Chronic wounds are one impact of cancer cell growth that may cause discomforts or pain. This study aimed to identify the relationship between pain, stress, and sleep quality in cancer patients with a chronic wound. We used a cross-sectional design with 76 patients from a cancer hospital in Jakarta, Indonesia. The instruments used were the Numeric Rating Scale, the Questionnaire on Stress in Cancer Patients, Revised 23, and the Pittsburgh Sleep Quality Index. The results of this study showed that moderate-severe pain produced a higher than average amount of stress (58.86), while patients with no pain or only mild pain had a lower than average stress level (52.3). The results indicated that there was a relationship between pain before analgesic usage, pain during bandage replacement, pain that occurred at night, and stress (p=0.003, 0.007, and 0.002, respectively; α=0.05). Patients who had poor sleep quality experienced above average stress (56.3), while those with good sleep quality reported below average stress levels (45.6). These results indicated that there was a relationship between stress and sleep quality (p=0.033; α=0.05). Poor quality sleep is more common in patients with a moderate to severe pain scale rating (93.1%). However, Fisher's exact test results found that there was no relationship between pain and sleep quality (p=0.301; α=0.05). The results of this study concluded that stress can affect pain and sleep quality, but the pain did not have a direct effect on sleep quality in chronic wound patients.
There were 300 of 100,000 new cancer cases around the world and 195 of 100,000 deaths due to cancer1. Ineffective cancer treatment often leads to complications, including wounds due to the rupture of a cancerous mass. Cancer wounds may produce physical complaints, such as pain, odors, inflammation, edema, and an irregular shape of the wound2. Pain causes physical discomfort and psychological disorders, such as sleep disturbances, a decreased appetite; a lack of concentration, impaired interpersonal relationships, anxiety, depression, and decreased activities of daily living3. Research that focuses on cancer wounds is still limited in Indonesia.
Therefore, this study set out to determine the association between physical and psychological discomfort: pain and stress with sleep quality in malignant wound patients at the Dharmais Cancer Hospital in Jakarta, Indonesia.
MethodThis study used a cross-sectional design with a sample of 76 patients and was conducted at Dharmais Cancer Hospital. The respondents were chosen using a consecutive sampling method; the main inclusion criteria were people over the age of 20 who had a cancerous wound. The data collection procedure began with an explanation about the purpose of the study and a request for the respondent's participation in the study. This investigation used the Numeric Rating Scale (NRS) of pain intensity to determine the severity of their pain, the Questionnaire on Stress in Cancer Patients, Revised 23 (QSC-R23) to assess patients’ stress level, and the Pittsburgh Sleep Quality Index (PSQI) to measure their sleep quality.
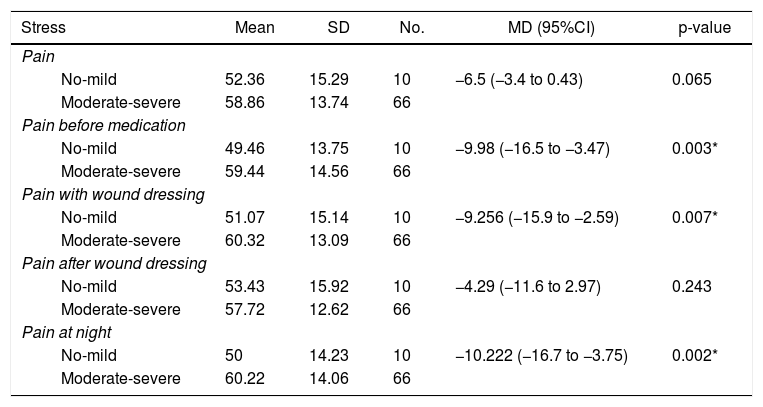
ResultsOur results (Tables 1 to 3) revealed that the average stress score of respondents who suffered from moderate to severe pain was high at 58.86 (SD: 13.74). However, the analysis showed that there was no significant relationship between pain and stress (p=0.065; α=0.05).
Association between pain and stress.
| Stress | Mean | SD | No. | MD (95%CI) | p-value |
|---|---|---|---|---|---|
| Pain | |||||
| No-mild | 52.36 | 15.29 | 10 | −6.5 (−3.4 to 0.43) | 0.065 |
| Moderate-severe | 58.86 | 13.74 | 66 | ||
| Pain before medication | |||||
| No-mild | 49.46 | 13.75 | 10 | −9.98 (−16.5 to −3.47) | 0.003* |
| Moderate-severe | 59.44 | 14.56 | 66 | ||
| Pain with wound dressing | |||||
| No-mild | 51.07 | 15.14 | 10 | −9.256 (−15.9 to −2.59) | 0.007* |
| Moderate-severe | 60.32 | 13.09 | 66 | ||
| Pain after wound dressing | |||||
| No-mild | 53.43 | 15.92 | 10 | −4.29 (−11.6 to 2.97) | 0.243 |
| Moderate-severe | 57.72 | 12.62 | 66 | ||
| Pain at night | |||||
| No-mild | 50 | 14.23 | 10 | −10.222 (−16.7 to −3.75) | 0.002* |
| Moderate-severe | 60.22 | 14.06 | 66 | ||
Association between pain and sleep quality.
| Variable | Sleep quality | Total | p-value | |
|---|---|---|---|---|
| Good, no. (%) | Bad, no. (%) | |||
| Pain | ||||
| No-mild | 8 (17) | 39 (83) | 47 (100) | 0.301 |
| Moderate-severe | 2 (6.9) | 27 (93.1) | 29 (100) | |
| Pain before medication | ||||
| No-mild | 7 (20) | 28 (80) | 35 (100) | 0.172 |
| Moderate-severe | 3 (7.3) | 38 (92.7) | 41 (100) | |
| Pain with wound dressing | ||||
| No-mild | 7 (15.6) | 38 (84.4) | 45 (100) | 0.514 |
| Moderate-severe | 3 (9.7) | 28 (90.3) | 31 (100) | |
| Pain after wound dressing | ||||
| No-mild | 8 (15.7) | 43 (84.3) | 51 (100) | 0.482 |
| Moderate-severe | 2 (8) | 23 (92) | 25 (100) | |
| Pain at night | ||||
| No-mild | 7 (17.5) | 33 (82.5) | 40 (100) | 0.317 |
| Moderate-severe | 3 (8.3) | 33 (91.7) | 36 (100) | |
For participants with moderate to severe pain, the average stress score was higher during wound care activities (60.32; SD: 13:09). There was a significant relationship between pain during wound care and the patient's stress level (p=0.007; α=0.05).
In regards to the relationship between pain following wound care and stress level, respondents reported a moderate to severe pain score (57.72, SD: 12.62). However, the analysis showed that there was no significant relationship between pain after wound care and stress level (p=0243; α=0.05).
The average stress score of respondents who reported moderate to severe pain was higher at night (60.22, SD: 14.06). The analysis showed that there was a significant relationship between pain at night and stress level (p=0.002; α=0.05).
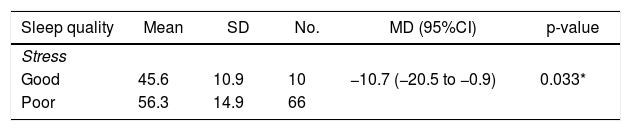
Our investigation revealed that the average stress score of respondents with poor sleep quality was high (56.3, SD: 14.9) here was a significant association between stress level and sleep quality (p=0.033; α=0.05).
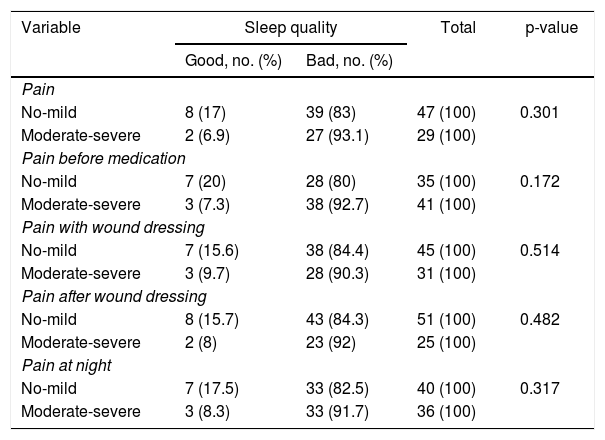
Poor sleep quality was more frequently experienced by the respondents who suffered from moderate to severe pain. The percentage of participants with poor sleep quality, who also reported moderate to severe pain, was 93.1%. Only 6.9% of the respondents reported moderate to severe pain but still experienced good sleep quality. There was no significant relationship between pain and sleep quality (p=0.301; α=0.05).
Before taking pain medication, 92.7% of the respondents who suffered from moderate to severe pain experienced poor sleep quality. Only 7.3% of the participants with moderate to severe pain still had good sleep quality. Our analysis indicated that there was no significant relationship between pain and sleep quality (p=0172; α=0.05).
Poor sleep quality was commonly experienced by respondents who suffered from moderate to severe pain and was as high as 90.3%. Only 9.7% of patients with moderate to severe pain had good sleep quality. There was no significant relationship between pain and sleep quality (p=0514; α=0.05).
After the wound dressings were changed, poor sleep quality was often experienced by the respondents who suffered from moderate to severe pain. Only 8% of participants, who reported moderate to severe pain, still had good sleep quality. The analysis showed that there was no significant relationship between pain and sleep quality (p=0.482; α=0.05).
For the condition of pain at night, 91.7% of the respondents who reported poor sleep quality suffered from moderate to severe pain. Only 8.3% of the patients with moderate to severe pain experienced good sleep quality. The analysis showed that there was no significant relationship between pain with sleep quality (p=0.317; α=0.05).
DiscussionThe respondents with cancer wounds often suffered from physical discomfort symptoms, including pain. Pain induced by cancer sores is precipitated by the infiltration of tumor cells, the effects of treatment, and replacements of wound dressings that are not appropriate2. The questionnaire results revealed that respondents with cancer wounds suffered pain with an average score of 3.61 (SD: 2.472). Pain experiences can vary widely, so the perceived pain will often be different at night, during wound dressing procedures, after wound dressing procedures, and before taking pain medication. The experience of moderate to severe pain frequently occurred before the respondents took a pain killer and also at night.
According to Desen's theory, stress may cause increased pain. Because people often think deeply about particular problems at night before going to bed, this increased stress at bedtime may also increase the pain intensity at night4. This factor affected the results of this study, where the average pain at night was quite high.
Respondents also experienced stress, with an average total stress score of 54.89; 30.3% experienced severe stress. Increased emotional reactions affect the immune and hormonal systems of the body and eventually lead to the development of cancer cells5. This theory about stress from Desen was consistent with the results of studies that showed an association between the stress level and pain before taking pain medication, during wound dressing procedures, and at night (p=0.003, 0.007, 0.002, respectively; α=0.05).
Stress can cause physiological and psychological disturbances, including sleep disorders3. The theory was supported by the results of this study, which found an association between stress and sleep quality (p=0.033; α=0.05). Stress could be a trigger for anxiety, which stimulates the sympathetic nervous system and alters the stages of REM and NREM sleep by activating norepinephrine3.
A study of 258 hospitalized patients found a relationship between depression and sleep quality (p < 0.001). Stressful conditions may be triggered by environmental factors, social support, and the coping strategies of each individual6.
Pain may cause physical discomfort, which often produces a decline in the quality of sleep3. Our results showed that 86.8% of respondents reported poor sleep quality. These patients suffered from a higher intensity of pain than the respondents who had good sleep quality. However, there was no significant relationship between sleep quality and pain before taking drugs, during wound dressing procedures, after wound dressing procedures, or at night (p=0.172, 0.514, 0.482, 0.317 respectively; α=0.05).
A previous study that included 2635 respondents showed that 62.6% of cancer patients who experienced pain had poor sleep quality (p <0.01)7. Another investigation of 214 cancer patients who underwent treatment produced similar results; there was no relationship between pain and sleep disturbances (p=12:26; α=0.05)8. Sleep quality is not only influenced by the presence of pain; a decline in the quality of sleep may also be affected by increasing age, stress level, and environmentally induced inconveniences.
The researchers concluded that an increased intensity of pain may lead to poor sleep quality in certain individuals. However, there was no significant correlation between pain and sleep quality in this study. These results may be influenced by a particular determinant, such as one's perception of and ability to express pain and also sleep disorders caused by various factors, such as the environment, waking at night to urinate, the effects of pain medications, and time shifting of the sleep-wake cycle, which all could lead to a decline in sleep quality.
The differences in perceived pain may also be influenced by cultural factors and an individual's adaptability to the pain experience. According to Roy's adaptation theory, each individual has a dissimilar capacity for adaptability. The ability of individuals to maintain their health depends on their ability to adapt to various stimuli. The adaptation rate is also influenced by a person's coping mechanisms. Therefore, individuals with good coping mechanisms, should also have the ability to adapt positively to pain stimuli.
Culture may also affect the way a person tolerates and interprets pain9. The Javanese culture tends to accept pain without much complaint. The results of this study indicated that the majority of respondents came from Java. As a result, the average pain intensity was not rated too high and was still classified as mild pain. However, although most respondents in this study experienced mild pain, the degree of pain was actually not relevant because the majority of respondents (86.8%) still reported poor sleep quality.
In addition, our study was performed only in outpatient settings where the level of pain and sleep disorders will be perceived differently by patients in the wards. These results led to the absence of a significant correlation between pain and sleep quality in patients with cancer wounds at Dharmais Cancer Hospital in Jakarta, Indonesia.
ConclusionsThe results showed an absence of a relationship between pain and sleep quality in patients with a cancer wound. However, there was an association between pain and stressful conditions, as well as stressful conditions and sleep quality. These results indicated that pain impacts the psychological condition, producing stress that may lead to a decreased quality of sleep. However, the relationship between pain and sleep quality was not directly correlated because of the impact of stress; no correlation was identified between pain and quality of sleep.
RecommendationThis study suggests that other researchers develop studies for inpatient and outpatient settings to compare certain variables, such as pain intensity, stress levels, the use of analgesic drugs, the environment, and sleep quality, patients in inpatient and outpatient facilities. The researchers also propose an investigation into stress and sleep quality in patients with cancer wounds.
The researchers would like to thank PITTA Universitas Indonesia for its generous contribution of funding for this research study.