To find out how important discharge planning program influence of satisfaction and independency stroke patients due to hypertension. Discharge planning is important for continuity of care and treatment during the patient hospitalized and after going home.
MethodThis study Quasi-experimental method was used, pre and post-test for control group and intervention group with 160 respondent, 33 respondent pre and post 33 respondent for control group, and 33 respondent pre and 37 respondent post for intervention group, then 24 respondent observed start from hospitalized until discharge from hospital for patient independency.
ResultsThe result of the study show that the satisfaction compares between control group meaningless significant, but satisfaction compare pre and post-test between intervention group very strong significant, but while comparing between control and intervention group, it does not significant. Meanwhile, patient independency strong significant while discharge planning programs applied.
ConclusionsIt is concluded that discharge planning is necessary to be implemented for stroke patient and used by the healthcare team to perform the care and treatment.
Discharge planning is a sustainable healthcare process in transferring patients from one health facility to another. According to Kozier discharge planning is a process where patients provided with initial treatment followed with nursing treatment, both in the sense of their healing process and in maintaining their healthy status,1 and Brenda stated that discharge planning is a process in which patients are assisted to make proper treatment plans to be used in current health facilities or to help them to take care of themselves, and its including situations where patients receiving treatments from health facilities in their neighborhood.2 The goal of discharge planning is to ensure the continuity of patient's care which prepared from the moment the decision to receive hospital treatment was made until the patient returned home or to the environment where they reside.3
Discharge planning has been applied since the very moment the patient start to receive treatment from the hospital. This was made clear by Birjandi and Bragg stated that discharge planning had been applied during the first 24h of hospitalization of patients, to determine patients’ needs during they stay.4 In this period, patients’ needs that have to be considered and prepared when they returned home or moved to another health facility are determined. The Toronto Central Local Health Interaction Network describes the patient's discharge planning which prepared from the outset will ensure sustainable healthcare while also prevent patients from repeatedly coming to receive treatment and medication for the same complication.5 The discharge planning aims to ensure a sustainable treatment is maintained from the moment the decision to receive treatment were made until the patient returned home or to where they reside. Discharge planning is an interdisciplinary team which provides patients with good service in order to achieve sustainable treatment and medication from the moment they start receiving hospital treatment until they returned home.6
In accordance with this study, a proper and discharge planning will result in (a) helping patients to receive appropriate health care, (b) preventing patients from returning to the hospital with the same complications, (c) is one of the factors related to the quality of the treatment, (d) maximize the effectiveness of hospital services, (e) assist patients to reduce the maintenance costs.7–9 Discharge planning is useful for reducing maintenance costs, avoiding patients with similar complication to repeatedly going back to the hospital, shortening maintenance time, and providing education which adjusted to the patient needs.10 Halstead and Jones also explained the benefits of discharge planning: (1) reducing recurrence rates of the illness; (2) preventing hospitalization and exposure to emergency unit; (3) assisting patients to understand their needs in relation to their treatment and all the costs required, and (4) documentation needs of the patient. Patients and their families would feel satisfied when they receive services that meet their expectations, this also applied for nurses who do the treatment.11
One aspect that makes the patient feel satisfied: the patient relationship with hospital personnel which related to the hospitality and good communication between patients and the personnel in providing all the information required by the patient. This explains hypertensive patients require properly prepared discharge planning12 2007).
Hypertension is a chronic condition which requires sustainable treatment and medication, so control measures are needed to keep the blood pressure in the normal range. Hypertension can be observed from 3 (three) aspects: (a) as a sign, hypertension is a sign of atherosclerotic heart disease (b) as a risk factor, hypertension contributes to the increased atherosclerosis, thickening sediment in blood vessel walls (c) as a disease, hypertension is the main contributor of deaths caused by heart disease, cerebrovascular, kidney, and vascular diseases13,14 WHO report in 2008, the hypertension incidence is ranked 10th as the cause of death in the world, while in Asia it ranked ninth and hypertension shares as the cause of death is 12.8% and in 21st century hypertension has become a major issue of global health problems, and this number will continue to increase.13 Than Murthy, predicted up to the year 2025, the number of hypertension patients is predicted to increase to 29%, or about 1.6 billion people worldwide.14
Hypertensive patients require sustainable treatment and medication since it is diagnosed until further treatment. Proper and sustainable treatment and medication patients with hypertension, whether it is at the hospital or after they returned home, can help them to avoid more severe risks.5 By conducting continuous monitoring and medication to high-risk cardiovascular disease patients aged 55 and older may reduce the risk of myocardial infarction, stroke, and death.3 Patients with hypertension who are hospitalized require support in the form of good service management and nursing treatment including discharge planning.
Prevention and proper discharge planning will lessen the complications, cost-effectiveness, avoid re-hospitalization of the treated patients, and satisfy the patients and their families. It is important to develop the most appropriate model for hypertensive patients. by discovering the contributing factors in discharging planning to be used as a baseline data in the development of the model. Some research on discharge planning is still limited to the functions and benefits of the planning and yet to be focused on the development of a model of discharge planning so that this model can be used as a new approach in providing comprehensive health services in Indonesia.
MethodQuasi-experimental method was used, pre and post-test for the control group and intervention group with 160 respondent, 33 respondent pre and post 33 respondent for the control group, and 33 respondent pre and 37 respondent post for the intervention group, then 24 respondent observed start from hospitalized until discharge from hospital for patient independency. The study was conducted at two private hospitals in different place.
ResultsPatient satisfactionPatient satisfaction was measured by comparing the control group pre and post-intervention, intervention group pre, and post-intervention, and then compare between intervention group and control group, and the result as below.
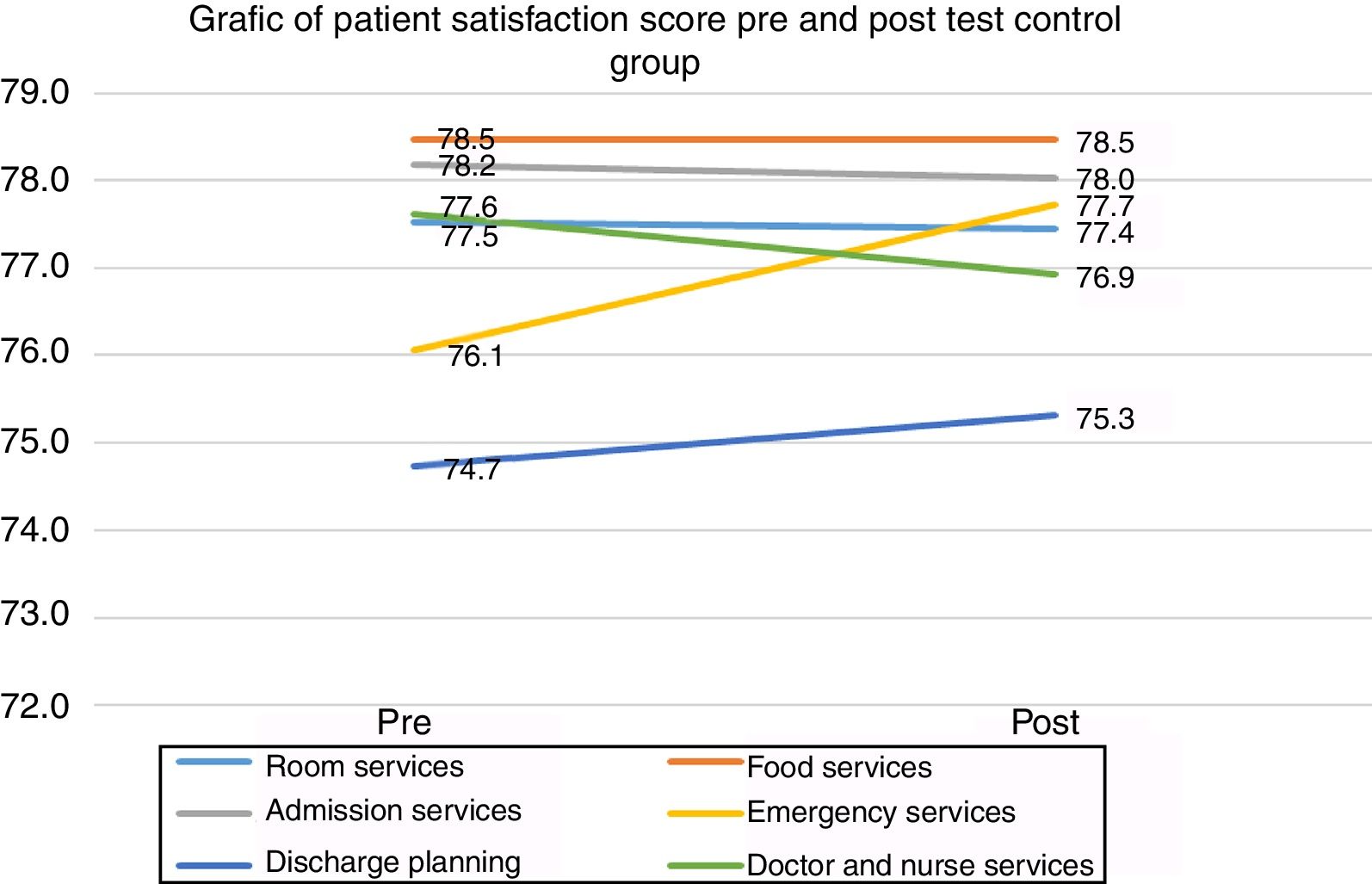
Patient satisfaction pre and post-test control groupThe result between pre and post-test on control group was any differences with room services satisfaction difference (−0.1), but P-value 0.960>P-value 0.05 no significance, food services (0.0), P-value 1.000>P-value 0.05, hospital admission services (−0.2), P-value 0.932>P-value 0.05, emergency services (1.7), P-value 0.425>P-value 0.05, discharge planning process (1.7) P-value 0.676<P-value 0.05, and Doctor and Nurses services difference mean (−0.7), P-value 638>P-value 0.05 do not have significant value. Overall patient satisfaction of Control Group when viewed with P-value 0.883>P-value 0.05, meaningless between pre and post-test the control group, and the detail differences as seen in the following Table 1 and Fig. 1.
Patient satisfaction pre and post test control group.
| Patient satisfaction control group | Pre | Post | Differential | P-value |
|---|---|---|---|---|
| Room services | 77.5 | 77.4 | −0.1 | .960 |
| Food services | 78.5 | 78.5 | 0.0 | 1.000 |
| Admission services | 78.2 | 78.0 | −0.2 | .932 |
| Emergency services | 76.1 | 77.7 | 1.7 | .425 |
| Discharge planning | 74.7 | 75.3 | 0.6 | .676 |
| Doctor and nurse services | 77.6 | 76.9 | −0.7 | .638 |
| Total | 77.1 | 77.3 | 0.2 | .883 |
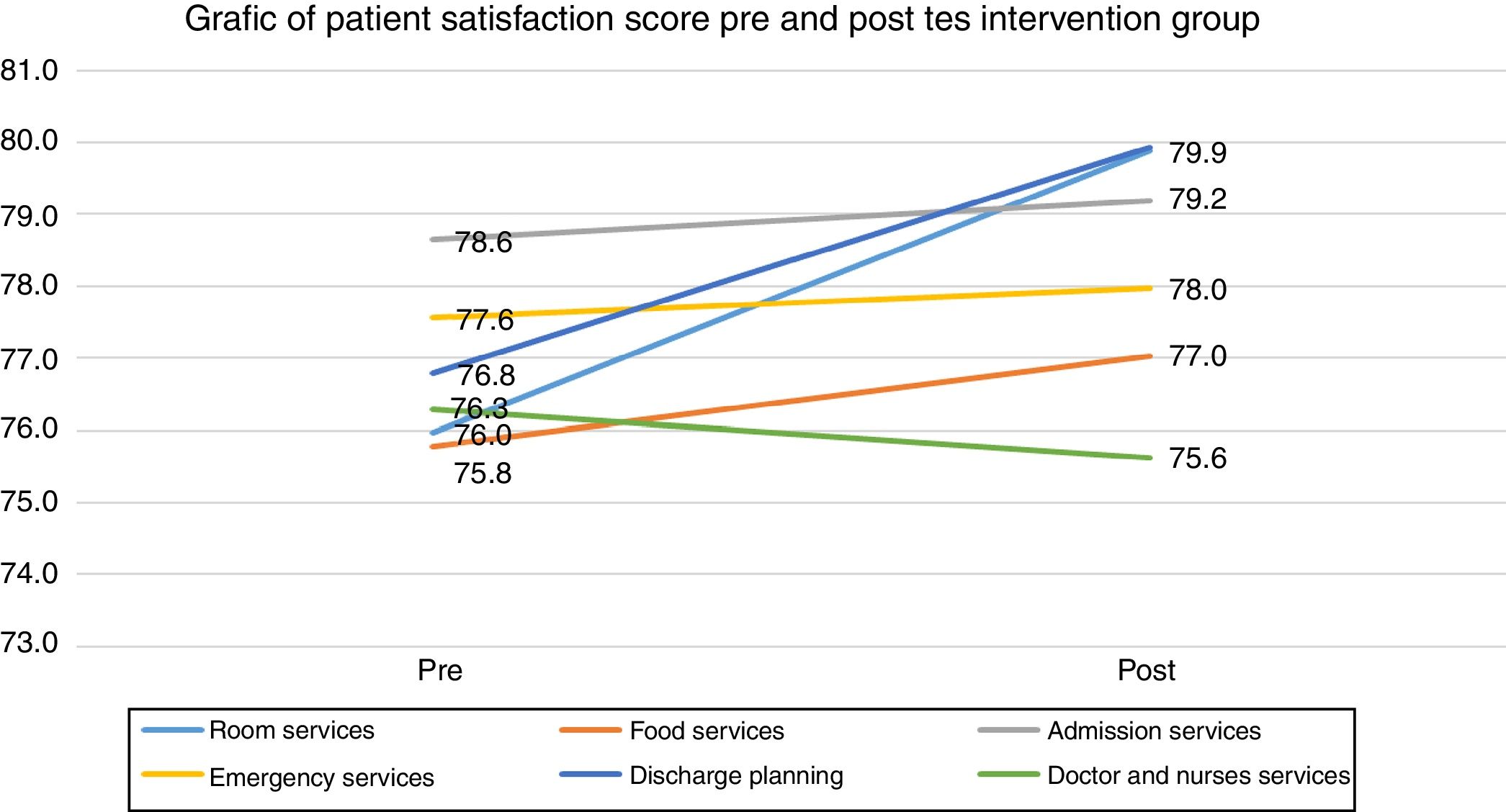
The result between pre and post-test on intervention group was any differences with room services satisfaction difference (3.9), and P-value 0.00<P-value 0.05, have significance, food services (1.3), P-value 0.007<P-value 0.05, hospital admission services (0.5), P-value 0.103>P-value 0.05, emergency services (0.4), P-value 0.324>P-value 0.05, discharge planning process (3.1) P-value 0.676<P-value 0.05, and Doctor and Nurses services difference mean (−0.7), P-value 0.196>P-value 0.05. Do not have significant value. Overall patient satisfaction of intervention group when viewed with P-value 0.00<P-value 0.05, have significance between pre and post-test the intervention group, and the detail differences as seen in the following Table 2 and Fig. 2.
Patient satisfaction intervention group.
| Patient satisfaction intervention group | Pre | Post | Differential | P-value |
|---|---|---|---|---|
| Room services | 76.0 | 79.9 | 3.9 | .000 |
| Food services | 78.5 | 77.0 | 1.3 | .007 |
| Admission services | 78.6 | 79.2 | 0.5 | .103 |
| Emergency services | 77.6 | 78.0 | 0.4 | .324 |
| Discharge planning | 76.8 | 79.9 | 3.1 | .000 |
| Doctor and nurse services | 76.3 | 75.6 | −0.7 | .196 |
| Total | 76.8 | 78.3 | 1.4 | .000 |
The result between intervention and control group Mean was found significant differences with room services satisfaction difference (4.0) P-value 0.019<P-value 0.05, food services (1.3) P-value 0.434>P-value 0.05, hospital admission services (0.7) P-value 0.685>P-value 0.05, discharge planning process (2.6) P-value 0.067<P-value 0.05, and the only in the emergency department (−1.3) and doctors and nurses service (0.0), do not have significant value. Overall patient satisfaction, when viewed with P-value 0.40, >P-value 0.05 meaningless between the control group and the intervention group, and the differences as in the following Table 3.
Patient satisfaction.
| Patient satisfaction | Control differential | Intervention differential | Control and intervention differential | P-value |
|---|---|---|---|---|
| Room condition | −0.1 | 3.9 | 4.0 | .019 |
| Food services | 0.0 | 1.3 | 1.3 | .434 |
| Admission services | −0.2 | 0.5 | 0.7 | .685 |
| Emergency services | 1.7 | 0.4 | −1.3 | .529 |
| Discharge planning process | 0.6 | 3.1 | 2.6 | .067 |
| Docter and nurses services | −0.7 | −0.7 | 0.0 | .993 |
| Total | 0.2 | 1.4 | 1.2 | .400 |
Patients independencies were observed starting from a patient hospitalized. During admission gave them training and education regarding stroke treatment and the end of treatment conduct evaluation regarding patients independency. The evaluation was done for 24 patients, and the result was P-value 0.00<P-value 0.05. The result shows that discharge planning intervention by educating patient is strong significant useful for patient independency. The result showed in Table 4.
Patients independency.
| No. | Instructions | Patients (N=24) | P* | |||
|---|---|---|---|---|---|---|
| Pre (n=24) | Post (n=24) | |||||
| Mean | SD | Mean | SD | |||
| 1 | Sitting to standing | 1.83 | .637 | 2.63 | .824 | 0.00 |
| 2 | Standing unsupported | 1.79 | .721 | 2.79 | .833 | |
| 3 | Sitting with back unsupported bet feet supported on the floor or a stool | 1.88 | .797 | 2.75 | .737 | |
| 4 | Standing to sitting | 1.79 | .658 | 2.63 | .770 | |
| 5 | Moving | 1.75 | .737 | 2.67 | .761 | |
| 6 | Standing unsupported with eyes closed | 1.98 | .751 | 2.71 | .751 | |
| 7 | Standing unsupported with feed together | 1.71 | .624 | 2.46 | .779 | |
| 8 | Reaching forward with outstretched arm while standing | 1.71 | .751 | 2.58 | .776 | |
| 9 | Pick up object from the floor from a standing position | 1.92 | .830 | 2.63 | .824 | |
| 10 | Turning to look behind over left and right shoulders while standing | 1.63 | .576 | 2.21 | .721 | |
| 11 | Turn 360 Degrees | 1.38 | .647 | 2.25 | .737 | |
| 12 | Place alternate foot on step or stool while standing unsupported | 1.58 | .717 | 2.25 | .721 | |
| 13 | Standing unsupported one foot in front | 1.75 | .794 | 2.75 | .737 | |
| 14 | Standing one foot | 1.63 | .875 | 2.71 | .859 | |
Based on the results of the early stages of this study, there are several important points found as the factors contributing to the development of the discharge planning model, hence requiring further discussion to obtain viable solutions in developing the planning model. Because of any gab between existing discharge and expecting discharge planning, such as the initial discharge planning was prepared one day before patients discharge, which supposed to be done before the patient started to hospitalize or within the first 24h after admission and received treatment for unplanned cases.4,15,16
The Discharge Planning Team was not formed to implement discharge planning and its continuous implementation. There should be the case administrator, social workers, service coordinators, evaluators, or patient and family services.4 The hospital management policy has great influence on the implementation of discharge planning as a successful introduction of services require consistent hospital supporting policies. The determinant of patients to be discharged was only by the physician, and yet it should be decided by taking into consideration the suggestions of the discharge planning team. The collective feedback by health team could a positive impact on the patient and his family satisfaction. The collaboration of health personnel is also required for the patient's discharge.16
A good implementation of discharge planning for patients with Congestive Heart Failure (CHF) can lower their recurrent hospitalization rates from 44.2% to 11.4% in six months and increased cost-effectiveness. They are reverted from being charged for the US $ 1541 for every re-visit.8 This statement is supported by research conducted by Bull, Hansen, and Gross on elderly patients with heart failure. Two weeks after their repatriation, 9.5% of the sample was re-hospitalized, and 8.1% returned to the hospital, and after two months it turned out that 20% was re-hospitalized and 18% came back to the emergency unit. Prior the observation, they have conducted pre-assessments to identify the patients’ needs from their initial treatment until later after they have returned home so that they could receive sustainable treatment or medication until they are cured.17
The discharge planning can be well integrated by forming a dedicated team that manages all of the patient's treatment plans for both hospitalized or repatriated patients with planning that are made from the very moment the patient is set up for a further treatment, so that the patients and their families could experience satisfaction from the discharge planning service which is provided while they are receiving treatment. Kotler explains that patient satisfaction is patients’ level of feeling after comparing the performance (or outcome) that they felt compared to their expectations.17
Gerson stated that patient satisfaction is a situation where patients perceive that their expectations have been met or exceeded.17 Further, the factor that delays the implementation of the discharge planning is the lack of discipline of some doctors in completing all required documents for the repatriation. A team of health workers should be assigned to have it completed before the patient is discharged.
From the results, the understanding on discharge planning is still more dominantly controlled by the head of the inpatient unit than the head nurses or nurse practitioners, so it is necessary to foster communication and training to nurses who do not understand the implementation of discharge planning very well.
The conclusion of this research is that discharge planning for patients with hypertension complications is necessary to ensure efficiency in carrying out treatment and medication. As a consequence, it will surely make the patient and their family more satisfied. The discharge planning model for patients with hypertension complications is necessary considering the contributing factors of discovered in this study. Furthermore, it is necessary to explore the mechanism and needs substances in comprehensive models and modules development.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2017 funded by DRPM Universitas Indonesia No. 365/UN2.R3.1/HKP.05.00/2017.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.