To summarize the implementation of patient safety culture in nursing practice at the hospitals.
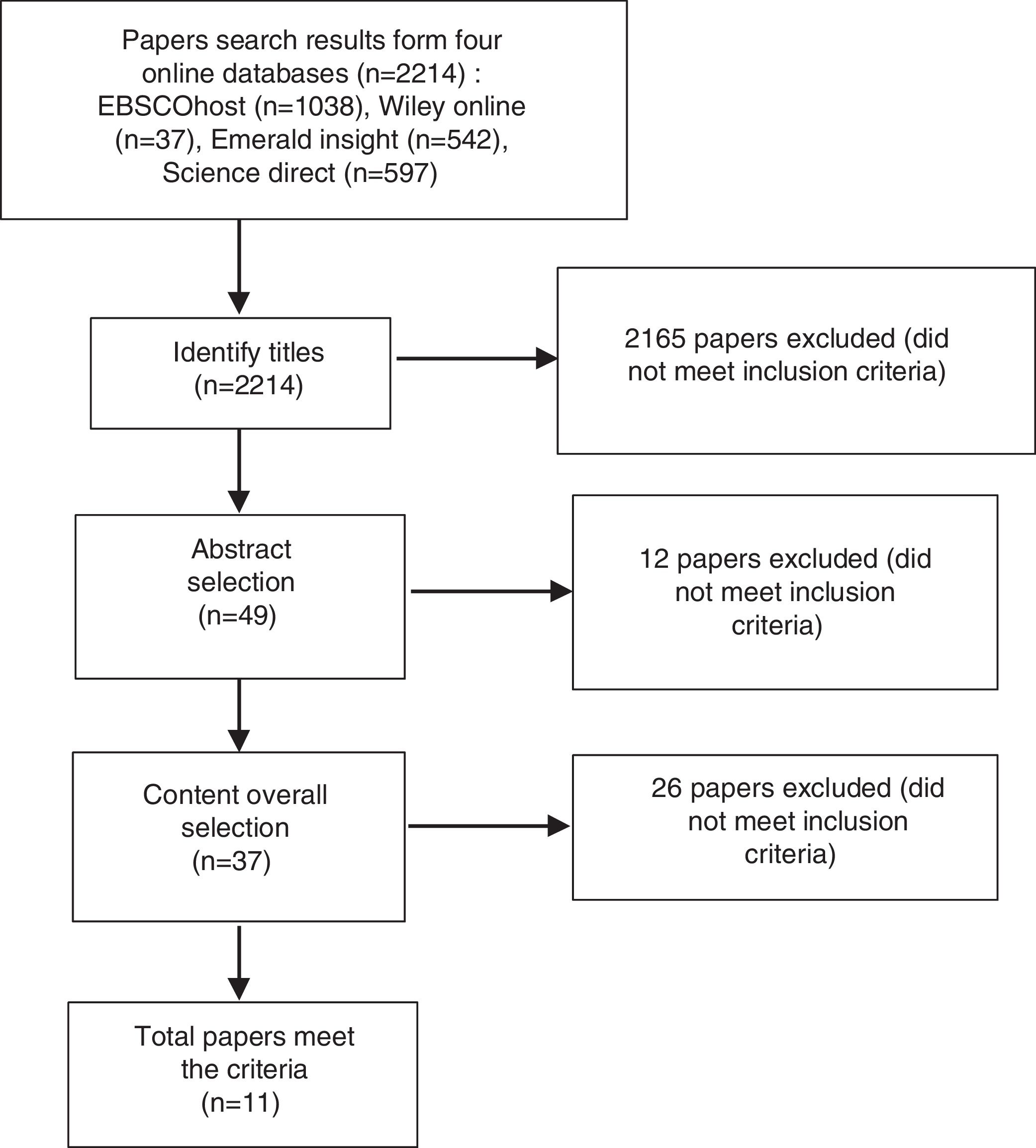
MethodWe did a literature review of the peer-reviewed articles published between 2009 until 2018 from four online databases: Emerald Insight, EBSCO, ScienceDirect, and Wiley Online, using the keywords “patient safety culture”, “nurse,” and “hospital.” For the selection of articles, we used the PRISMA Groove Model with a three-step procedure (i.e. reviewing the titles, abstracts, and full contents of the articles). Selected articles were analyzed based on the 12 dimensions of patient safety culture as proposed by Agency for Healthcare Research and Quality (AHRQ).
Results11 articles were included in the final review. We categorized the results into three categories: strengths, weaknesses, and predictors of the patient safety culture of the nursing practice. The strengths consisted of four dimensions: (1) teamwork within units, (2) organizational learning and continuous improvement, (3) the support of the hospital management to the safety of patient, and (4) frequency of events reported. On the other side, weaknesses included: (1) assumptions about the safety of the patient as a whole, (2) handover and transfer, (3) open communication, (4) staffing, (5) nonpunitive response to errors, and (6) teamwork across hospital units. Lastly, the predictors of the patient safety culture were: (1) feedback and communication about errors and (2) supervisor/manager hopes and actions that promote safety.
ConclusionOur findings can inform the hospital management to enhance the patient safety culture among nurses. It can also inform the strategy to manage the potential threats and opportunity of the patient safety implementation at the hospital.
Hospitals must provide quality service by creating a safe, effective, and well-managed hospital organization.1 One of the key activities is the evaluation of the patient safety culture in nursing practice at the hospitals.2 The World Health Organization (WHO) has listed “safety culture” as one of ten topics related to human factors that are relevant to patient safety.2,3 In 2005, the European Union (EU) also developed a system to discuss and promote patient safety as the primary thing on health care service.4
The patient safety culture affects many health workers, including their performance.5 Suroso et al. (2015) added its importance to meet the satisfaction of the people using the health care service. The patient safety culture is defined as a pattern of behavior between human and a unified organization, based on the beliefs and values, in continuously reducing the negative effects of the nursing care on the patients.6 Indeed, patient safety culture is a complex and abstract concept, yet it is of important determinant of the health care organization.2,7
The patient safety culture aims to reduce medical errors. The Institute of Medicine (IOM) seminal report “To Err Is Human: Building a Safer Health System” mentioned that each year approximately 44,000 to 98,000 people in the United States hospitals died due to medical errors, a higher number compared with the mortality caused by accident, breast cancer, and AIDS.8 However, medical errors are preventable, and preventing them can improve all aspects of patient safety.3,5,9,10
To improve patient safety, previous studies recommended a promising area of improvement in the patient safety culture.11,12 Many surveys have been conducted to measure the level of attention of the health care workers and hospital compliance relative to the application of patient safety.13 According to Agency for Healthcare Research and Quality (AHRQ), the Hospital Survey on Patient Safety Culture (HSOPSC), there are 12 dimensions of patient safety culture11,13:
- 1.
Supervisor/manager hopes and actions that promote the safety
- 2.
Organizational learning and continuous improvement
- 3.
Teamwork within units
- 4.
Communication openness
- 5.
Feedback and communication about errors
- 6.
Nonpunitive response to errors
- 7.
Staffing
- 8.
The support of the hospital management to the safety of the patient
- 9.
Teamwork across hospital units
- 10.
Hospital handoffs and transitions
- 11.
Overall perceptions of security
- 12.
The frequency of events reported
In addition, Ms et al. suggested that open communication among healthcare workers is a factor that can potentially improve patient safety. Conversely, problems related to communication can threaten patient safety.14 According to Ammouri, Tailakh, Muliira, Geethakrishnan, and Al Kindi and Abdi, Delgoshaei, Ravaghi, Abbasi, and Heyrani, a very good cooperation in the hospital is the key that supports the formation of patient safety.10,15
Some health care institutions have a lot of things to improve the culture of patient safety that do not particularly address the human behavior but the formal management system.16 Whereas, understanding the human and culture of the patient safety should be the priority.17
With this background in mind, the objective of this review was to summarize and analyze the implementation of patient safety culture in nursing practice at the hospitals from the extant literature.
MethodSearch strategyThe systematic review was started by retrieving articles published between 2009 and 2018 from four online databases: Emerald Insight, EBSCO, ScienceDirect, and Wiley Online (Table 1), using the keywords “patient safety culture,” “nurse,” and “hospital.” The initial search hit 2214 articles. The articles were then evaluated using the PICOS framework: P=participants, I=phenomenon of interest, Co=context, S=type of study (Table 2).17-20
Search strategy.
| Databases | Keywords | N |
|---|---|---|
| EBSCO | (patient) AND (safety) AND (culture) AND (nurse) AND (hospital) | 1038 |
| Wiley Online | (patient) AND (safety) AND (culture) AND (nurse) AND (hospital) | 37 |
| Emerald Insight | (patient safety culture) AND (nurse) AND (hospital) | 542 |
| Science Direct | (patient) AND (safety) AND (culture) AND (nurse) AND (hospital) | 597 |
| Total | 2214 | |
Inclusion and exclusion criteria.
| Frame | Inclusion criteria | Exclusion criteria |
|---|---|---|
| P | Nurses who work at hospital | Nurses work at the non-hospital settings |
| I | The implementation of the patient safety culture in hospitals between 2009 to 2018 | The implementation of the patient safety culture in hospitals outside the period of 2009 to 2018 |
| Co | Nursing | Non-nursing |
| S | Peer-reviewed research articles published in the journals, quantitative and qualitative studies, and open-access | Non-research articles |
Articles were selected using an adaptation of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) groove model.21 The selection process was carried out in three steps. In the early stages of the search of four online databases, 2214 articles were retrieved, followed by the first step of selection, which consisted of identifying titles that matched the keywords and the discussion topic. This step reduced the total number of articles to 49. The second step was selected based on the relevance of the abstracts (n=37). The final step involved selecting articles based on their overall content and the inclusion criteria.21 which resulted in a total number of 11 articles for analysis (Fig. 1). Articles were ranked using the Scimago Journal and Country Rank (SJR). The analysis related to the culture of patient safety as demonstrated by nurses in hospitals was conducted on these 11 articles.22
ResultsStudy descriptionThe results of the eleven articles have been analyzed. Two studies were conducted in China.23,24 The remaining studies were conducted in Saudi Arabia,25 South Korea,14 Turkey,26 Oman,10 Iran,15 Finland,27 the Netherlands,5 Taiwan,12 and Jordan.2 The articles were then numbered to facilitate the review process (Table 3).
Papers sort numbers.
| No | The authors names | SJR (Q1–Q4) | Summary |
|---|---|---|---|
| 1 | Alquwed et al. (2018) | Q1 | Strengths, weaknesses, and predictors of patient safety culture must be considered of policymakers, head of the hospital, and nurse manager in performing actions to improve patient safety culture in the hospital. |
| 2 | Ms et al. (2018) | Q1 | Age, hospital class, professional background, and professional level potentially improve and reinforce patient safety culture. |
| 3 | Yu et al. (2018) | Q1 | Evaluation of handover affects the perception of a culture of patient safety in the perinatal care units. |
| 4 | Dirik and Intepeler (2017) | Q1 | The convenience of the working environment and the presence of the manager can help health institutions in improving patient safety culture. |
| 5 | Ammouri et al. (2015) | Q1 | Learning and continuous improvement, hospital management support, supervisor/manager expectations, feedback and communications about an error, teamwork, hospital handoffs, and transitions were the main predictors of patient safety culture. |
| 6 | Abdi et al. (2015) | Q1 | The nurse manager is able to assume the role of creating a culture of safety by way of encouraging staff to report errors, cultivate learning from errors and troubleshooting communication between professions. |
| 7 | Turunen et al. (2015) | Q2 | Nurse managers have a major role in creating a culture of patient safety and ensure the safe progress of patient to caring in four acute care hospitals in Finland. |
| 8 | Smits et al. (2012) | Q1 | “Willingness to report” is a very important cultural dimension of patient safety. |
| 9 | Chen, I-Chi, Ng Hui-Fuang, Li (2012) | Q3 | Patient safety behavior is influenced by the cultural safety and cultural organizations. |
| 10 | Feng et al. (2011) | Q2 | The commitment of managers to patient safety is the key to build a culture of safety and as the role model to ensuring a patient safety culture |
| 11 | Khater et al. (2015) | Q1 | Nurses should replace the traditional culture of shame or blame with non-punitive culture in Jordanian hospitals. |
The analysis was conducted based on the 12 dimensions of patient safety culture, as previously described. These dimensions were further arranged into the following three categories (Table 4).
- 1.
Strengths (n=10)
- ∘
teamwork within units (n=1)
- ∘
organizational learning and continuous improvement (n=2)
- ∘
the support of the hospital management to the safety of patient (n=4)
- ∘
frequency of events reported (n=3).
- ∘
- 2.
Weaknesses (n=16)
- ∘
assumptions about the safety of the patient as a whole (n=3)
- ∘
handover and transfer (n=3)
- ∘
open communication (n=3)
- ∘
staffing (n=2)
- ∘
nonpunitive response to errors (n=3)
- ∘
teamwork across hospital units (n=2)
- ∘
- 3.
Predictors (n=6)
- ∘
feedback and communication about errors (n=3)
- ∘
supervisor/manager hopes and actions that promote the safety (n=3)
- ∘
Categories of patient safety dimensions.
| Category | Cross-sectional | Mixed method | No. paper | Important findings |
|---|---|---|---|---|
| Strengths | ||||
| Teamwork within units | 1 | 1, 4, 5, 11 | Teamwork is a critical patient safety culture. It was moderate (59.3%) and highest score in Oman (83.4%). Teamwork is able to address the problem of a job, enable the team members to learn and grow. | |
| Organizational learning-continuous improvement | 2 | 1, 4, 5 | It is high positive responses (Second highest 81.1%) to enhance the safety of the patient and building an effective leadership in the hospitals. | |
| The support of the hospital management to the safety of patient | 3 | 1 | 4, 6, 8, 11 | It is an important role in the relationship between nurse and patient safety. It gives priority to patient safety. |
| The frequency of events reported | 3 | 7, 8, 11 | This includes the high numbers that have been done at the nurse manager. This figure is about 69.15% and 59% implementing nurse. | |
| Weakness | ||||
| Overall perceptions of safety | 3 | 1, 2, 3 | This is rated at 50% or below. This perception is influenced by confidence, openness and communication culture, language, and religion. | |
| Hospital handoff and transitions | 3 | 1, 3, 11 | Handoff dissatisfaction and ineffective procedures of nursing handoff are global problems. They are influenced by knowledge transfer among staffs, inadequate policies, fatigue, stress, excessive workload, incomplete handoff system, no handoff guideline/checklist | |
| Communication openness | 3 | 1, 3, 11 | This is rated at 37.4%–49%. This happens because nurses are afraid to ask when they are in doubt. The main cause of more than 70% occurrence of sentinel events. | |
| Staffing | 2 | 1, 11 | This is rated at 21.2%–34.53%. | |
| Nonpunitive response to the error | 3 | 1, 7, 11 | This is rated at 16.6%–21% | |
| Teamwork across hospital units | 2 | 3, 11 | This is rated at up to 41.73%. It is a critical culture that relies on collaboration, cooperation, and mutual respect. | |
| Predictors | ||||
| Feedback and communication about error | 3 | 1, 5, 11 | This is rated at 56.3%–68.7%. It is based on the report of the incident. The manager needs to proactively respond to the follow-up of reporting to improve patient safety and prevent errors. | |
| Supervisor/manager hopes and actions that promote the safety | 3 | 1, 5, 11 | This is rated at 54.3%–57.95%. Patient safety relies heavily on supervisor/manager's actions such as appropriate staffing, seriously responding to the consideration of staff, emphasizing good cooperation, and addressing the emerging patient safety issues. | |
Four dimensions were identified as strengths: teamwork within units,10,12,26,28 organizational learning and continuous improvement,10,12,26 the support of the hospital management to the safety of patient,5,15,26,28 and frequency of events reported.5,27,28 The successful practice of the application of these dimensions can shape a patient safety culture by directing the officer's behavior naturally to improve patient safety.26
WeaknessesSix dimensions were categorized as weaknesses, including assumptions about the safety of the patient as a whole,14,23,25 handover and transfer,14,25,28 open communication,14,25,28 staffing,2,25 nonpunitive response to errors,25,27,28 and teamwork across hospital units.14,28 These dimensions, in general, have proven to negatively affect patients and healthcare organizations.25
PredictorsFurthermore, wwo dimensions were identified as predictors: feedback and communication about errors and supervisor/manager hopes and actions that promote the safety.10,12,28 The perception of patient safety depends on other factors existing within a hospital that affect nursing practice, such as nurse demographics (e.g., age, gender, marital status, education, hospital type, long-running services, worksite, long service at the given moment, and longtime work per week).25
DiscussionIn this study, we analyzed patient safety culture using 12 dimensions of patient safety according to the AHRQ to evaluate the patient safety in hospitals as a whole or for specific units within a hospital. The dimensions comprised 45 items covering a range of signs for presenting respondents’ commitment to and perception of patient safety.12
Effective teamwork and improved organizational learning help hospital policy makers and nurse managers improve a culture of sustainable patient safety,25 reduce the length of hospital stay and improve the safety of clinical trials.29 In addition, effective nursing practice is also able to facilitate a safety culture thus encouraging nurses to participate in decision making26 and implementing strategies to maintain nurse leadership abilities.10 Studies show that people in the same workplace can support each other to get the work done well, safely, and timely, with an increasingly strong patient safety culture.2
Hospital management support for patient safety is related to reported events about drugs, materials/equipment, and collaboration with local doctors/consultants. In units with better reporting, there are fewer incidents of errors with equipment and more collaboration with experts.5 Thus, managers should encourage the staffs’ awareness and compliance in reporting of errors as it contributes to developing a strong safety culture.26
Hospitals should pay significant attention to the weaknesses identified by this study25 because they represent threats to patient safety.14 For instance, without a good system of handoff, the handoff errors are more likely to occur in the hospital.14 Without standardized handoff guidelines, the evaluation of handoffs by nurses is also more likely to be negative.14
Understanding the perceptions of hospital nurses on the patient safety culture is equally important for the policymakers at the hospital to strengthen the patient safety culture from the point of nursing workforce.12 Nurses with lower workload tend to better perception of patient safety, and vice versa. Therefore, policies nurse staffing is of paramount important to enhance the culture of patient safety.2
These dimensions have aspects that can either negatively or positively affect patient safety at the hospital. Lacking coordination between units in the hospital is associated with errors and unexpected events.2 Good communication and proactive response to the recommendations of staffs to improve patient safety can help avoid errors.10 At present, evaluation of patient safety culture is carried out by many international accreditation organizations.25 Above all, strengthening patients safety takes a solid commitment of the healthcare organizations.30
Our findings can inform the hospital management to enhance the patient safety culture among nurses. They can also inform the strategy to manage the potential threats and opportunity of the patient safety implementation at the hospital. The strengths identified in this review can help enhance the patient safety culture, facilitate nurses in decision-making, implement strategies pertinent to the patient safety. Meanwhile, the weaknesses listed in this study also deserve a significant portion of attention from the hospital policymakers as they can threaten the patients safety culture.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2018 funded by DRPM Universitas Indonesia No. 1853/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.