To evaluate the degree of satisfaction of women treated with dermopigmentation and reconstruction of the Areola-Nipple Complex (ANC) after breast reconstruction, as well as their demographic profile and clinical-evolutionary characteristics.
MethodsDescriptive observational study including 128 women treated with dermopigmentation after oncologic breast reconstruction during 2018. In 2021 they were administered an adapted satisfaction questionnaire, which contains 27 items and categorizes satisfaction from 1–5, in addition other clinical-evolutionary and demographic variables were collected.
ResultsMean age was 51 (±9) years, 89.1% had previously undergone PDA reconstruction. Mean satisfaction with dermopigmentation was 4.4 (±0.88) and 3.79 (±1.06) for PDA reconstruction. Complications were rare, but 54.5% (n = 54) of the patients reported that the CAP reconstruction did not offer the expected projection, 91.6% (n = 98) that the color had faded and 51.4% (n = 55) would choose permanent tattooing. It was perceived that, the higher the satisfaction of the CAP, the higher the satisfaction of dermopigmentation, while the older the age and previous chemotherapy treatment the lower the color durability (p value ≤ 0.05).
ConclusionsPatients who underwent reconstructive breast surgery show a high degree of satisfaction with dermopigmentation and surgical reconstruction of the PDA, but reiterate the low projecticity of the dermopigmentation and the surgical reconstruction of the PDA, but reiterate the low degree of satisfaction with the dermopigmentation.
Evaluar el grado de satisfacción de las mujeres tratadas con dermopigmentación y reconstrucción del Complejo Areola-Pezón (CAP) tras una reconstrucción mamaria, así como su perfil demográfico y sus características clínico-evolutivas.
MétodoEstudio observacional descriptivo donde se incluyeron 128 mujeres tratadas con dermopigmentación tas una reconstrucción mamaria oncológica durante el año 2018. En 2021 se les administró un cuestionario de satisfacción adaptado, que contiene 27 ítems y categoriza la satisfacción del 1-5, además se recogieron otras variables clínico-evolutivas y demográficas.
ResultadosLa media de edad fue de 51 (± 9) años, a un 89,1% se les realizó la reconstrucción del CAP previamente. La satisfacción media de la dermopigmentación fue de 4,4 (± 0,88) y de 3,79 (± 1,06) para la reconstrucción del CAP. Las complicaciones fueron escasas, pero el 54,5 %(n = 54) de las pacientes refieren que la reconstrucción del CAP no ofrece la proyección esperada, el 91,6% (n = 98) que el color ha desvanecido y el 51,4% (n = 55) elegirían el tatuaje permanente. Se percibió que, a mayor satisfacción del CAP, mayor satisfacción de la dermopigmentación, mientras que a mayor edad y tratamiento con quimioterapia previa menor durabilidad de color (pValor ≤ 0,05).
ConclusionesLas pacientes intervenidas por cirugía reconstructiva de mama muestran un alto grado de satisfacción de la dermopigmentación y de la reconstrucción quirúrgica del CAP, pero reiteran la escasa proyección del CAP, la falta de permanencia de color y la voluntad de obtener resultados más duraderos. Los resultados preliminares invitan a seguir investigando en la posible relación causal entre variables.
Dermopigmentation as an alternative and/or complement to surgical reconstruction of the nipple-areola complex is widely used and accepted, but few studies have evaluated patient satisfaction and future lines of improvement.
What does it contribute?This is the first specific study conducted in the country, and indicates that satisfaction with dermopigmentation is high, complications are low, and that new lines of future research in dermopigmentation and permanent tattooing are being opened.
In 2022, the estimated incidence of breast cancer in Spain was 33375 new cases.1 The initial therapeutic approach includes chemotherapy, radiotherapy, and/or oncological surgery as the treatments of choice. In relation to surgery, there are several options ranging from conservative surgery to reconstructive surgery, ending with reconstruction of the nipple-areola complex (NAC) to create a natural appearance of the whole breast.2
Procedures for reconstruction of the nipple-areola complex vary according to the therapeutic circuits and the surgeon’s choice. There are different techniques for the creation of the neo-nipple such as grafting, local flaps, or new nipple prostheses. The local flap is one of the most commonly used techniques and consists of creating a nipple using the patient’s own skin. It is performed when sufficient skin and tissue is available and is performed under local anaesthesia. The most notable limitation of this surgery is loss of volume and projection.2
In our country, in some plastic surgery services, in order to enhance the benefits of reconstruction surgery of the NAC, dermopigmentation (also known as micropigmentation) is offered as part of the public service portfolio.2,3 This is a non-surgical technique performed by nurses, is practically painless, and consists of introducing a series of pigments under the epidermis using a dermograph that uses micropuncture at a depth of 2–3 mm of skin.3 The objective is to mimic the natural appearance of the breast. Sometimes, when it is anticipated that the projection of the neo-nipple will not be optimal, direct 3D dermopigmentation is chosen, which mimics projection through the optical effect of colours and shadows.2,3 It is generally performed in two sessions 4–8 weeks apart, although more sessions may be necessary depending on the skin’s absorption of the pigment and at the health professional’s discretion.3,4 Post-treatment care is based on hygiene and prevention of infection. The treatment is semi-permanent and lasts 2 to 5 years on average.3–5 These aspects are different from permanent tattooing, which is primarily based on inks that offer longer lasting results.6 The pigment may take 10 years or more to disappear totally, the little data available indicate that durability is linked to the shade and intensity used, and the specific skin response.3–6
In the field of areolar reconstruction, the same contraindication criteria apply as for decorative tattoos, and chemotherapy and/or radiotherapy in under six months, unstable scars, skin disorders, local or systemic bacterial, fungal, or viral infections are included as provisional contraindications.4–7
No clear prevalence data are available with regard to generic complications of tattooing or dermopigmentation; when they occur, these complications are usually hypersensitivity/allergy and/or infection.7 In the specific area of areolar reconstruction, the few published studies indicate that complications are infrequent, but the risk of infection, local bleeding, and/or allergic reaction must still be considered.5,8–10 There are no data on causal relationships between complications and risk factors such as type of reconstruction, previous treatment, or previous history.10
In recent years, numerous studies have been conducted on surgical reconstruction techniques for the NAC (including tattooing) and their relationship with self-image,3,11,12 which confirm that the creation of a new NAC can help improve self-image.5,10 Although not yet validated, questionnaires have been designed for dermopigmentation, to assess satisfaction, durability, and adverse effects.4,5,9 The published data arise from descriptive analyses, which show reliable and satisfactory results from the perspective of patients and professionals, but these questionnaires are brief and there is a lack of analytical data that evaluate the relationship between variables and the specificity of the products used.
It is for this reason that the present study aims to evaluate the degree of satisfaction of women treated with areolar dermopigmentation and reconstruction of the NAC in the public tertiary hospital Hospital Universitari de Bellvitge (HUB), to describe their demographic profile and thus determine their clinical and evolutionary characteristics.
MethodCross-sectional descriptive observational study, in which the study population was women who underwent the dermopigmentation procedure after reconstructive breast surgery in 2018 at the HUB outpatient clinic. The study consisted of determining the degree of satisfaction of women treated with dermopigmentation and reconstruction of the NAC two years after oncological reconstructive breast surgery, describing the profile of the women who come for this procedure, and determining their demographic, clinical, and progression characteristics.
The inclusion criteria for the study were those women undergoing breast reconstructive surgery at the HUB who required dermopigmentation and underwent the treatment in 2018. Women who did not provide informed consent (IC), who underwent pigmentation outside this period, who had postoperative contraindications and, therefore, could no longer be pigmented, or who had died since the intervention were excluded.
In 2018, 170 patients were treated under the dermopigmentation programme, a sample of 128 women was selected, a value sufficient to estimate with a confidence of 95% and a precision of +/- 5 percentage units, a population percentage that is expected to be around 50% with a percentage of necessary replacements of 20%.
A non-probabilistic consecutive method was used to select the sample.
The main variable under study was the degree of satisfaction; an ordinal qualitative variable that was measured in parallel for the variables of surgical reconstruction of the NAC and dermopigmentation using a Likert-type scale from 1 to 5: 5 (excellent result), 4 (good result), 3 (satisfactory result), 2 (disappointing result), 1 (poor result).
This variable was collected using a questionnaire developed by Martin and Cutress,5 translated and adapted by our research team (February 2021), including new variables of interest: pathological history, previous treatment, timing of complications, and treatment preference.
In April 2021, a pilot test of the original questionnaire consisting of 27 questions was undertaken, administering it to two nurses who specialise in pigmentation, three plastic surgeons from the Functional Breast Unit, and a non-randomly selected patient for validation of understanding of the content, assessed by means of a structured survey. The suggested modifications were then made, and the final questionnaire consists of 27 questions (to be completed by the patient) divided into two sections: clinical data and satisfaction data.
The secondary variables to be studied were: age, pathological history, allergies, date of reconstruction surgery, type of oncological surgery performed, previous oncological treatment, previous nipple reconstruction, laterality of the reconstructed nipple, assessment of nipple position, assessment of nipple size, complications of NAC reconstruction, laterality of dermopigmentation, timing of dermopigmentation, method of anaesthesia, assessment of areolar size, assessment of areolar staining, complications of dermopigmentation, durability of colour, repetitions of the technique, willingness to repeat, and preferences of treatment technique (dermopigmentation/permanent tattooing).
The questionnaire was administered by the research team in the second half of 2021, two years after the intervention. The patients were contacted by telephone, the study was explained and, after signing the IC form, they were offered the option of completing the questionnaire in person or by telephone. For the telephone responses, the research team recorded the answers manually on an individual questionnaire (paper) and then transferred them to the study database. For the responses recorded in person (paper), the transfer of data directly into the database was organised. The IC form (verbal/paper) was attached to the medical record.
The data obtained were analysed using Minitab V19 statistical software and a descriptive analysis using mean, standard deviation, and minimum and maximum values for variables following a normal and median distribution, 25th and 75th percentile, and minimum and maximum values for those variables that did not follow a normal distribution. In addition, χ2 and Kruskal-Wallis tests were used to analyse the relationship between the categorical variables; satisfaction with the NAC, dermopigmentation satisfaction, NAC complications, dermopigmentation complications, timing of colour disappearance, anaesthesia, and treatment preference with the rest of the variables.
The present study has the approval of the institution’s ethics committee (PR196/21). All respondents agreed to participate by signing of IC via telephone, and the data collected for the study were identified by a numerical code to guarantee pseudonymised treatment in accordance with current legislation. This project was conducted in accordance with the ethical standards of the Declaration of Helsinki and good research practice.
ResultsOne hundred and twenty-eight patients were asked to participate in the study, 110 responded to the questionnaire, 9.4% did not answer the telephone calls, and 4.7% had died since the intervention. All patients included chose the telephone participation option. All respondents were women, the mean age was 51 (±9 standard deviation [SD]) years, in terms of clinical characteristics it was observed that most had no comorbidities or allergies, 69.4% (n = 75) had undergone complementary treatments with chemotherapy, and 61.1% (n = 66) had undergone radiotherapy (Table 1).
Clinical characteristics of the patients.
| N = 128 | (%) | |
|---|---|---|
| 1. Comorbidities | ||
| No | 78 | (72.2) |
| Cardiovascular | 10 | (9.3) |
| Skin disease | 3 | (2.8) |
| Other | 17 | (15.7) |
| 2. Allergies | ||
| No | 87 | (80.6) |
| Drug | 18 | (16.7) |
| Metal | 1 | (.9) |
| Other | 2 | (1.9) |
| 3. Previous breast reconstruction | ||
| Yes | 103 | (98.1) |
| No | 2 | (1.9) |
| 4. Type of reconstructive breast surgery | ||
| Fixed volume implant | 18 | (16.7) |
| Dorsalis muscle and fixed-volume implant | 7 | (6.5) |
| Broad latissimus dorsi muscle | 6 | (5.6) |
| DIEP | 57 | (52.8) |
| PAP | 2 | (1.9) |
| Other | 18 | (16.7) |
| 5. Neo/adjuvant radiotherapy | ||
| Yes | 66 | (61.1) |
| No | 42 | (38.9) |
| 6. Neo/adjuvant chemotherapy | ||
| Yes | 75 | (69.4) |
| No | 33 | (30.6) |
DIEP: Deep inferior epigastric perforator flap; PAP: Profunda artery perforator flap.
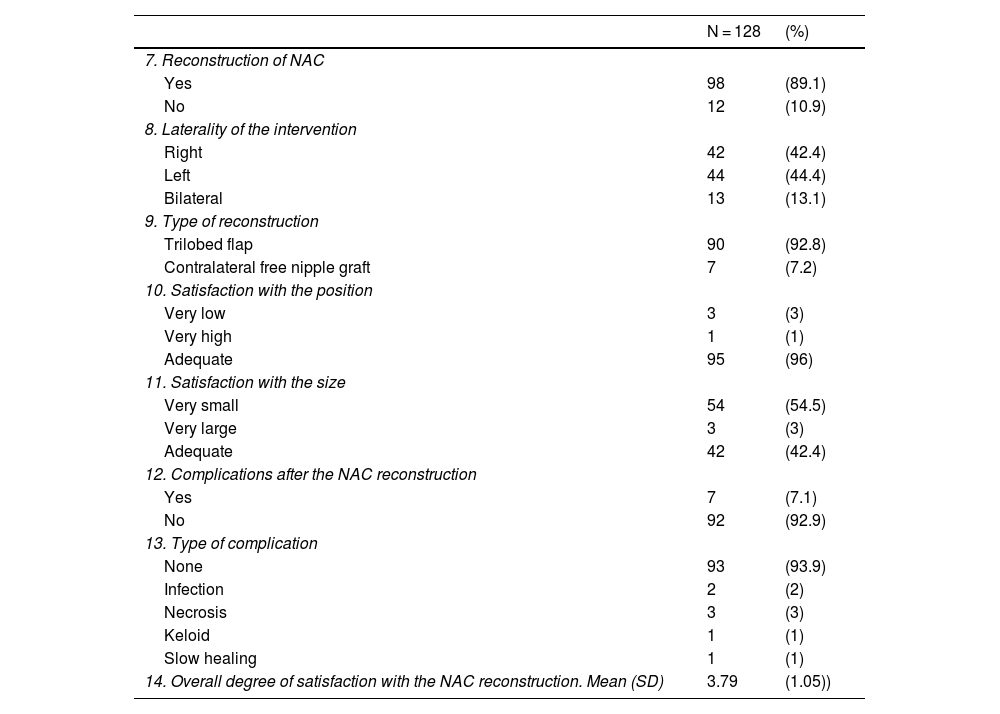
Using a scale of 1 to 5, the mean satisfaction with regard to reconstruction of the NAC was 3.79 (±1.06). Surgical nipple reconstruction was performed in 89% (n = 98) of the women treated, 93% (n = 90) of the cases with trilobed flap. In relation to the position of the nipple, 96% (n = 95) considered it adequate; for 54.5% (n = 54) of the patients the new nipple was too small (Table 2).
Satisfaction with the surgical reconstruction of the nipple-areola complex.
| N = 128 | (%) | |
|---|---|---|
| 7. Reconstruction of NAC | ||
| Yes | 98 | (89.1) |
| No | 12 | (10.9) |
| 8. Laterality of the intervention | ||
| Right | 42 | (42.4) |
| Left | 44 | (44.4) |
| Bilateral | 13 | (13.1) |
| 9. Type of reconstruction | ||
| Trilobed flap | 90 | (92.8) |
| Contralateral free nipple graft | 7 | (7.2) |
| 10. Satisfaction with the position | ||
| Very low | 3 | (3) |
| Very high | 1 | (1) |
| Adequate | 95 | (96) |
| 11. Satisfaction with the size | ||
| Very small | 54 | (54.5) |
| Very large | 3 | (3) |
| Adequate | 42 | (42.4) |
| 12. Complications after the NAC reconstruction | ||
| Yes | 7 | (7.1) |
| No | 92 | (92.9) |
| 13. Type of complication | ||
| None | 93 | (93.9) |
| Infection | 2 | (2) |
| Necrosis | 3 | (3) |
| Keloid | 1 | (1) |
| Slow healing | 1 | (1) |
| 14. Overall degree of satisfaction with the NAC reconstruction. Mean (SD) | 3.79 | (1.05)) |
NAC: Nipple-areola complex; SD: Standard Deviation.
In 98% (n = 108) of the patients in the sample, areolar dermopigmentation was performed after reconstruction of the NAC.
For 97.2% (n = 104) of the patients the size of the areola was correct and for 75.7% (n = 81) the tone was adequate. Ninety-one per cent (n = 98) indicated that the colour had faded over time. Mean satisfaction with the result of the dermopigmentation was 4.4 (±.88). Finally, if given the choice between dermopigmentation or permanent tattooing, 51.4% (n = 55) of them would choose permanent tattooing, 29.9% (n = 32) would be advised by the health professional, and 14% (n = 15) would undergo dermopigmentation again (Table 3).
Satisfaction with the dermopigmentation of the nipple-areola complex.
| N = 128 | (%) | |
|---|---|---|
| 15. Laterality treated | ||
| Right | 44 | (40.7) |
| Left | 47 | (43.5) |
| Bilateral | 17 | (15.7) |
| 16. Time performed | ||
| Before NAC reconstruction | 2 | (2) |
| After NAC reconstruction | 98 | (98) |
| 17. Analgesia beforehand | ||
| No | 6 | (5.6) |
| Topical analgesia (cream) | 101 | (94.4) |
| 18. Satisfaction with areolar size | ||
| Very small | 2 | (1.9) |
| Very large | 1 | (.9) |
| Adequate | 104 | (97.2) |
| 19. Satisfaction with colour | ||
| Very clear | 21 | (19.6) |
| Very dark | 5 | (4.7) |
| Adequate | 81 | (75.7) |
| 20. Complications of dermopigmentation | ||
| Yes | 10 | (9.3) |
| No | 98 | (90.7) |
| 21. Type of complication | ||
| None | 98 | (90.7) |
| Infection | 1 | (.9%) |
| Skin reaction | 1 | (.9%) |
| Pain | 8 | (7.4%) |
| 22. Disappearance of colour later | ||
| Yes | 98 | (91.6) |
| No | 9 | (8.4) |
| 23. Timing of disappearance of colour | ||
| After one year | 18 | (16.8) |
| After two years | 41 | (38.3) |
| After three years | 17 | (15.9) |
| After four years | 3 | (2.8) |
| DK/NA | 28 | (26.6) |
| 24.Repetition of treatment | ||
| No | 101 | (94.4) |
| Yes | 6 | (5.6) |
| 25.Willingness to repeat | ||
| Yes | 99 | (92.5) |
| No | 8 | (7.5) |
| 26.Treatment preference | ||
| Permanent (tattoo) | 55 | (51.4) |
| Semi-permanent (dermopigmentation) | 15 | (14) |
| At the discretion of the health professional | 32 | (29.9) |
| DK/NA | 5 | (4.7) |
| 27.Overall degree of satisfaction with dermopigmentation. Mean (SD) | 4,27 | (.88) |
NAC: Nipple-areola complex; SD: Standard Deviation.
Table 4 shows the association between satisfaction with the NAC and dermopigmentation with other variables, detecting statistically significant differences. It was observed that patients with larger NAC size showed greater satisfaction (p = .001), also those who had reconstruction of the NAC (p = .039). In addition, patients with higher satisfaction with the NAC showed higher satisfaction with the dermopigmentation (p = .002) (Table 4). However, older patients reported that the colour disappeared sooner (p = .047) and a longer duration of colour in time was observed in patients who had not previously undergone chemotherapy (p = .045). Patients who reported a larger areolar size had a higher degree of satisfaction with dermopigmentation (p = .033), whereas those who reported not wanting to repeat the treatment had a lower degree of satisfaction (p = .024).
Analysis between variables – Kruskal-Wallis test.
| Variable | Variable | p-Value |
|---|---|---|
| Radiotherapy | Size of NAC | .131 |
| Chemotherapy | Size of NAC | .632 |
| Satisfaction with NAC | Size of NAC | .001 |
| Satisfaction with NAC | Age | .243 |
| Satisfaction with NAC | Reconstruction of NAC | .039 |
| Satisfaction with NAC | Areolar position | .530 |
| Satisfaction with dermopigmentation | Age | .423 |
| Satisfaction with dermopigmentation | Satisfaction with NAC | .002 |
| Satisfaction with dermopigmentation | Reconstruction of NAC | .619 |
| Satisfaction with dermopigmentation | Type of surgery | .307 |
| Satisfaction with dermopigmentation | Areolar size | .033 |
| Satisfaction with dermopigmentation | Willingness to repeat | .024 |
| Duration over time of colour | Age | .047 |
| Duration over time of colour | Radiotherapy | .168 |
| Duration over time of colour | Chemotherapy | .045 |
| Complications of dermopigmentation | Age | .918 |
| Complications of dermopigmentation | Radiotherapy | .870 |
| Complications of dermopigmentation | Chemotherapy | .964 |
| Complications of dermopigmentation | Type of surgery | .748 |
| Treatment preference | Age | .267 |
| Areolar colour | Chemotherapy | .968 |
| Areolar colour | Age | .989 |
| Areolar colour | Radiotherapy | .251 |
| Anaesthesia | Complications of dermopigmentation | .772 |
| Size of NAC | Type of surgery | .181 |
In the present study, we observe that the patients who underwent reconstructive breast surgery showed a high degree of satisfaction with dermopigmentation but reiterate the lack of colour permanence and the desire to obtain longer lasting results.
The profile of the patients who underwent the procedure shows that they had few comorbidities, and most had undergone previous chemotherapy and/or radiotherapy treatment. Most of the patients underwent surgery with an autologous, deep inferior epigastric perforator (DIEP) flap reconstruction or fixed volume implants. They then underwent surgical reconstruction of the NAC and the average satisfaction with its results was high. The analysis indicates that patients with larger NAC size reported a higher level of satisfaction than those who had NAC reconstruction. Even so, it should be noted that a significant number of patients stated that the result in relation to the size and/or projection of the neo-nipple was low, stating that it was small in relation to the expected results, which is consistent with the data published to date.2,13 It was not possible to investigate the relationship between this factor and variables such as age, neo/adjuvant chemotherapy, neo/adjuvant radiotherapy, or the type of previous breast reconstruction, and the data published to date do not allow conclusions to be drawn in this respect.2 The results are also consistent with a low complication rate,1 which in this case should only be extrapolated to trilobed flap reconstruction because most of the patients in the sample underwent this procedure, thus excluding other reconstructions.
In line with the data from previous studies, the degree of satisfaction with dermopigmentation was high, as was satisfaction with the areolar size, most of the women stating that they would undergo it again.4,9 With regard to complications, the data are similar to published studies, and the most frequently reported complication was pain during the procedure,4,5,8,9 where no relationship was observed between the complication variable and the use of topical anaesthesia. Nurses performed the treatment, and although in the present study it is not possible to contrast the data with the performance of the technique by other professionals such as tattoo artists, the relationship of this variable with the rate of complications and satisfaction is a present line of study.8,11,14
Ninety-one percent of the sample indicated that the colour had faded, which is expected and in line with the results published to date given the characteristics of the technique and the pigments used (Eurotouch®).3,5,13,15 Older patients and those with previous chemotherapy treatment showed less duration of the colour over time (statistically significant differences were detected in all of them), a fact to be considered in clinical practice.
Finally, it should be noted that if the patients were given the choice between dermopigmentation or permanent tattooing, more than half of them would choose tattooing; the main differences between dermopigmentation (pigments) and permanent tattooing are based on the depth of insertion and the composition of the product used.6,13 In the medical field, there is controversy and no consensus on the use of pigments and/or permanent inks13; the published data are not conclusive and do not consider aspects such as breast reoperation rates (due to recurrence of disease or complications such as encapsulation of prostheses) and the aesthetic changes that this may entail in the breast, the effect of treatments such as radiotherapy and/or chemotherapy, or the effect of skin degradation caused by potential repetition of treatments in the area to be treated.6 Pigments are used in Spain and most countries, which could be for legal (homologation), safety, or tradition reasons, as yet unknown, and therefore, there are limitations such as lack of permanence.4,13
One of the strengths of the study is that it is the first Spanish study to evaluate satisfaction with the technique with a large number of patients in a referral centre with years of experience performing this procedure. Furthermore, this project is specifically led by nurses and opens up a new field of study in the profession.
The limitations of the study include the lack of justification in high-quality literature of the subject under study and the lack of a validated questionnaire; given that dermopigmentation and tattooing are techniques that were primarily performed by non-health professionals, the contents published to date are scarce and not very up-to-date, and there is a lack of data regarding evaluation of the programmes, protocolisation of the technique, complications, the relationship with previous procedures or pathologies, and/or the durability of the treatment.4,6–8 For this reason, prior to the study, the questionnaire was adapted and validated for comprehension, including four new questions.
We could also consider the lack of a larger sample as a limitation, as this could limit the associative analysis between variables. Finally, the telephone participation of the patients could be a limiting factor, as there could be response bias and/or errors in the transcription of data.
Future analytical studies would be justified, as well as validating the instrument and/or looking for causal relationships between the variables under study, such as the relationship between treatments, durability, and satisfaction. Future randomised studies would even be indicated to compare the impact of different pigmentation or tattooing procedures in relation to durability, user satisfaction, and/or complications.13,14
ConclusionsPatients who underwent reconstructive breast surgery showed a high degree of satisfaction with the results of areolar dermopigmentation and surgical reconstruction of the NAC. The results confirm that NAC reconstruction does not entail significant risks for patients, but it often does not offer the expected projection, although this does not affect patient satisfaction.
With regard to dermopigmentation, the data reiterate the safety of this treatment given in healthcare centres. In addition, a lack of durability and permanence of the pigments in the skin is shown and it is observed that patients want permanent or more lasting results such as those offered by the permanent tattoo technique, thus opening up new lines of future treatments and/or research studies.
FundingThis project obtained partial support from the Research Committee in the HUB's 2022 call for research project awards in care. No other specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research study.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all the participating patients, without whose opinion and participation the study would not have been possible, and the HUB (Nursing Support Service for Information Systems and Research in Care) for their collaboration.