This article aims to identify and assess the utilization of interactive educational media in improving self-efficacy of pulmonary tuberculosis patients.
MethodA comprehensive search strategy by systematic literature review that searches research articles in database research journals, internet searches, and article reviews. The search database used in MEDLINE, CINAHL, Pubmed, Cochrane library, Proquest PsycINFO, and Science Direct.
ResultsThe use of interactive educational media on clients with Tuberculosis problems has been widely applied. Application of interactive educational media found that the interventions are to encourage the client to overcome the existing obstacles such as loss of client's privacy, stigma from family and society, transportation problem, and the burden of conventional therapy.
ConclusionsInnovative strategies are needed in an effort to improve self-efficacy. The number of media can be a reference for health workers in implementing a tuberculosis treatment program that will enhance client self-efficacy.
The World Health Organization has stated that pulmonary TB disease is a global humanitarian emergency, which requires a national and global commitment to pulmonary tuberculosis disease control established in the policy of SDGs 2015–2030 with the target of decreasing morbidity and mortality rate.1 According to the World Health Organization data at 2013, there are 8.6 million new cases of pulmonary tuberculosis (TB) and 410,000 deaths. The number of new cases in Indonesia in 2015 amounted to 125 per 100,000 inhabitants. Tuberculosis is an important issue for Indonesia, which has a high prevalence rate. Pulmonary tuberculosis can be handled and controlled by giving information to patients to increase their self-efficacy.2
Self-efficacy defined as an individual's belief in their ability, which is necessary for self-motivation. Lack of awareness is one cause of lack of adherence to medication protocols and negative health behaviors, such as spitting and sneezing, in pulmonary TB patients. Increasing self-efficacy could improve patients’ awareness of their health behavior. Self-efficacy plays an essential role in supporting treatment for pulmonary tuberculosis and in the prevention of transmission. Innovative strategies are needed to improve self-efficacy in this patient group.
Increasing patients’ self-efficacy used and delivered health education via a variety of methods. Studies have indicated that social media is more useful than traditional media for improving self-efficacy and disseminating health information. The results showed that an e-health video that lasted for just over ten minutes was effective in encouraging stages in the level of changes to the preparation stage of breast self-examination and self-efficacy of breast self-examination.3 An intervention involving a series of videos is a cost-effective method of delivering nutrition education to low-income families.4 Interactive educational media is an effective way of delivering health promotion to the community. Interactive educational media involves the patient actively, which increases the self-efficacy of pulmonary tuberculosis patients. Many forms of educational media have studied, so there is a need for a detailed review. The results of this systematic review will help nurses, health workers, governments, and non-governmental organizations to provide and develop health education using interactive educational media.
This review aimed to identify and assess the use of interactive educational media to improve the self-efficacy of pulmonary tuberculosis patients. Interactive educational media applied in various studies related to health promotion. The results of this review could help nurses, health workers, governments and non-governmental organizations to select effective interactive educational media for pulmonary TB patients.
MethodsDesignA literature review conducted on the research question, “Which interactive educational media is the most effective in improving the self-efficacy of pulmonary tuberculosis patients?”
Eligibility criteriaSelection criteria were chosen based on the research question. To be included, studies needed to be written in English and published between 2000 and 2017. Only studies for which the full text was available included. Studies had to investigate the use of interactive educational media for improving the self-efficacy of pulmonary tuberculosis patients.
SourcesThe article developed a comprehensive search strategy, whereby research articles accessed via databases, research journals, internet searches, and article reviews. The databases used were MEDLINE, CINAHL, PubMed, the Cochrane Library, ProQuest, PsycINFO, and Science Direct.
SearchKeywords used in the search were tuberculosis, self-efficacy, health education, visual education, video, mobile application, social media, computer network, and interactive technology. Searching article combined with the Boolean operators AND and OR. Same search criteria used from a database journal.
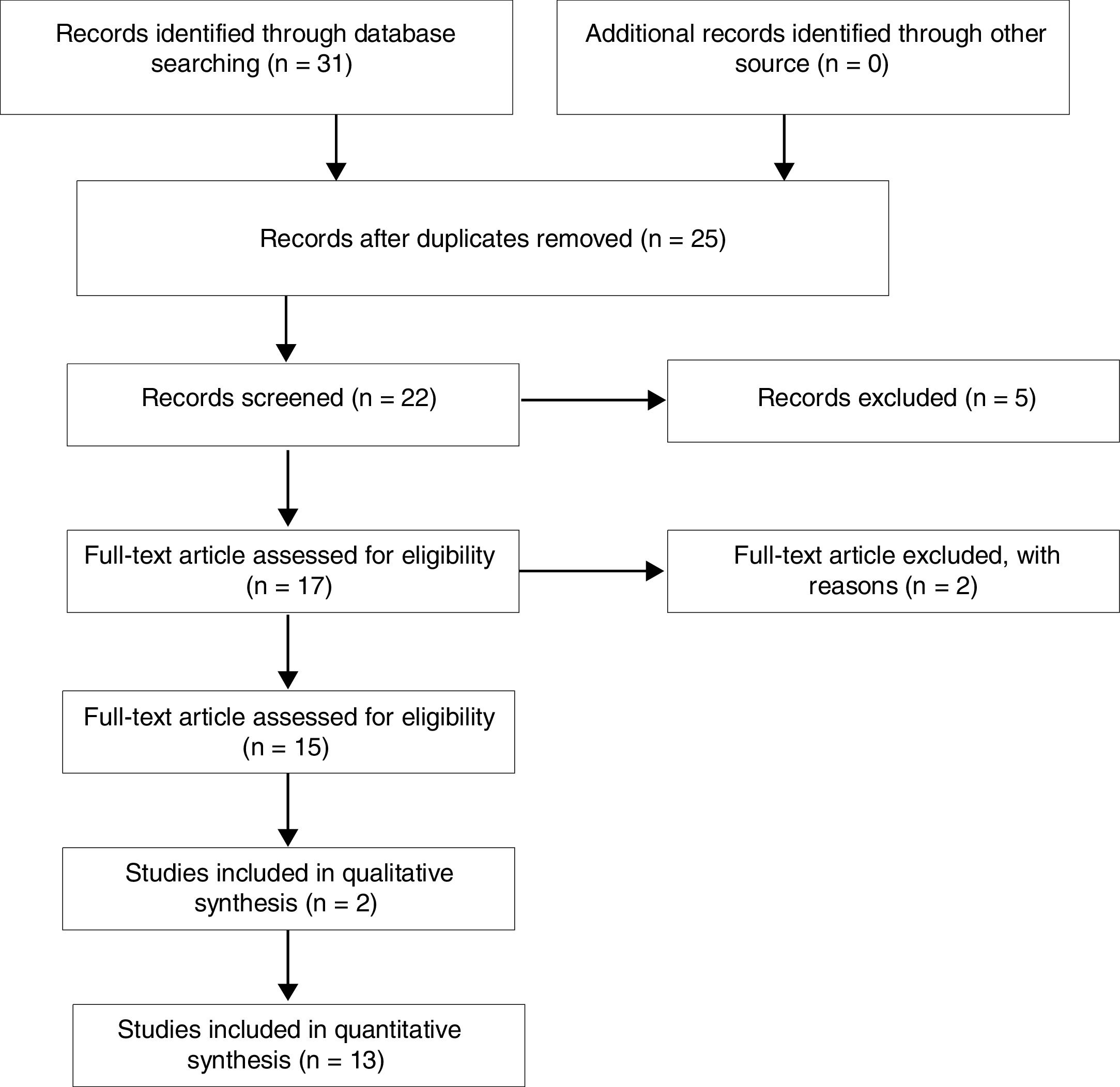
Study selection and data analysesBased on an analysis of English research literature from a total of 31 searches, the review included 15 studies that identified and assessed the use of interactive educational media for improving the self-efficacy of pulmonary tuberculosis patients. The selection process for the studies shown in Fig. 1, and this used by PRISMA recommendations.
ResultsClinicians may attempt to change the health behavior of individuals and communities by delivering health education via various educational media. One such media is video. Video interventions are effective in promoting sunscreen adherence, female condom use, HIV testing, prostate cancer screening, breast self-examination, medication adherence, and self-care in heart failure patients.5 Video-based social media channels via YouTube have also been used to educate people about chronic obstructive pulmonary disease. Videos uploaded to YouTube channels with video role model content are capable of enhancing self-efficacy training.6,7 Video media has also been applied to educate cervical cancer patients with hearing loss.8 Result research shows that the use of video in health education has widely applied.
Health education videos have also used for patients with tuberculosis. Video instructions on sputum are closely linked to the increased visit of microscopic TB detection.9 Use of video-based devices and mobile phones at home was more effective on self-efficacy and adherence when compared with home visits by officers and significantly decreased the number of neglected observations of patients with tuberculosis.10 Health workers in Salvador showed a video to tuberculosis patients to help them understand their disease, and this significantly increased patients’ knowledge about the success rates of TB treatment and transmission. This increased time efficiency, the number of patients undergoing treatment, the amount of sputum sent to the clinic, and the number of investigations of suspected TB. Involving the families of TB patients in the video intervention led to a decrease in negative stigma within the family. Family fears diminished, and motivation increased in family members undergoing treatment.11
The growing use of mobile devices in the community has implications for their use in health education, especially in patients with tuberculosis. Research has used mobile phone applications. Health workers used the mHealth application for the Multi-Drug Resistance TB Program in remote areas of southern Africa for seven months, which increased the number of patients undergoing treatment. Also, communication among health workers increased with the use of the application.12 In southern India, the TB DOTS treatment utilizes the patient's mobile phone for calling in the consultation process between the patient with TB and the TB treatment supervisor. The result shows that the use of mobile phones for consultations with patients can be useful for promoting patient compliance. Patients assume that mobile phones are a valuable medium of communication for them even though they prefer face-to-face interaction with healthcare workers.13 A similar use of mobile phones has been implemented in Peru, where messages sent by short message service (SMS) were used to improve TB treatment compliance.14 In the United States, SMS has been coupled with telephone services to remind patients of their medication schedule.15
As for systematic review research results related to the use of mobile phones in TB treatment, interventions have been designed to encourage the patient to overcome obstacles such as loss of privacy, transportation problems, and stigma within their family and society. The burden of conventional therapy. The patient's perceived implications of attention and a sense of responsibility for treatment embedded in them.16 The results of this systematic review indicate that SMS-based interventions used to treat TB are ineffective because the poor quality of content has failed to improve patient compliance in tuberculosis treatment.17
Another form of interactive patient intervention is the use of integrated smartphones with web-based, or Mobile Interactive Supervised Therapy (MIST) systems. This type of intervention is provided by sending reminders about medication regularly, and they require patients to record and upload a video every time they take a drug, which is then reviewed by a health worker.18 Interactive patient intervention demonstrates that some innovative interventions promoting adherence in patients with TB enhance the patient's self-efficacy.
DiscussionVarious forms of intervention have applied by researchers using creative innovations applied to multiple types of educational media. The articles reviewed in this study showed that educational media used in the treatment of tuberculosis patients included video, video calls, telephone service, short message service (SMS), and applications on smartphones.
This study found that some videos provided to patients have poor qualities, and educational video interventions uploaded on YouTube channels were found to be qualified and disreputable. Sorting and selecting videos that contain useful information requires a good understanding of TB and its treatment. This type of intervention was not sufficient in measuring self-efficacy and changes in patient behavior. The advantages of video interventions are cheaper regarding cost compared with other interventions.
Mobile phone interventions have barriers to some service users. The majority of TB patients have low socioeconomic status, which means that they may need additional training from health workers to use mobile phone features, such as alarms, calling, video calls, and SMS. Also, this medium requires incentives offered to patients. The advantage of this medium is the effectiveness of monitoring, especially of patients who have started DOTS. Monitoring helps the patient to participate in TB treatment until it completed. The use of mobile phones means that clinicians can offer a high-intensity service, which makes the patient feel paid attention, which is likely to have an impact on the emergence of self-efficacy.
ConclusionIndonesia is a country with a high prevalence of pulmonary TB, so it is important to find ways to handle and control this disease. One way to do this is to provide information to pulmonary TB patients to increase their self-efficacy. Poor adherence to medication and negative health behaviors, such as spitting and sneezing, has been found to be due to a lack of individual awareness. Increasing self-efficacy could increase patients’ awareness and in turn, improve their health behavior. Innovative strategies are needed to improve self-efficacy, such as the delivery of health education via interactive educational media. Types of educational media available to TB patients include video, video calls, telephone, service short message service (SMS), and applications on smartphones. A number of these media can be used by health workers to deliver tuberculosis treatment programs that increase patients’ self-efficacy.
Limitations of the studyOnly articles written in the English language included in the study, so there were no articles from Indonesia. Also, only those articles whose full texts were available in electronic bibliographic databases reviewed.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2017 funded by DRPM Universitas Indonesia No. 369/UN2.R3.1/HKP.05.00/2017.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.