the interprofessional education program and Collaboration conducted by the health students organized by Poltekkes Kemenkes Surakarta.
Literature reviewIPE began in 1960s and 1970s, in most parts of the United Kingdom and the United States. IPE is also one powerful method to enhance teamwork or professional education reformation.9,10 The IPE program within a health professional environment can improve the existing curriculum with IPE curriculum.10 Education enables health policy to provide better work practices and productivity to increase the patients’ outcomes, educational spirit, patients’ safety, and better access to health services.7,11 The family-centered collaborative practice is the main objective of IPE, through the sustainable reflection practices.12 The benefits are not only for patients and students, but also related to the substantial production of “work products” for educational institutions.13 With this assessment, the institution may evaluate whether the existing IPE program has operated in accordance with the curriculum.14,15
MethodsPopulation and sampleThe population of this study is all students of Poltekkes Kemenkes Surakarta who have been practicing at the interprofessional education programs in community consisting of 1061 students from 8 different majors.
Inclusion and exclusion criteria:
This study has some inclusion criteria:
- •
The students of Nursing, Midwifery, Physiotherapy, Occupational Therapy, Orthotics and Prosthetics, Speech Therapy, Acupuncture, and Herbal Medicine in the Academic Year of 2018/2019 registered in the Study Plan Card (KRS).
- •
The students have completed all academic programs meeting the required curriculum competencies.
- •
The students should have attended the OTOF CIPIPEC initial meeting.
- •
The students are proposed by each Study Program and still active.
- •
The students have read the information sheet and signed the Letter of Agreement to become the research subjects.
This research used a quasi-experiment design with a pre-posttest to analyze the implementation effect of OTOF CIPIPEC on health students. The study was conducted by Poltekkes Kemenkes Surakarta consisting of 8 (eight) departments which have implemented an interprofessional education program. The program was conducted starting from July 19 to August 9, 2019. The research location is in Mojosongo Sub-District, Jebres District, Surakarta with 38 Community Units (RW), 1066 Family Heads (KK), and Sibela Public Health Center, Surakarta. The research stages start by planning locations in the community, implementing actions in Jebres district, Surakarta, as well as observing and evaluating for 3 weeks. At the beginning of this research, there were 1061 research subjects. However, only 1031 research subjects had the complete data to analyze. The data analysis was conducted using the Wilcoxon test (Fig. 1).
ResultNursing is a department with the most students participate in the OTOF-CIPIPEC activities (18.1%) followed by the midwifery department by 17.8% while acupuncture department has least students participate in the OTOF-CIPIPEC activities by only 8.1%. Before the OTOF-CIPIPEC activities are conducted, the average students’ readiness is 27.18 (7.9), while after the OTOF-CIPIPEC activities are conducted the average students’ readiness increases up to 44.41 (14.61). The result of Statistical analysis shows that the average students’ readiness before and after implementation (p-value 0.001) increases by 63.2%. Before the OTOF-CIPIPEC activities are conducted, the average students’ teamwork is 44.43 (9.5), while after the OTOF-CIPIPEC activities are conducted, the average students’ teamwork increases up to 71.88 (17.4). The result of statistical analysis shows that the average students’ teamwork before and after implementation (p-value<0.001) increases by 61.17%.Table 1 explains that before the OTOF-CIPIPEC activities are conducted, the average students’ perception on the other professions’ role is 31.85 (10.1), while after the OTOF-CIPIPEC activities are conducted, the average students’ perception on the other professions’ role increases up to 52.18 (18.2). The result of statistical analysis shows that the average students’ perception on the other professions’ role before and after implementation (p-value<0.001) increases by 61.03%. Table 2 explains that before the OTOF-CIPIPEC activities are conducted, the average students’ satisfaction is 20.42 (9.4), while after the OTOF-CIPIPEC activities are conducted, the average students’ satisfaction increases up to 45.23 (20.7). The result of statistical analysis shows that the average students’ satisfaction before and after implementation (p-value<0.001) increases by 113.04%. Table 3 shows that the OTOF-CIPIPEC activities may increase the students’ readiness through teamwork and perception on other professions’ role by 93.3%.
Comparison of students’ perceptions on the other professions’ role before and after learning treatment of interprofessional education and collaboration program.
| Component | Pre (n=1036) | Post (n=1036) | p value | Average increase % |
|---|---|---|---|---|
| Perception | <0.001 | 61.03 | ||
| Mean (SD) | 31.85(10.1) | 52.18(18.2) | ||
| Median | 33.0 | 52.0 | ||
| Range | 0–60 | 0–100 |
The health workers are required to collaborate with the other professions to solve the problems.16 Interprofessional education may bridge the students to prepare their readiness collaborating with the other professions. In this research, the OTOF-CIPIPEC activities may facilitate the students to increase their readiness, cooperation, perception and satisfaction in working with the other professions in community. If the management is conducted at the early stage, it is expected that the health problems may immediately be overcome.16
ReadinessStudents’ readiness can explain the students’ confidence when collaborating with the other professions. Too high self-confidence may lead to less effective care services, while less confidence may reduce the students’ motivation to solve the health problems.6 The result indicates that there is a significant increase in the students’ self-confidence before and after the implementation of OTOF-CIPIPEC (p-value<0.001). A study conducted by Anderson and Thorpe (2014)17 mentioned that community-based IPE is a solution to increase the students’ readiness to work with the other professions. Community-based IPE may facilitate the students to work in a partnership to have working experiences with the other professions. Students’ readiness to provide care services for patients in the community to improve the patient care18 is the key point. The use of IPE may increase the students’ readiness to improve their ability to collaborate with the other professions.19 According to Tataw (2011),20 the students’ readiness and competence to implement IPE start with several variables, including communication skill, emotion, value, reflection and patients care in the community. In addition, students’ competence and readiness are built based on the technical skill, cognitive function, moral, integrative function, relationship context, and thinking habit with the implementation of IPE in the community.17
TeamworkHealth workers are required to cooperate, coordinate and collaborate characterizing the interprofessional relationship to provide the patient-centered care called interprofessional teamwork.4 The research result has found that there is an increasing students’ teamwork before and after the implementation (p-value<0.001). This teamwork is for the implementation of OTOF-CIPIPEC, the students worked together to solve the family health problems. Through IPE in the community, the students gained experiences after working together with the other professions to understand each health profession's role.16 The key to increase collaboration is by improving communication among the team members.21 Educational institutions recommend this integration as a part of the health workers’ training and education. All health professionals must be well educated to provide the patient-centered care as the interdisciplinary team members, emphasize the evidence-based practices to improve the quality, patient safety, and informatics.5 The importance of effective communication, teamwork complexity and team decision are related to interprofessional development resulting in learning benefits. All tutors can see the interprofessional learning values and welcome the students’ feedbacks to improve the patient care.17,22 Referring to the WHO's view, interprofessional education aims at preparing all health professional students to be able to work together with the common objective to provide a safer and better health care system.11 Within the scope of community, each family has different health needs and problems.4 The IPE basic idea is that teamwork and collaboration do not only help the patients and clients discuss their needs but also help to resolve tensions between professions within a short-distance.10 In the implementation of OTOF-CIPIPEC, the students are required to work together in determining the appropriate treatments to solve the family health problems.
PerceptionBefore this research is conducted, the students have a low perception about other professions’ role. After the implementation of OTOF-CIPIPEC, the students are able to collaborate and work together to intensify their perceptions. The result of this research is in line with that conducted by Ilmanita (2014)6 stating that there is a perception increase of pharmacist students on the other professions after the implementation of IPE. IPE education may improve the interprofessional communication and the other professional perceptions that eventually increase the students’ confidence when treating the patients.23 A research conducted by Kahaleh et al. (2015)14 have found that IPE encourages interprofessional collaboration although the students’ score changes are various. IPE education in community may increase the other professions; perception changes. The students who have implemented IPE will show better attitudes toward the other professions when performing a teamwork in the community.17 After exposed to IPE, the students have a higher awareness related to the refection value in understanding and mutual understanding practices among the team members.12 IPE may improve overall interprofessional attitudes and cooperative skills. However, not all parts of the program meet the needs of all participating scientific disciplines due to the differences of educational backgrounds and knowledge.24
SatisfactionSatisfaction of students participating in OTOF-CIPIPEC increase after the implementation (p-value<0.001). The students’ satisfaction has increased by an average of 61.3% as the students h learned interprofessional collaboration skills in providing health care services similar to those performed in the real working world. The students may have direct experience, or share, and perform care services in accordance with each department's competencies and management.12 Team-based learning may increase the students’ motivation and patients’ safety. This valuable experience may increase the students’ satisfaction after the IPE implementation.25 When the students are able to work together and improve the patient care in the community, they may increase their satisfaction when the progress is achieved by the interprofessional team.26,27 Teamwork and professional interaction influence the students’ readiness to collaborate with the other professions after the implementation of OTOF-CIPIPEC by 93.3% (R2=93.3; p-value<0.001). This analysis showed that the students who can work within a team and have a good perception may be considered having better readiness to perform the collaboration practices and vice versa. Understanding each other's role and working together as an effective team can increase the students’ readiness to take care the patients. Therefore, IPE is proven effective and important for the students’ education to develop their readiness. Effective IPE is not easy to perform for the community-based education. However, IPE is proven to be effective to increase the average students’ readiness to have interprofessional collaboration.28–30 The implementation of OTOF-CIPIPEC may improve the students’ readiness for collaboration, teamwork, perceptions toward other professions, and satisfaction. The students’ readiness is significantly influenced by the incompetence in teamwork and perceptions to the other professions in interprofessional collaboration. Community-based implementation is considered greatly important because most research locations are still in the rural areas while community is the first line in community health problems.
Limitation and future researchThis research assesses the results before and after the implementation of OTOF-CIPIPEC, yet the variables within a long-term period and impacts have not been measured. This research focuses more on the students’ success, not assessing the satisfaction levels of stakeholders and educators participating in the OTOF-CIPIPEC activities. It is recommended that further research should assess the long-term impacts on the students participating in IPE. In addition, it is also recommended to conduct further research related to the impacts of OTOF-CIPIPE Complementation on the stakeholders’ and patients’ satisfaction.
Conflict of interestsThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Conference on Healthcare and Allied Sciences (2019). Full-text and the content of it is under responsibility of authors of the article.