This study aimed to examine the correlation between inhalation therapy and length of hospital stay in children under age of five with pneumonia.
MethodThis cross-sectional study included 102 consecutive patients (secondary data) with pneumonia. The patients were divided depending on the type of therapy they received: Group I used inhalation therapy with bronchodilator β-agonist + NaCl 0,9%, Group II used inhalation therapy with bronchodilator β-agonist and anticholinergic + NaCl 0,9%, Group III used inhalation therapy with NaCl 0,9%, and Group IV used no inhalation therapy.
ResultsThe study results showed a significant correlation between the use of inhalation therapy and the length of hospital stay (p = 0.000) after being controlled age, leucocyte count, and the type of antibiotic therapy. However, there was no significant correlation between the use of inhalation therapy and the length of hospital stay in children under the age of five with pneumonia after sex and oxygen therapy being controlled.
ConclusionsInhalation therapy with a combination of bronchodilator β-agonist and anticholinergic + NaCl 0.9% and with bronchodilator β-agonist + NaCl 0.9% are the two most effective treatments with which to reduce the length of hospital stay in toddlers with pneumonia.
Pneumonia still has a high rate of prevalence and remains one of the leading causes of deaths among toddlers worldwide, especially in developing countries. The World Health Organization (WHO) estimates that there are 156 million cases of pneumonia afflicting children under five years old annually. Pneumonia is responsible for 15% of deaths among children under five years old, accounting for 922 thousand deaths in 20151,2.
According to a survey conducted by the Indonesian Health Ministry in 2013, the prevalence rate of pneumonia in all age groups throughout Indonesia increased from 2.1% in 2007 to 2.7% in 2013. In terms of age groups, children aged 1 to 4 years have the highest rate of pneumonia prevalence, at 18.5%3. Of all Indonesian provinces, West Nusa Tenggara Province has one of the highest pneumonia prevalence rates among children under five years old. It was estimated that in the province, as many as 54,220 children under five years old in 2014 were afflicted by pneumonia but that only 26,631 (49.12%) were treated by professional health workers4.
One of the most troubling symptoms experienced by pneumonic children is respiratory tract blockage due to mucus accumulation. The respiratory tract can be cleared of mucus accumulation by performing various medical interventions, one of which is inhalation therapy. Inhalation therapy can help remove the airflow obstruction and reduce the mucus accumulation in the patient's respiratory tract5. In spite of the fact that inhalation is performed on most patients, some medical professionals do not recommend it for the routine management of hospitalized children6.
The use of various therapeutic interventions may influence a patient's length of hospital stay. Appropriate and effective treatment is necessary to avoid recurrent infections, which can prolong the patient's duration of treatment at the hospital and thus increase treatment costs7. The purpose of this research project was to examine the correlation between inhalation therapy and length of hospital stay among pneumonic children under five years old.
MethodsThis study applied a descriptive-analytical research design and a cross-sectional approach. This study used secondary data which were obtained from the medical records of patients treated at the hospital within the one-year period from May 2015 to May 2016 and then written manually on the data forms. The respondents were selected using the consecutive sampling technique. The research sample consisted of 102 children under five years old who had been treated at the P3 Regional Hospital and had their treatment documented in the hospital's medical records. Our inclusion criteria were that (1) the patients were under five years old (aged 0 to 59 months) and (2) the patients were diagnosed with pneumonia and treated at the hospital. Our exclusion criterion was that the patients were treated at the hospital and diagnosed with pneumonia coupled with other infectious diseases, such as congenital heart disease or immunodeficiency disease. Samples were obtained using the consecutive sampling technique. The data were analyzed using the univariate and bivariate analyses with the Chi-square statistical test, which was performed using computer software. This research project was approved by the Ethics Committee of the Faculty of Nursing of Universitas Indonesia.
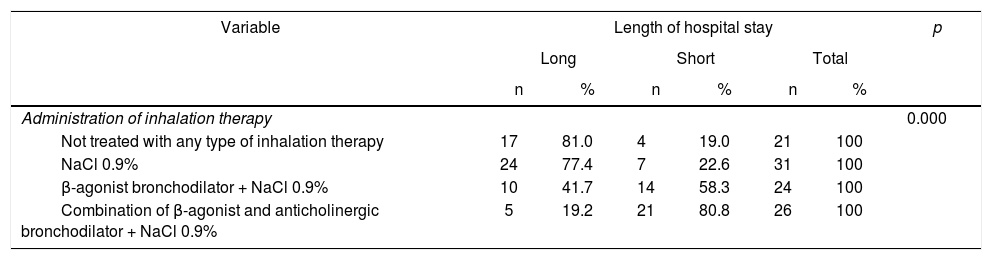
ResultsThe characteristics of the respondents showed that most of this study participants were male (70 children, or 68.6%). Their median age was 11 months. The youngest was 1 month old, and the oldest was 59 months old. Fifty-six samples (54.9%) had leucocytes ≤ 14,000/mm3. Most samples (71 children, or 69.6%) received second-line antibiotics, and the median oxygen therapy volume was 1 liter/minute. Twenty-one samples (20.6%) did not receive any inhalation therapy at all; 31 (30.4%) samples were treated with inhalation therapy using NaCl 0.9%, 24 samples (23.5%) were treated with inhalation therapy using β-agonist bronchodilator + NaCl 0.9%, and 26 samples (25.5%) were treated with inhalation therapy using a combination of β-agonist and anticholinergic bronchodilator + NaCl 0.9%. Fifty-six (54.9%) participants had a long treatment duration (> 5 days), whereas 46 (45.1%) participants underwent a short treatment duration. (Table 1)
Correlation between the Administration of inhalation therapy and the length of hospital stay for pneumonic children.
| Variable | Length of hospital stay | p | |||||
|---|---|---|---|---|---|---|---|
| Long | Short | Total | |||||
| n | % | n | % | n | % | ||
| Administration of inhalation therapy | 0.000 | ||||||
| Not treated with any type of inhalation therapy | 17 | 81.0 | 4 | 19.0 | 21 | 100 | |
| NaCl 0.9% | 24 | 77.4 | 7 | 22.6 | 31 | 100 | |
| β-agonist bronchodilator + NaCl 0.9% | 10 | 41.7 | 14 | 58.3 | 24 | 100 | |
| Combination of β-agonist and anticholinergic bronchodilator + NaCl 0.9% | 5 | 19.2 | 21 | 80.8 | 26 | 100 | |
Table 1 demonstrated that the administration of inhalation therapy using a combination of β-agonist and anticholinergic bronchodilator + NaCl 0.9% resulted in shorter treatment durations (80.8% of cases) as compared to other types of inhalation therapy or the absence of inhalation therapy. This result proves that there is a significant correlation between the administration of inhalation therapy and the duration of treatment (p = 0.000).
The results of the bivariate analysis of the confounding and dependent variables showed correlations between the age, number of leucocytes, and the type of antibiotics prescribed (p < 0.05), while there was no significant correlation between the sex and oxygen therapy volume (p > 0.05).
DiscussionPneumonic children in this study received different intervention treatments for the purpose of clearing their respiratory tracts of mucus deposits. The treatments consisted of inhalation therapy using NaCl 0.9% only, using β-agonist bronchodilator + NaCl 0.9%, and using a combination of β-agonist and anticholinergic bronchodilator + NaCl 0.9%, as well as treatments that did not involve any inhalation therapy at all. The results indicated that in general, children who received inhalation therapy had shorter treatment durations than those who did not receive inhalation therapy at all.
Therefore, inhalation therapy can be considered as an effective medical intervention for respiratory tract diseases. This is due to the fact that by means of inhalation, medicines can enter directly into the patients’ respiratory tracts and reach their lungs more quickly than if they are distributed via other systemic circulation routes8. The administration of respiratory tract medicines through inhalation therapy may reduce the necessary dosage and minimize potential side effects as compared to administration via other routes9. Inhalation therapy can help prevent respiratory tract blockage, dilute pulmonary secretions, and release mucus accumulations from respiratory tracts5.
In this study, pneumonic children who received inhalation treatment received three different types of therapy. The results showed that children who received inhalation treatment coupled with a bronchodilator, either β-agonist or the combination of β-agonist and anticholinergic has shorter treatment durations than children who received inhalation therapy with normal saline at 0.9%.
Most of the pneumonic children in the age range of 2 to 12 months and 1 to 5 years experienced wheezing10. Wheezing occurs due to the constriction or blockage of the lower respiratory tract, which must be immediately treated with a fast-acting bronchodilator. In addition to fast-acting bronchodilator medicines, such as those belonging to the β-agonist group, some therapists also prescribe a combination of β-agonist and anticholinergic bronchodilator by means of inhalation11,12.
The results of this study correspond to those published by the Scottish Intercollegiate Guidelines Network, which imply that inhalation therapy using a combination of β-agonist and anticholinergic bronchodilator results in a more significant bronchodilatation effect, faster recovery, and a shorter treatment duration13. It has been confirmed that the combination of β-agonist and anticholinergic bronchodilator can increase the bronchodilatation effect and that it is a simple combination therapy. In addition, this type of bronchodilator produces a more long-lasting effect and requires only 30 to 60 sixty minutes to reach its maximum effect14.
In addition to inhalation therapy coupled with a combination of β-agonist and anticholinergic bronchodilator, inhalation therapy coupled with β-agonist bronchodilator also resulted in shorter treatment durations. This finding corresponded to previous study indicating that the administration of inhalation therapy coupled with β-agonist bronchodilator could decrease the severity of disease and shorten the duration of treatment at hospitals without causing any negative effects15. Another study also discovered that inhalation with salbutamol (another member of the β-agonist bronchodilator group) may reduce patients’ treatment duration and disease severity16. Furthermore, inhalation therapy using salbutamol (β-agonist bronchodilator) + NaCl 0.9% produced a higher bronchodilatation effect than that produced via inhalation therapy using salbutamol only17. Another research discovered that inhalation therapy using salbutamol (β-agonist bronchodilator) + NaCl 0.9% could increase the frequency of coughing and the volume of discharged sputum as compared to salbutamol inhalation only18.
β-agonists are a group of fast-acting bronchodilators whose mechanism includes the relaxation of smooth muscles in the respiratory tract. The addition of a β-agonist bronchodilator to an inhalation therapy can reduce asphyxia and improve patients’ quality of life19. Additionally, this group of bronchodilators can help dilute mucus, control the bronchoconstriction of the respiratory tract, and maximize mucociliary clearance5,14.
In spite of the administration of inhalation therapy, some pneumonic cases in this research project resulted in longer treatment durations. This may happen when patients are at a very young age. Infants, especially those under six months old who suffered from respiratory tract edema and inflammation, were more prone to respiratory disorders because infants have smaller respiratory tract diameters, and this may extend the time required to treat their diseases20. Other factors that may affect to the duration of treatment of pneumonic children are the number of leucocytes and the type of antibiotics prescribed.
Innovations in the diagnosis and treatment of pneumonia are required to overcome this leading cause of death among children under five years old. Almost all deaths caused by pneumonia afflicting children can be prevented through more accurate diagnoses and appropriate treatments, as well as providing more skillful health workers in greater numbers21.
Additionally, appropriate and effective therapy for pneumonic children can reduce their length of hospital stay, prevent nosocomial infections and thus shorten treatment duration, prevent recurrent infections in children, and reduce the costs of hospital treatment. Appropriate therapy also offers significant benefits to the hospital. It can reduce the costs of treatment and increase the hospital's reputation due to the patients’ and their families’ improved satisfaction with the quality of the service provided during the patients’ treatment at the hospital.
The results showed that pneumonic children who received inhalation therapy experienced shorter treatment durations than those who did not receive any inhalation therapy. Nurses, as professional health workers who take charge of patients during their treatment at hospitals, are expected to provide accurate explanations of their patients’ conditions so that the patients can receive appropriate and effective treatment for their health problems.
The limitations of this research include the researchers’ inability to perform a direct examination of the patients’ specific conditions during treatment due to the secondary data used in this study. Thus, the researchers were unable to generate a classification of each patient's pneumonic types.
The results of this study can be used to create guidelines for providing more effective health and nursing services, especially in the administration of respiratory tract clearance procedures. These results are also expected to serve as an example of evidence-based practice for the development of the science of nursing and as scientific proof that inhalation therapy offers significant benefits for the treatment of pneumonic children.
We would like to extend our thanks to the Heads of the Medical Record Room and Children's Ward of the P3 Regional Hospital, West Lombok Regency, West Nusa Tenggara Province; the research assistants, and the Department of Research and Community Services, Universitas Indonesia.
Conflicts of interestThe authors declare no conflicts of interest for this study.