Identify sleep quality and related factors in patients with diabetic ulcer.
MethodThis research design used cross sectional study with a sample of 97 diabetic ulcer patients in a clinic wound care. The research instruments consist of Perceived Stress Scale (PSS) to assess the stress level, and the Pittsburgh Sleep Quality Index (PSQI). Questionnaire to identify the sleep quality.
ResultsThe results showed that there was a significant difference between subjective sleep quality and sleep quality measured using PSQI (p: 0.001). Factors that affected sleep quality were income (p: 0.014), stress levels (p: 0.001), medications (p: 0.026), pain levels (p: 0.048), and diet (p: 0.009).
ConclusionThe results of this study indicate that the importance of conducting sleep quality assessment with the associated factors is to overcome the sleep problems in diabetic patients.
The prevalence of diabetes mellitus increases over years. American Diabetes Association, showed in 2012, 29,100,000 people or 9.3% of US populations suffer from diabetes mellitus, in which 1.25 million adolescence and adult suffers from type 1 diabetes mellitus.1 The basic health research in Indonesia, Riset Kesehatan Dasar (Rikesdas) in 2013 showed that 6.9% of the population or 12,191,564 people suffers from TGT, and 3.6% of the population or 64,668,297 people suffers from GDP, with the total population of 176,689,336.2 Moreover, the prevalence of diabetic ulcer in Indonesia was up to 15% of the population, with the number of amputation was approximately 30% and the number of mortality was to 32%.3
Similar research reported that diabetic ulcer occurs in 14.3% of 581 patients with diabetes mellitus.4 Diabetic foot ulcer is the most common type of the treatment given by hospital for patients with diabetes mellitus, with the percentage of 80%. The diabetic ulcer condition cause a sleep disorder related to the stress level due to their illness. The sources of the patients’ stress with diabetic ulcer are psychological burden of their illness, the lack of support from their family, environment, treatment adherence, and the limitation of physical activity.5
The research conducted by Howell et al. showed that approximately 25%–29% patients with chronic illness (cancer) suffers from insomnia which resulted in a decreasing sleep quality. Researches on sleep quality in chronic illness patient, especially in diabetic ulcer, are few.6 Moreover, research that compare sleep quality in PSQI with subjective sleep quality in the ninth question on PSQI, as well as factors affecting sleep on patients with diabetic ulcer has not been studied. Therefore, this research aimed to identify the subjective sleep quality and the affecting factors in patients with diabetic ulcer.
MethodIn this study, a quantitative research with a simple, descriptive research design using cross-sectional method was performed. The sample of this research constitutes of 97 patients with diabetic ulcer that was taken using Purposive Sampling technique. The instrument to collect data in this research consisted of the patients’ characteristics, Perceived Stress Scale (PSS) to assess the stress level, and The Pittsburgh Sleep Quality Index (PSQI) to identify the sleep quality
ResultsThe duration of the wounds in respondents with diabetes mellitus is 1–30 years, while the duration of the wounds in respondents with diabetic ulcer is 1–72 months (Table 1).
The result shows that the average age of patients with diabetic ulcer is 54.84 (95% CI: 53.13–56.54) with standard deviation of 8484. Meanwhile, the average duration of patients having diabetes mellitus is 9.21 years (95% CI: 7.63–10.78) with standard deviation of 7.825 and the average duration of patients with diabetes mellitus that suffers from wound is 5.54 months (95% CI: 3.76–7.31) with standard deviation of 8.769 (Table 2).
Factors affecting sleep.
| No. | Characteristic | N (%) | No. | Characteristic | N (%) |
|---|---|---|---|---|---|
| 1 | Age | Upper middle income | 26 (26.8) | ||
| <60 years old | 64 (66) | 5–10 million | 15 (15.5) | ||
| ≥60 years old | 33 (34) | >10 million | 11 (11.3) | ||
| 2 | Sex | 5 | Comorbidity | ||
| Female | 54 (55.7) | Yes | 47 (48.5) | ||
| Male | 43 (44.3) | None | 50 (51.5) | ||
| 3 | Education | 6 | Ulcergrade | ||
| Low-level education | 41 (42.3) | Superficial wound | 20 (20.6) | ||
| No education | 8 (8.2) | Grade 0 | 0 | ||
| Elementary school | 20 (20.6) | Grade 1 | 20 (20.6) | ||
| Junior high school | 13 (13.4) | Deep wound | 77 (79.4) | ||
| Higher-level education | 56 (57.7) | Grade 2 | 49 (50.5) | ||
| Senior high school | 31 (32) | Grade 3 | 24 (24.7) | ||
| Tertiary education | 25 (25.8) | Grade 4 | 3 (3.1) | ||
| 4 | Income | Grade 5 | 1 (1.0) | ||
| Lower middle income | 71 (73.2) | 7 | Random blood glucose | ||
| <1 million | 11 (11.3) | Normal | 47 (48.5) | ||
| 1–3 million | 21 (21.6) | Diabetic | 50 (51.5) | ||
| 3–5 million | 65 (67) | ||||
| 8 | Sleep habits | Other habits | |||
| Sound | Yes | 20 (20.6) | |||
| Loud | 27 (27.8) | None | 77 (79.4) | ||
| Quiet | 70 (72.2) | 9 | Insulin | ||
| Lighting | Oral insulin | 72 (74.2) | |||
| Light | 35 (36.1) | Injected | 25 (25.8) | ||
| Dim | 21 (21.6) | 10 | Diet | ||
| Dark | 41 (42.3) | None | 60 (61.9) | ||
| Temperature | Sleep-inducing | 12 (12.4) | |||
| Warm | 4 (4.1) | Sleep-preventing | 25 (25.8) | ||
| Moderate | 45 (46.4) | ||||
| Cold | 48 (49.5) | ||||
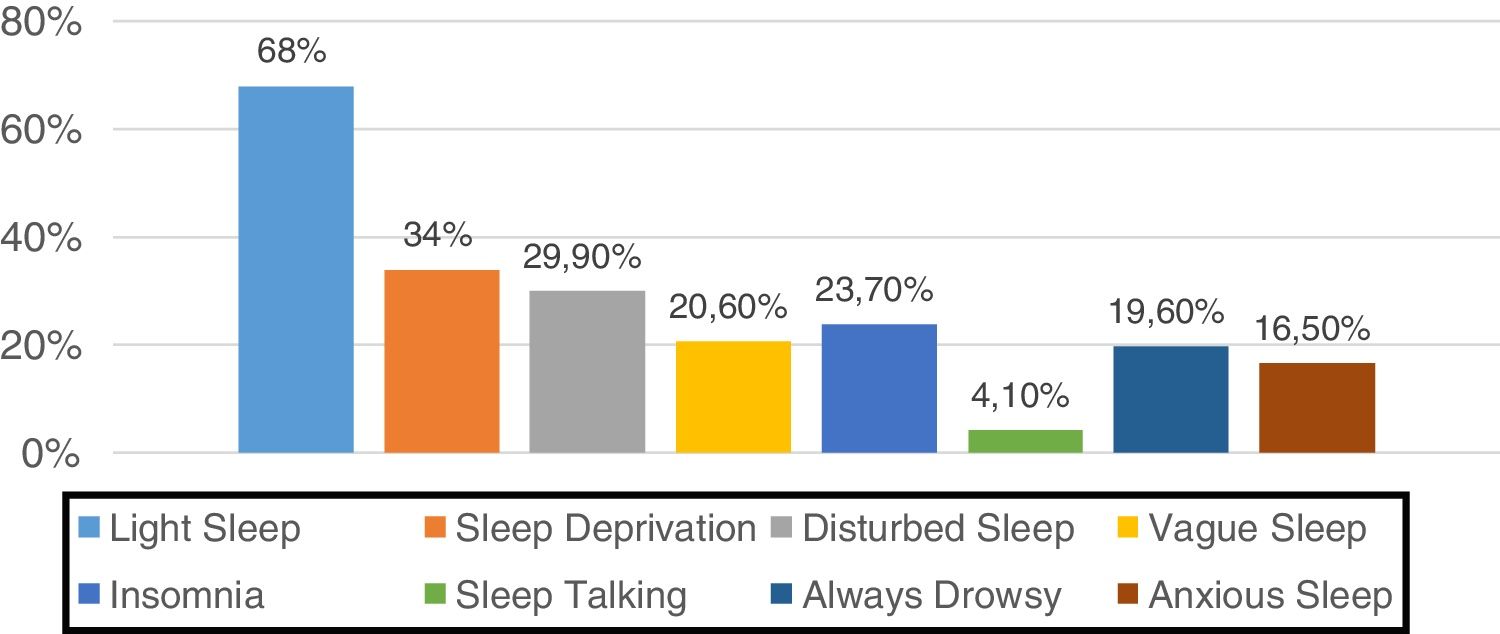
Patients with diabetic ulcer suffered from various sleeping disorder due to their disease. Below is the graph displaying the frequency of sleeping disorder that occurs in patient with diabetic ulcer (Fig. 1).
The result showed that the most common sleeping disorders in patients with diabetic ulcer was disrupted sleeping patterns due to repetitive awakening, lack of sleep, and not soundly sleep. Meanwhile, other sleeping disorders only occur in few respondents (Table 3).
Comparison between Subjective Sleep Quality and Sleep Quality (PSQI).
| Sleeping Quality | Level of quality | N (%) | X2 | Margin value | |
|---|---|---|---|---|---|
| Good | Bad | ||||
| Subjective | 81 (84) | 16 (16) | 97 (100) | 8.320 | 0.001* |
| PSQI | 2 (2) | 95 (98) | 97 (100) | ||
According to the ninth question in PSQI questionnaire (sleep perception), it was found that most of the respondents stated that they had a good sleep quality (83.5%), while the other result of the measurement using the comprehensive PSQI showed that most patients had a low sleep quality (97.9%). Thus, this research showed that there were discrepancies between sleep quality that the patients express (subjective sleep quality) and the comprehensive sleep quality based on PSQI. The result reported a significant disparity between subjective sleep quality and comprehensive sleep quality (PSQI) (p: 0.001, α: 0.05) (Table 4).
Relationship between factors and sleep quality.
| No. | Variable | Sleep quality | Total (%) | X2 | p value | |
|---|---|---|---|---|---|---|
| Good N (%) | Bad N (%) | |||||
| 1 | Age | |||||
| <60 years old | 52 (81.2) | 12 (18.8) | 64 (100) | 0.297 | 0.586 | |
| ≥60 years old | 29 (87.9) | 4 (12.1) | 33 (100) | |||
| 2 | Sex | |||||
| Male | 35 (81.4) | 8 (18.6) | 43 (100) | 0.050 | 0.823 | |
| Female | 46 (85.2) | 8 (14.8) | 54 (100) | |||
| 3 | Education | |||||
| Low level | 33 (80.5) | 8 (19.5) | 41 (100) | 0.167 | 0.683 | |
| Higher level | 48 (85.7) | 8 (14.3) | 56 (100) | |||
| 4 | Income | |||||
| Lower-middle | 22 (68.8) | 10 (31.2) | 32 (100) | 6.034 | 0.014* | |
| Upper-middle | 59 (90.8) | 6 (9.2) | 65 (100) | |||
| 5 | Comorbidity | |||||
| Yes | 39 (78) | 11 (22) | 50 (100) | 1.521 | 0.218 | |
| None | 42 (89.4) | 5 (10.6) | 47 (100) | |||
| 6 | Ulcergrade | |||||
| Superficial wound | 19 (95) | 1 (5) | 20 (100) | 2.417 | 0.180 | |
| Deep wound | 42 (89.4) | 15 (19.5) | 77 (100) | |||
| 7 | Random blood glucose | |||||
| Normal | 40 (85.1) | 7 (14.9) | 47 (100) | 0.019 | 0.89 | |
| Diabetic | 41 (82) | 9 (18) | 50 (100) | |||
| 8 | Sleeping habits | |||||
| Sound | ||||||
| Loud | 20 (74.1) | 7 (25.9) | 27 (100) | 2.416 | 0.136 | |
| Quiet | 61 (87.1) | 9 (12.9) | 70 (100) | |||
| Lightning | ||||||
| Light | 30 (85.7) | 4 (14.3) | 35 (100) | 0.024 | 0.876 | |
| Dim-dark | 51 (82.3) | 11 (17.7) | 62 (100) | |||
| Temperature | ||||||
| Hot–moderate | 38 (77.6) | 11 (22.4) | 49 (100) | 1.750 | 0.186 | |
| Cold | 43 (89.6) | 5 (10.4) | 48 (100) | |||
| Other habits | ||||||
| Yes | 14 (70) | 6 (30) | 20 (100) | 3.336 | 0.091 | |
| None | 66 (86.8) | 10 (13.2) | 77 (100) | |||
| 9 | Insulin | |||||
| Oral insulin | 64 (88.9) | 8 (11.1) | 72 (100) | 5.879 | 0.026* | |
| Injected | 17 (68) | 8 (32) | 25 (100) | |||
| 10 | Diet | |||||
| Sleep-inducing | 7 (58.3) | 5 (41.7) | 12 (100) | 8.467 | 0.09* | |
| Sleep-preventing | 24 (96) | 1 (4) | 25 (100) | |||
The statistic test showed that sleeping quality has a significant relationship with income (p: 0.014), stress level (p: 0.001), medication (types of insulin) (p: 0.026), level of pain (p: 0.048), and diets before sleep (p: 0.09) (Table 5).
The study's result showed that there was a significant relationship between the pain level (p: 0.048) and stress (p: 0.001) with subjective sleep quality that is expressed by patients with diabetic ulcer.
DiscussionThe result of this research showed that majority of the respondents stated that they had a good quality of sleep (83.5%). However, using PSQI questionnaire, this research found that most respondents have a low level quality of sleep (97.9%), it was concluded that most respondents state that the quality of their was good even though the overall result shown by PSQI questionnaire, most respondents had a low quality of sleep. The analysis found that there was a significant difference between subjective sleep quality (patient perception) in the ninth number of PSQI and the sleeping quality measured by comprehensive PSQI questionnaire (p: 0.001).
Patients with chronic illness require psychology adaptation. A study reported the importance of cognitive factor, behavior, and social in facilitating this adaptation during treatment and giving psychosocial interference toward patients.7 The experience of having disease affect the physiology adaptation along with the changes in psychology adaptation.7 That research showed that psychosocial interference can improve indicator in psychology and physiology adaptation in patients with chronic illness. Analysis from Schwartz research stated that psychology adaptation occurs due to the fact that patients feel stuck in their disease, and therefore some patients express their negative feeling (such as anger, fear, and pressured), but the emotional stage appears in an early detected disease, or when it was known as the first stage of disease acceptance.8
The disease acceptance will increase with the help of support system such as families, and friends that encourage the patient to be more active in doing their activities.8 The condition may affect the patient adaptation to the disease, which results in disease acceptance and adaptation so that the patient will have more positive thought that could affect their physical needs, such as rest and sleep.
Therefore, illness adaptation causes the disparity between subjective sleep quality according to patient perspective with the sleep quality that is comprehensively tested using PSQI, in which the majority of patients are used to their own sleep quality that they experienced during their illness.
The analysis showed that there was no significant relationship between the age of respondents and the sleep quality (p: 0.586). Similar study also showed that there was no significant relationship between age and sleep quality in patients with cancer wound (p: 0.183).9 However, a different study reported a significant relationship between age and sleep quality in 130 patients with rheumatoid (p: 0.006).10 The increasing of age may influence the rest and sleep pattern.
Moreover, the study's result showed that there was no significant relationship between the respondent gender and sleep quality (p: 0.823). A research reported that how gender can be a risk factor in sleeping problems. National Sleep Foundation mentioned that the risk factor of insomnia often exists in elderly and female.11 Female experiences decreasing in sleep quality that is related to hormonal changes, such as menstruation, pregnancy, and menopause.
The research results revealed that the patient's level of education did not have a significant influence in sleep quality (p: 0.683). A low quality of life had a significant relationship with low level of education.12 Education play an important factor in affecting patients’ knowledge that is related to their behavior to avoid the disease complications
The analysis showed that income has a significant relationship with sleep quality (p: 0.014). A research conducted by Isa and Baiyewu reported that a low income has a significant relationship with patients’ quality of life with diabetic ulcer.13 Similar research by Gautam et al. also shows that a low level of life quality has a significant relationship with low economic social status and low level of education.12
This research analysis reported that comorbidity existing within the patient with diabetic ulcer does not have a significant relationship with sleep quality (p: 0.218). However, another research showed the impact of heart disease with sleep quality, in which approximately 28% of patients with heart disease has a low sleep quality.14 However, a different study revealed that there is no significant relationship between hypertension and sleep quality.15
Furthermore, the research analysis showed that the ulcer grade has no significant relationship with sleep quality (p: 0.180). Similar research by Niranjan et al. displayed a meaningful relationship between the wound degree and patients’ quality of life with diabetic ulcer.16 The wound condition can cause a discomfort feeling that will influence patients’ life pattern, including sleeping.
Another study's results showed that there is no significant relationship between Random Blood Glucose score and sleep quality (p: 0.224). However, Tarihoran et al. stated that there is a significant relationship between the blood sugar concentration with patients sleep quality (p: 0.036).17 This research showed that 56.7% patients have blood sugar concentration above normal. Another research explained that the high level of blood sugar concentration in patients with diabetes mellitus may cause sleep disorder related to nocturnal condition.18 That condition can cause patient easily to be awaken during nighttime to urinate. Thus, the sleeping time will be disrupted which influences sleep quality.
This research showed significant relationship between sleeping habit (voice, lighting, temperature) and sleep quality (p>0.05). The patients’ sleeping quality can be influenced by patients sleeping habit, such as noise, temperature, and lighting.11 Potter and Perry stated that some patients are having sleeping disorder related to temperature that are too hot or too cold, or unsuitable lighting.19
This study's results explained that the level of stress and anxiety has a significant relationship with sleep quality (p: 0.001). This is similar with a research conducted by Fauziyah and Gayatri that found a significant relationship between the level of stress and sleep quality (p: 0.033).9 Restless thought, stress, and anxiety due to the illness can influence the individual’ capacity to have a good rest as it causes muscle tension. Sleeping difficulties can be affected by anxiety and negative thought that is related to physical situation, as well as the anxiety of the foot condition that has to be amputated, to the anxiety of the illness that cannot be cured.20 Similar research showed that in 258 inpatients respondents, there is a significant relationship between depression and sleep quality (p<0.001).15
The use of insulin (oral or injected) has a significant relationship with sleep quality (p: 0.026). A research conducted by Vatankhah et al. showed that injected topical insulin can significantly increase the process of wound healing.21 The research showed that the use of injected insulin has more side-effects compared to oral insulin which influences the patients’ sleep qualities.
Moreover, the research analysis also showed the level of pain that has a significant relationship with sleep quality (p: 0.048). Increasing the severity of ulcer condition can cause disruption in rest and sleep patterns due to the pain that the patients feel.20 A research mentioned that diabetic ulcer pain and the long period of wound healing can cause sleeping disorder that creates feeling discomfort that influence the patients’ quality of life.22
Lastly, the study revealed that type of diet also has a significant relationship with sleep quality (p: 0.009). Several types of food could influence the quantity and quality of sleep. Food products that are high in caffeine, such as coffee, cola, and chocolate, function as stimulant that affects natural pattern of sleep.23
Based on the research it is concluded that individual perception regarding sleep quality has a disparity with the measurement of comprehensive sleep quality using The Pittsburgh Sleep Quality Index (PSQI). This condition is influenced by the recovery process of the illness that occurs for a long period of time. The long period of time allows the patients to feel accustomed to their condition. Thus, patients with diabetic ulcer state that they have a satisfactory sleep quality, even though PSQI measurement shows otherwise.
This research mentioned a significant relationship between affecting factors; income, stress, insulin type, and pain with sleep quality. Therefore, the information from this study can be used to develop knowledge related to factors that affect sleep, as well as to increase the quality of services in giving intervention toward patient by emphasizing on comfort. Moreover, it is important to stress the urgency of doing analysis on sleep quality by examining affecting factors to solve the sleep problems in patients with diabetic ulcer.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2017 funded by DRPM Universitas Indonesia No. 374/UN2.R3.1/HKP.05.00/2017.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.