Case report is a narrative description of the problem of one or several patients. The CARE checklist (CAse REport) is the consensus document for reporting clinical case reports and through adaptations to the different CARE disciplines is used to define standards for authors in scientific journals; however, the specificity of the nursing process makes it difficult to adjust nursing case reports to CARE. The aim was to analyze the publications of clinical cases with a nursing perspective in scientific journals, as well as the quality standards and evaluation systems used. Few journals reviewed agreed to publish nursing case reports or stated standards for authors to adjust to CARE. Preliminary results indicated average or poor adherence to CARE, with the most reported elements being: Keywords, patient information and introduction. Adherence was lower for the elements: Timeline, therapeutic intervention, follow-up and outcomes, and patient perspective. The characteristics of the nursing process implies a low adherence to CARE, so it is necessary to unify criteria to guide researchers, authors, reviewers and editors of scientific journals, as well as to improve the rigor and quality of the reports. Currently, there are no specific guidelines for reporting clinical case reports with a nursing perspective available. These normative gaps could be solved by developing a CARE extension adapted to the methodological characteristics of the nursing process.
El informe de un caso clínico es una narración detallada que describe el problema de uno o varios pacientes. La lista de comprobación CARE (CAse REport) es el documento de consenso para reportar los informes de casos clínicos y a través de adaptaciones a las diferentes disciplinas CARE es utilizada para definir las normas a los autores en revistas científicas; no obstante, la especificidad del proceso enfermero dificulta ajustar los informes de casos enfermeros a CARE. El objetivo de este artículo es analizar las publicaciones de casos clínicos con perspectiva enfermera en revistas científicas, así como analizar los estándares de calidad y sistemas de evaluación utilizados. Pocas revistas consultadas aceptaron publicar informes de casos enfermeros o declararon normas a los autores para ajustarse a CARE. Los resultados preliminares indicaron adherencia media o pobre a CARE, siendo los elementos más reportados: Palabras clave, información del paciente e introducción. La adherencia fue menor para los elementos: Calendario, intervención terapéutica, seguimiento y resultados y perspectiva del paciente. Las características del proceso enfermero implican una baja adherencia a CARE, por lo que es preciso unificar criterios para guiar a los investigadores, autores, revisores y editores de revistas científicas y mejorar el rigor y la calidad de los informes. En la actualidad, no existen directrices específicas para la presentación de informes de casos clínicos con perspectiva enfermera. Estas carencias normativas podrían solventarse desarrollando una extensión CARE adaptada a las características metodológicas del proceso enfermero.
The nursing discipline is underpinned by a broad theoretical framework that includes adherence to its own precepts and conceptual systems as well as others imported from other disciplines without the necessary critical analysis, which results in some variability in the clinical practice of nurses1,2; all while awaiting the development of a general theory of its own.3 Nursing clinical practice is also affected by the high level of complexity intrinsic to human responses, which requires a holistic approach through multiple interventions in constant interaction, and this leads to variability, flexibility and uncertainty1,2 causing inaccuracy and lack of assimilation by many nurses.4 This situation has resulted in a conglomerate or paradigmatic cross-fertilisation of epistemic currents that must be consolidated with a progressive, solid, rigorous, organised, and unidirectional theoretical foundation, which is necessary for the upward and consolidated progress of the discipline. The nursing process (NP) is the scientific and systematic method of clinical reasoning used by nurses to make decisions with which to provide comprehensive, safe, and quality care.5,6 This form of reasoning involves the combination of critical thinking processes and reflective practice,7 as well as the development of skills to identify, judge, and resolve human responses to health conditions and life processes, or the susceptibility to that response presented by an individual, family, group or community.8
Since Hall introduced the concept of NP, its development and conceptualisation has evolved gradually and in parallel with nurses’ scientific autonomy and disciplinary competencies.2 However, although this development of NP signals an evolution towards a structured and holistic care paradigm reflecting the dynamic nature of nursing, it has not developed as expected on the international scene, with limitations of approach, systematic projection, and critical reflection3; such that inaccuracies, omissions, or excesses in NP translate into uncertainties in nursing.
The NP is now an essential part of nursing practice to provide individualised, patient-centred, outcome-oriented care. The clinical use of NP involves scientific reasoning, which implies that nurses must analyse, interpret, and evaluate information reflectively, considering diverse perspectives, and making informed decisions in complex and changing situations. In this effective problem-solving model,9 in addition to professional competencies, there are other elements that intervene and influence the correct clinical application of NP, such as patient characteristics, and organisational factors.10 The NP has gradually evolved towards what has been termed advanced NP, which proposes the implementation in each of its stages of the different standardised language systems as defined, validated, and recognised by the American Nurses Association (ANA) in the international context,11,12 including diagnostic concepts, interventions, and standardised nursing outcomes; all explained with a scientific basis using valid assessment tools.10,13 Moreover, the quality with which the advanced NP is put into practice is influenced by the knowledge, skills, and attitudes of nurses, giving them competence in clinical decision making.9
This decision-making process involves the five stages of NP, which include:
- •
Assessment: collecting information on a patient's physiological, psychological, socio-cultural, spiritual, economic, and lifestyle.
- •
Diagnosis: Systematic analysis and interpretation of data and development of inferences and hypotheses for clinical judgement about responses to actual or potential health conditions or needs.
- •
Planning: Prioritisation of identified problems and care needs and setting measurable and achievable short- and long-term goals and prescribing interventions required to achieve them.
- •
Implementation: Putting into practice of the planned care, reassessing the person and evaluating their response to achieve the expected outcomes, according to the objectives set with the aim of improving or resolving the problems.
- •
Evaluation: Continuous monitoring and evaluation of the progress of the patient's state of health and the effectiveness of interventions to check the adequacy of the care plan (CP) and to implement modifications as necessary.5,14 Evaluation is a final, cross-cutting step throughout the NP.
The NP stages are internationally recognised as having the theoretical elements necessary to provide accurate nursing documentation.15 In this sense, the CP is the element used by nurses to represent the NP, integrate, and organise information and establish correspondence between the data and the reality observed,16 which facilitates communication within the interdisciplinary team and contributes to the quality of patient care and safety.17 In the care setting, nurses record this information on the health process of individuals in electronic health records (EHR). Several instruments have been developed to assess this documentation, including Q-DIO (Quality of Diagnoses, Interventions, and Outcomes),18,19 NoGA Instrument,20 Cat-ch-ing Instrument,21 QOD (Quality of Nursing Diagnosis),22 and D-Cath Instrument.23 These tools have been designed to assess the structure, process, and content of the records. However, some of them only assess specific aspects (structure, process, or content) making it difficult to approach these records accurately. However, these instruments were not designed to assess the quality of nursing case reports.
Outcome reporting guidelines for presenting health science reportsThe reporting of research results in the health sciences should be thorough and rigorous so as to minimise biased publications of low value. To ensure this, the SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence) guidelines provide a common general framework for reporting new knowledge originating from different methodological approaches, improving the quality, safety, and value of healthcare in the scientific literature.24 However, to achieve this, efforts and resources are required that are standardised and regulated by individual standards for each research design using outcome reporting guidelines.
An outcome reporting guide is a structured and simple tool to be used by health science researchers when writing their manuscripts following reporting guidelines that include the minimum information necessary to ensure that they can be understood and replicated. The EQUATOR (Enhancing the QUAlity and Transparency Of health Research) network25 is a coordinated international initiative that aims to aggregate the outcomes of work done by individual groups to improve the reliability and value of scientific output in the health sciences by encouraging transparent and accurate reporting through robust outcome reporting guidelines. The EQUATOR network includes 576 guidelines with their respective extensions for different types of research designs and clinical areas, including the CAse REport (CARE) standards for clinical cases.25
Regarding clinical cases, a case report is a detailed narrative representation describing, for clinical, scientific, or educational purposes, a problem experienced by one or more patients26,27 with a rare disease or complication.27,28 There are different types of case reports according to different perspectives and authors, detailed below.
From a social science perspective, according to Yin29 case reports can be divided into two types:
- •
Embedded case reports: These integrate a main sub-unit of analysis and other secondary sub-units that incorporate aspects of analysis that pertain to other domains, services or professionals involved in the care process.
- •
Holistic case reports: Case studies with a single unit of analysis that focus only on the global nature of a phenomenon without examining other specific phenomena in operational detail.
Stake30 classifies case reports into three types:
- •
Intrinsic case reports: which aim to gain a better understanding of a particular case, rather than specific phenomena, without concern for theory building or transferability.
- •
Instrumental case reports: In which the researcher approaches a case for in-depth exploration of a particular aspect in order to answer a research question. The main difference between an intrinsic and instrumental case study is not the case, but the purpose of the case study, although it is not easy to draw clear lines of distinction between the two.
- •
Collective case reports: These focus on the study of several cases with the aim of comparatively understanding a common characteristic or phenomenon in a population.31
On the other hand, according to the classification proposed by Green and Johnson in the field of health sciences, case reports can be of three types32:
- •
Diagnostic case reports: Describe and discuss the diagnostic or analytic methods used to evaluate a patient. These cases present a diagnosis that is rare, confusing, or difficult to render, but often do not discuss treatment.
- •
Management case reports: Describe and discuss the full management of a patient, including how the patient is assessed and managed, providing the reader with an in-depth understanding of the case.
- •
Educational case reports: used to provide readers with current practice strategies while providing a brief review of the literature. While the case used to frame the educational experience may not be new, the manner in which the article is written should provide a new perspective on the topic under study.
In the clinical nursing setting, there is little background on the development and writing of case reports using the NP. Of note is the study by Sasa33 which addressed writing skills to develop critical thinking, deep learning, and reflective practice in the writing of a CP in nursing students. While, from the structural perspective of a CP, Siedlecki34 described the logical sequence of aspects to be taken into account in the process of developing and writing a clinical case study in nursing, which includes a preparatory stage in which the literature must be reviewed, the theoretical framework of the case and the key elements identified; a second stage of information collection and management; a third stage of analysis of the data that will make up the report; and finally, the dissemination stage through the organisation of the findings and writing of the manuscript.
Based on the contents of a nursing case study, some guidelines have been developed towards structural improvements of these reports. Siedlecki34 listed the elements that should be included in a case report: title, problem addressed, theoretical justification of the case, research question, relevance of the case, scientific evidence, analysis, summary of findings, and conclusions. This author also described some criteria of rigour that should be contemplated in a case report, such as: construct validity, conformity, credibility or internal validity, transferability or external validity, and reliability. Likewise, Tirado-Pedregosa et al.35 described and proposed a checklist with suggestions for writing and setting the structure of the case based on the use of the standardised language systems NANDA International (NANDA-I), Nursing Outcome Classification (NOC), and Nursing Interventions Classification (NIC), covering each of the sections it should contain, from the title, abstract, introduction, assessment, CP stages, case management, discussion, to the references.
Despite these proposals, in the field of nursing there is no "gold standard"36 for applying the NP in preparing case reports. These contributions are only a starting point for the unification of criteria when reporting a case study with a nursing perspective.
In 2013, the consensus document for reporting clinical case reports, known by its acronym CARE, was developed to optimise the completeness and transparency of case reports through a systematic tool designed to improve the quality of health service delivery.37 The CARE checklist consists of 13 items (title, keywords, abstract, introduction, patient information, clinical findings, timeline, diagnostic assessment, therapeutic intervention, follow-up and outcomes, discussion, patient perspective and informed consent), including a total of 30 elements required for reporting a clinical case report.
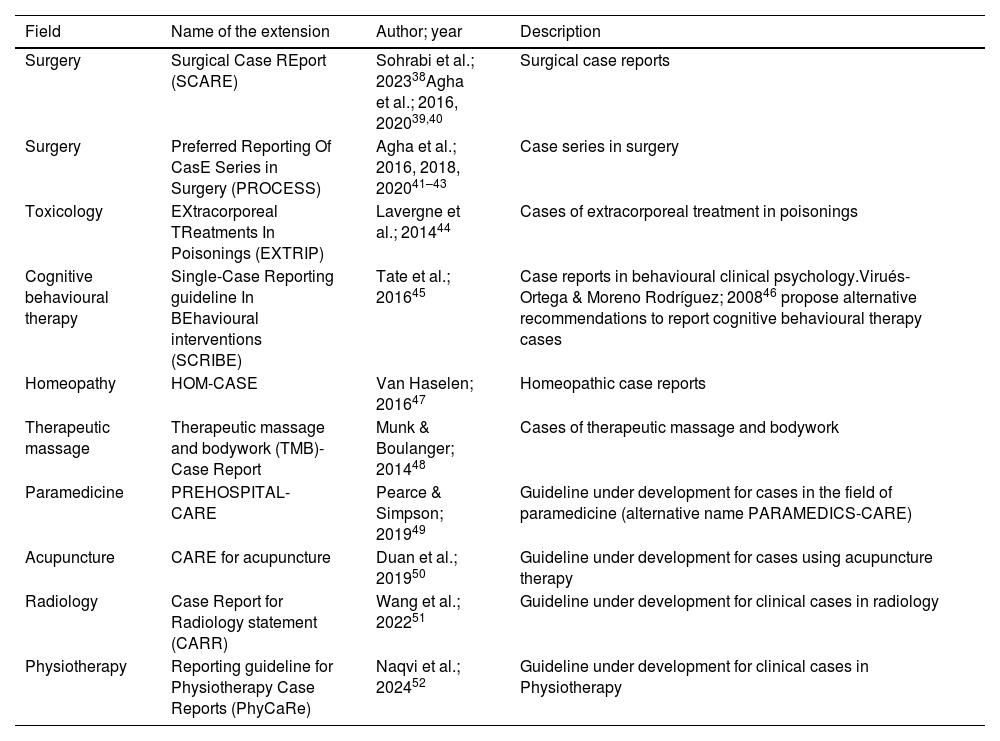
The CARE standards have so far been implemented and adapted to different scientific disciplines and areas of knowledge in health sciences for the purpose of reporting case reports in specific clinical situations, as shown in Table 1. Furthermore, the CReDECI 2 (Criteria for Reporting the Development and Evaluation of Complex Interventions)53,54 guideline is described in the scientific literature with the aim of providing unified criteria for reporting the development and evaluation of interprofessional interventions, which are fraught with complexity, and which are undertaken during the care process.
Adaptations of CARE standards.
| Field | Name of the extension | Author; year | Description |
|---|---|---|---|
| Surgery | Surgical Case REport (SCARE) | Sohrabi et al.; 202338Agha et al.; 2016, 202039,40 | Surgical case reports |
| Surgery | Preferred Reporting Of CasE Series in Surgery (PROCESS) | Agha et al.; 2016, 2018, 202041–43 | Case series in surgery |
| Toxicology | EXtracorporeal TReatments In Poisonings (EXTRIP) | Lavergne et al.; 201444 | Cases of extracorporeal treatment in poisonings |
| Cognitive behavioural therapy | Single-Case Reporting guideline In BEhavioural interventions (SCRIBE) | Tate et al.; 201645 | Case reports in behavioural clinical psychology.Virués-Ortega & Moreno Rodríguez; 200846 propose alternative recommendations to report cognitive behavioural therapy cases |
| Homeopathy | HOM-CASE | Van Haselen; 201647 | Homeopathic case reports |
| Therapeutic massage | Therapeutic massage and bodywork (TMB)-Case Report | Munk & Boulanger; 201448 | Cases of therapeutic massage and bodywork |
| Paramedicine | PREHOSPITAL-CARE | Pearce & Simpson; 201949 | Guideline under development for cases in the field of paramedicine (alternative name PARAMEDICS-CARE) |
| Acupuncture | CARE for acupuncture | Duan et al.; 201950 | Guideline under development for cases using acupuncture therapy |
| Radiology | Case Report for Radiology statement (CARR) | Wang et al.; 202251 | Guideline under development for clinical cases in radiology |
| Physiotherapy | Reporting guideline for Physiotherapy Case Reports (PhyCaRe) | Naqvi et al.; 202452 | Guideline under development for clinical cases in Physiotherapy |
In general, CARE standards are used by publishers and editors of scientific journals in the health sciences to define publication standards for authors. However, in the field of nursing, specific unified decision-support systems have not yet been developed. The aim of this dissertation is to analyse the publications of clinical cases with a nursing perspective in scientific journals, and the quality standards and evaluation systems used.
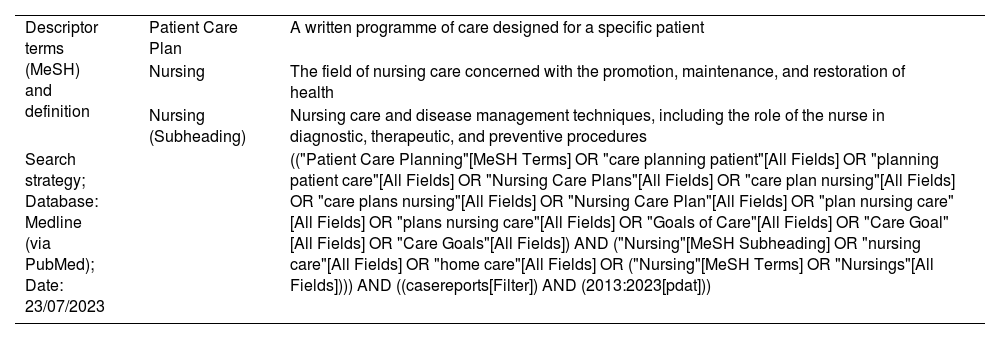
Analysis of the publications of clinical casesWe undertook a literature in the Medline database to estimate the scientific production of clinical cases using the NP in indexed journals and that have employed CARE standards, as shown in Table 2.
Search process.
| Descriptor terms (MeSH) and definition | Patient Care Plan | A written programme of care designed for a specific patient |
| Nursing | The field of nursing care concerned with the promotion, maintenance, and restoration of health | |
| Nursing (Subheading) | Nursing care and disease management techniques, including the role of the nurse in diagnostic, therapeutic, and preventive procedures | |
| Search strategy; Database: Medline (via PubMed); Date: 23/07/2023 | (("Patient Care Planning"[MeSH Terms] OR "care planning patient"[All Fields] OR "planning patient care"[All Fields] OR "Nursing Care Plans"[All Fields] OR "care plan nursing"[All Fields] OR "care plans nursing"[All Fields] OR "Nursing Care Plan"[All Fields] OR "plan nursing care"[All Fields] OR "plans nursing care"[All Fields] OR "Goals of Care"[All Fields] OR "Care Goal"[All Fields] OR "Care Goals"[All Fields]) AND ("Nursing"[MeSH Subheading] OR "nursing care"[All Fields] OR "home care"[All Fields] OR ("Nursing"[MeSH Terms] OR "Nursings"[All Fields]))) AND ((casereports[Filter]) AND (2013:2023[pdat])) |
The number of records retrieved was n = 70. After excluding duplicates (n = 2), they were screened by title and abstract to eliminate those that did not correspond to an NP (n = 34) and those published in languages other than Spanish, English, and Portuguese (n = 16). After the screening process, the number of publications reporting a clinical case using the NP was n = 18. To verify the correct reporting of the information in these publications, the CARE guide was applied to check the degree of adherence to each of its 30 elements. For this, following the proposal of Ravi et al.,55 four levels were established according to the number of elements checked, where 14 or less indicated poor adherence, 15–20 average adherence, 21–26 good adherence, and 27–30 excellent adherence. None of the publications analysed showed excellent or good adherence to CARE elements, half of them showing average adherence and the other half poor adherence.
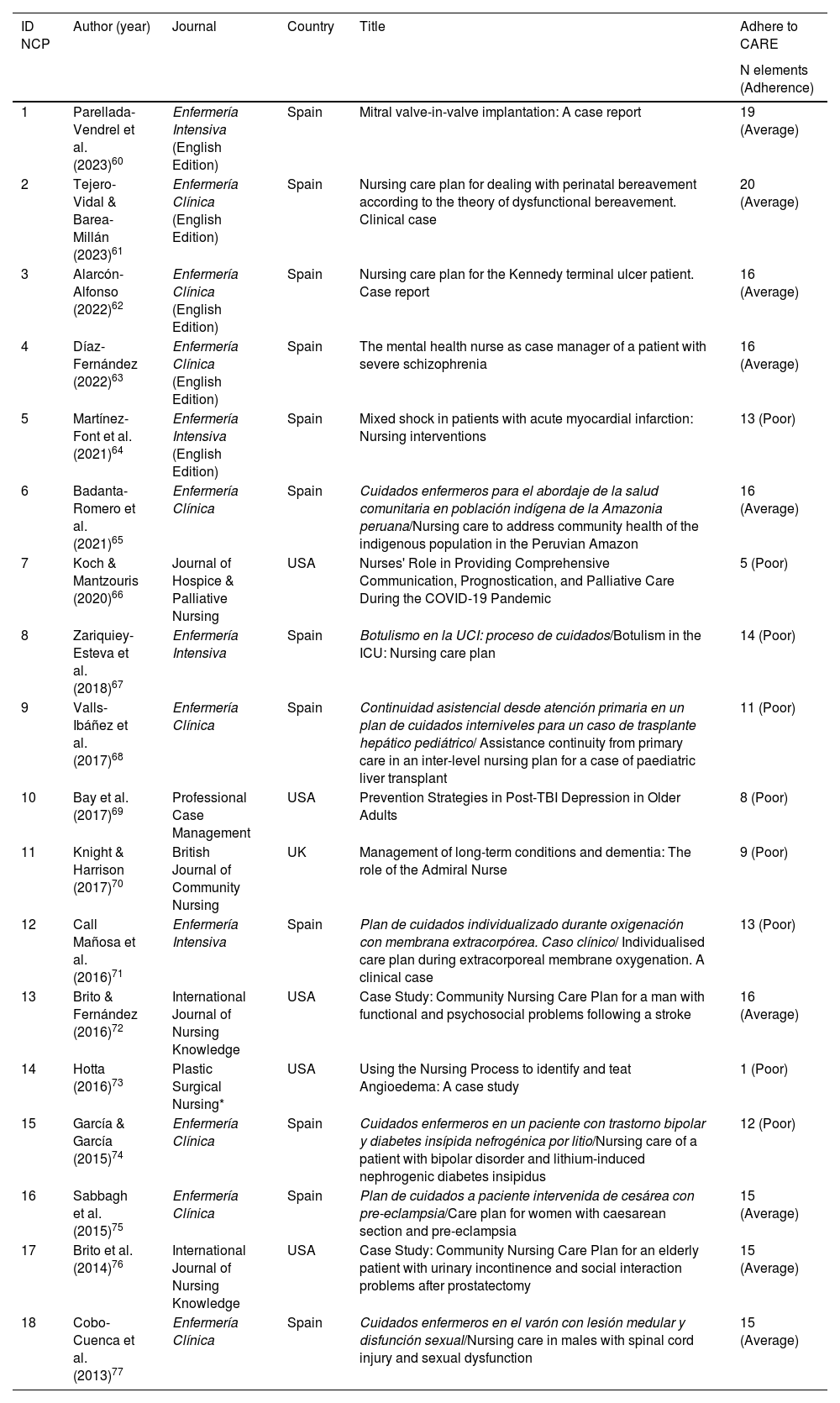
Table 3 shows the characteristics of the included studies and the degree of adherence according to the CARE checklist items.
Characteristics of the included published clinical cases.
| ID NCP | Author (year) | Journal | Country | Title | Adhere to CARE |
|---|---|---|---|---|---|
| N elements (Adherence) | |||||
| 1 | Parellada-Vendrel et al. (2023)60 | Enfermería Intensiva (English Edition) | Spain | Mitral valve-in-valve implantation: A case report | 19 (Average) |
| 2 | Tejero-Vidal & Barea-Millán (2023)61 | Enfermería Clínica (English Edition) | Spain | Nursing care plan for dealing with perinatal bereavement according to the theory of dysfunctional bereavement. Clinical case | 20 (Average) |
| 3 | Alarcón-Alfonso (2022)62 | Enfermería Clínica (English Edition) | Spain | Nursing care plan for the Kennedy terminal ulcer patient. Case report | 16 (Average) |
| 4 | Díaz-Fernández (2022)63 | Enfermería Clínica (English Edition) | Spain | The mental health nurse as case manager of a patient with severe schizophrenia | 16 (Average) |
| 5 | Martínez-Font et al. (2021)64 | Enfermería Intensiva (English Edition) | Spain | Mixed shock in patients with acute myocardial infarction: Nursing interventions | 13 (Poor) |
| 6 | Badanta-Romero et al. (2021)65 | Enfermería Clínica | Spain | Cuidados enfermeros para el abordaje de la salud comunitaria en población indígena de la Amazonia peruana/Nursing care to address community health of the indigenous population in the Peruvian Amazon | 16 (Average) |
| 7 | Koch & Mantzouris (2020)66 | Journal of Hospice & Palliative Nursing | USA | Nurses' Role in Providing Comprehensive Communication, Prognostication, and Palliative Care During the COVID-19 Pandemic | 5 (Poor) |
| 8 | Zariquiey-Esteva et al. (2018)67 | Enfermería Intensiva | Spain | Botulismo en la UCI: proceso de cuidados/Botulism in the ICU: Nursing care plan | 14 (Poor) |
| 9 | Valls-Ibáñez et al. (2017)68 | Enfermería Clínica | Spain | Continuidad asistencial desde atención primaria en un plan de cuidados interniveles para un caso de trasplante hepático pediátrico/ Assistance continuity from primary care in an inter-level nursing plan for a case of paediatric liver transplant | 11 (Poor) |
| 10 | Bay et al. (2017)69 | Professional Case Management | USA | Prevention Strategies in Post-TBI Depression in Older Adults | 8 (Poor) |
| 11 | Knight & Harrison (2017)70 | British Journal of Community Nursing | UK | Management of long-term conditions and dementia: The role of the Admiral Nurse | 9 (Poor) |
| 12 | Call Mañosa et al. (2016)71 | Enfermería Intensiva | Spain | Plan de cuidados individualizado durante oxigenación con membrana extracorpórea. Caso clínico/ Individualised care plan during extracorporeal membrane oxygenation. A clinical case | 13 (Poor) |
| 13 | Brito & Fernández (2016)72 | International Journal of Nursing Knowledge | USA | Case Study: Community Nursing Care Plan for a man with functional and psychosocial problems following a stroke | 16 (Average) |
| 14 | Hotta (2016)73 | Plastic Surgical Nursing* | USA | Using the Nursing Process to identify and teat Angioedema: A case study | 1 (Poor) |
| 15 | García & García (2015)74 | Enfermería Clínica | Spain | Cuidados enfermeros en un paciente con trastorno bipolar y diabetes insípida nefrogénica por litio/Nursing care of a patient with bipolar disorder and lithium-induced nephrogenic diabetes insipidus | 12 (Poor) |
| 16 | Sabbagh et al. (2015)75 | Enfermería Clínica | Spain | Plan de cuidados a paciente intervenida de cesárea con pre-eclampsia/Care plan for women with caesarean section and pre-eclampsia | 15 (Average) |
| 17 | Brito et al. (2014)76 | International Journal of Nursing Knowledge | USA | Case Study: Community Nursing Care Plan for an elderly patient with urinary incontinence and social interaction problems after prostatectomy | 15 (Average) |
| 18 | Cobo-Cuenca et al. (2013)77 | Enfermería Clínica | Spain | Cuidados enfermeros en el varón con lesión medular y disfunción sexual/Nursing care in males with spinal cord injury and sexual dysfunction | 15 (Average) |
ID NCP: Identifier of the nursing care plan; *Current name of the journal: Plastic and Aesthetic Nursing.
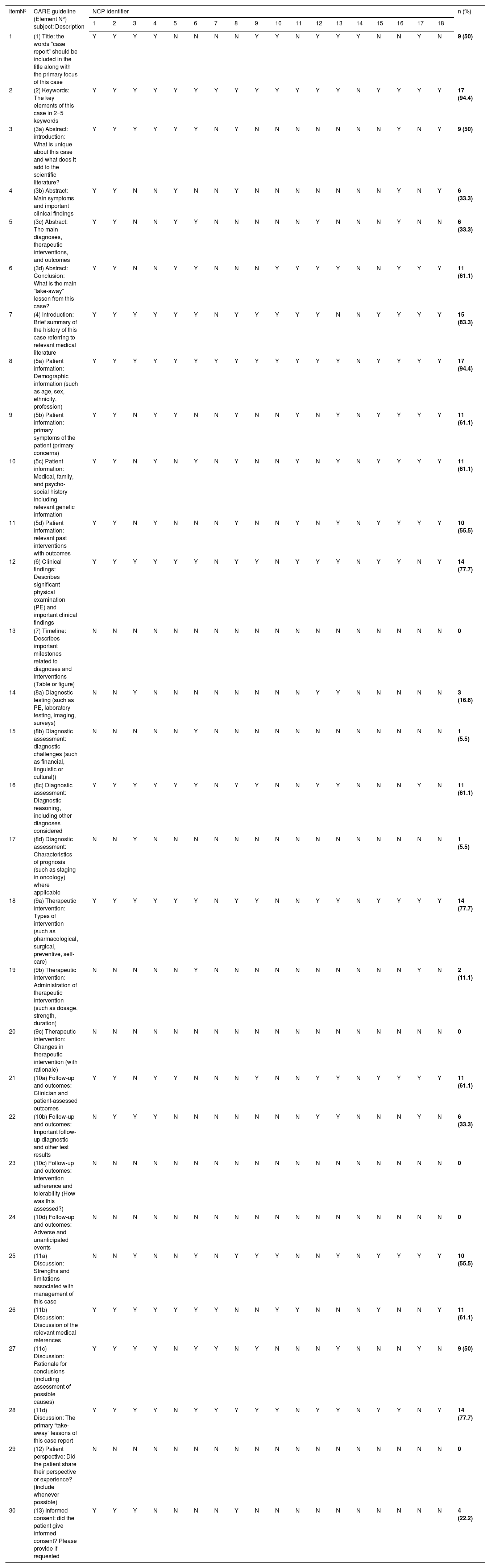
The most reported items were keywords (item 2) and patient information (item 5a) in n = 17 (94.4%) studies. Next, the introduction (item 4) was completed in n = 15 (83.3%) studies. The elements with the poorest adherence, which were never reported, were timeline (element 7), therapeutic intervention (element 9c), follow-up and outcomes (element 10c and element 10d), and patient perspective (element 12), while the diagnostic assessment elements (element 8b and element 8d) were completed only n = 1 (5.5%) time, as shown in Table 4.
Compliance with CARE checklist items in clinical cases.
| ItemNº | CARE guideline (Element Nº) subject: Description | NCP identifier | n (%) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |||
| 1 | (1) Title: the words "case report" should be included in the title along with the primary focus of this case | Y | Y | Y | Y | N | N | N | N | Y | Y | N | Y | Y | Y | N | N | Y | N | 9 (50) |
| 2 | (2) Keywords: The key elements of this case in 2−5 keywords | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | 17 (94.4) |
| 3 | (3a) Abstract: introduction: What is unique about this case and what does it add to the scientific literature? | Y | Y | Y | Y | Y | Y | N | Y | N | N | N | N | N | N | N | Y | N | Y | 9 (50) |
| 4 | (3b) Abstract: Main symptoms and important clinical findings | Y | Y | N | N | Y | N | N | Y | N | N | N | N | N | N | N | Y | N | Y | 6 (33.3) |
| 5 | (3c) Abstract: The main diagnoses, therapeutic interventions, and outcomes | Y | Y | N | N | Y | Y | N | N | N | N | N | Y | N | N | N | Y | N | N | 6 (33.3) |
| 6 | (3d) Abstract: Conclusion: What is the main “take-away” lesson from this case? | Y | Y | N | N | Y | Y | N | N | N | Y | Y | Y | Y | N | N | Y | Y | Y | 11 (61.1) |
| 7 | (4) Introduction: Brief summary of the history of this case referring to relevant medical literature | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | N | N | Y | Y | Y | Y | 15 (83.3) |
| 8 | (5a) Patient information: Demographic information (such as age, sex, ethnicity, profession) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | 17 (94.4) |
| 9 | (5b) Patient information: primary symptoms of the patient (primary concerns) | Y | Y | N | Y | Y | N | N | Y | N | N | Y | N | Y | N | Y | Y | Y | Y | 11 (61.1) |
| 10 | (5c) Patient information: Medical, family, and psycho-social history including relevant genetic information | Y | Y | N | Y | N | Y | N | Y | N | N | Y | N | Y | N | Y | Y | Y | Y | 11 (61.1) |
| 11 | (5d) Patient information: relevant past interventions with outcomes | Y | Y | N | Y | N | N | N | Y | N | N | Y | N | Y | N | Y | Y | Y | Y | 10 (55.5) |
| 12 | (6) Clinical findings: Describes significant physical examination (PE) and important clinical findings | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | N | Y | Y | N | Y | 14 (77.7) |
| 13 | (7) Timeline: Describes important milestones related to diagnoses and interventions (Table or figure) | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 |
| 14 | (8a) Diagnostic testing (such as PE, laboratory testing, imaging, surveys) | N | N | Y | N | N | N | N | N | N | N | N | Y | Y | N | N | N | N | N | 3 (16.6) |
| 15 | (8b) Diagnostic assessment: diagnostic challenges (such as financial, linguistic or cultural)) | N | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | N | N | N | 1 (5.5) |
| 16 | (8c) Diagnostic assessment: Diagnostic reasoning, including other diagnoses considered | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y | Y | N | N | N | Y | N | 11 (61.1) |
| 17 | (8d) Diagnostic assessment: Characteristics of prognosis (such as staging in oncology) where applicable | N | N | Y | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 1 (5.5) |
| 18 | (9a) Therapeutic intervention: Types of intervention (such as pharmacological, surgical, preventive, self-care) | Y | Y | Y | Y | Y | Y | N | Y | Y | N | N | Y | Y | N | Y | Y | Y | Y | 14 (77.7) |
| 19 | (9b) Therapeutic intervention: Administration of therapeutic intervention (such as dosage, strength, duration) | N | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | N | Y | N | 2 (11.1) |
| 20 | (9c) Therapeutic intervention: Changes in therapeutic intervention (with rationale) | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 |
| 21 | (10a) Follow-up and outcomes: Clinician and patient-assessed outcomes | Y | Y | N | Y | Y | N | N | N | Y | N | N | Y | Y | N | Y | Y | Y | Y | 11 (61.1) |
| 22 | (10b) Follow-up and outcomes: Important follow-up diagnostic and other test results | N | Y | Y | Y | N | N | N | N | N | N | N | Y | Y | N | N | N | Y | N | 6 (33.3) |
| 23 | (10c) Follow-up and outcomes: Intervention adherence and tolerability (How was this assessed?) | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 |
| 24 | (10d) Follow-up and outcomes: Adverse and unanticipated events | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 |
| 25 | (11a) Discussion: Strengths and limitations associated with management of this case | N | N | Y | N | N | Y | N | Y | Y | Y | N | N | Y | N | Y | Y | Y | Y | 10 (55.5) |
| 26 | (11b) Discussion: Discussion of the relevant medical references | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | N | N | Y | N | N | Y | 11 (61.1) |
| 27 | (11c) Discussion: Rationale for conclusions (including assessment of possible causes) | Y | Y | Y | Y | N | Y | Y | N | Y | N | N | N | Y | N | N | N | Y | N | 9 (50) |
| 28 | (11d) Discussion: The primary “take-away” lessons of this case report | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | N | Y | 14 (77.7) |
| 29 | (12) Patient perspective: Did the patient share their perspective or experience? (Include whenever possible) | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 |
| 30 | (13) Informed consent: did the patient give informed consent? Please provide if requested | Y | Y | Y | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | N | 4 (22.2) |
NCP: Nursing care plan; Y: yes; N: No.
We also undertook a search in Scimago Journal Rank (SJR) to identify journals that accepted nursing case reports among their publications. The inclusion criteria were journals that corresponded to the 2022 ranking. Filters were applied to limit searches to the area of knowledge "Nursing", the category "Nursing (Miscellaneous)" and the type of support "Journals", retrieving n = 159 journals. After consulting the publication guidelines, we found that n = 53 journals declared that they considered nursing clinical cases for publication. Of these, n = 23 journals did not indicate any rules to authors for the preparation of reports, n = 26 stated among their rules specific instructions on aspects related to length, structure, number of Tables and Figures, literature references and use of standardised nursing terminology, among other aspects. Only n = 6 journals were identified that referred to the CARE guidelines.
In addition, the publication standards of the journals that were retrieved through the preliminary search in Medline were consulted in which clinical case reports developed with the NP were identified and did not fall into the SJR category "Nursing (Miscellaneous)". Of these, only n = 1 referred to the CARE guideline, n = 1 provided specific instructions, and n = 4 did not provide any guidelines to authors for preparing a case report. The name of the journals, the SJR quartile in which they are listed, the country of publication, and the author guidelines described on each journal's website can be found in Supplementary File 1.
DiscussionThe guidelines for reporting results adapt to each of the methodological research designs, which are necessary for the correct drafting of the different types of manuscripts and contribute to the scientific quality required for publication.25 These guidelines are designed to provide researchers with clear and detailed guidelines on how to present their outcomes completely and scrupulously in scientific manuscripts. Indirectly, they are instruments with which the quality of scientific publications in the field of health sciences can be assessed. These guidelines have been developed with the aim of reducing uncertainty about what information is considered important in publications, with the ultimate goal of improving healthcare by emphasising completeness, accuracy, and transparency.56 In summary, outcome reporting guidelines serve several purposes, which include improving methodological quality, providing transparency and reproducibility, facilitating peer review, and becoming tools for critical reading.
In relation to case reports, the CARE standards cover the qualities that this type of publication must meet. Scientific knowledge generated through the results of clinical case reports often do not provide new knowledge,32 are not generalisable, do not address causal inference and explanatory mechanisms, and do not provide robust evidence compared to other research study designs. However, they can be a relevant and creative alternative way to update clinical practice and training by emphasising the patient's perspective as central to the process.57 Therefore, case reports should be reported as fully as possible to ensure their correct evaluation and potential usefulness.28 Thus, the case study method can be an additional creative alternative to traditional approaches in training and research.
Regarding the overall adherence of case study publications to CARE standards, Ravi et al.55 reviewed n = 36 medical journals in the Indian context with n = 1,178 published reports, of which none had excellent adherence; these authors identified good adherence 19%, average 70.7%, and poor adherence 10%. However, Yang et al.56 reviewed n = 184 nursing reports in n = 16 journals indexed in Science Citation Index (SCI) 37% were high quality (95% CI 30.0%–44.4%), 52.7% middle quality (95% CI 45.2%–60.1%), and 10.3% low quality (95% CI 6.3%–15.7%). This is similar to that observed in our preliminary search, with average adherence at 50% and poor adherence at 50%. On another note, Seguel-Moraga et al.54 analysed the quality of n = 201 clinical cases in the field of dentistry; using a score range 7–20 they noted that the reports were close to the average value (14.3 ± 2.6).
Finally, Moradi et al.59 reviewed n = 100 reviewed n = 100 surgical clinical cases in urology using the SCARE guide, with 49% adherence (Range: 21 %–79 %).
In our analysis, the CARE elements that showed the best adherence were keywords and patient information (n = 17; 94.4%), followed by introduction (n = 15; 83.3%); in third place were clinical findings, types of therapeutic intervention, and main lessons to be learned from the case (n = 14; 77.7%). in that they observed better adherence for clinical findings 97.9%, keywords 88.5%, and introduction 71.5%. Yang et al.52 found that the patient's socio-demographic information (n = 167; 90.8%; CI: 85.6–94.5), clinical findings (n = 171; 92.9%; CI: 88.2–96.2), diagnostic reasoning (n = 182; 98.9%; CI: 96.1–99.9), therapeutic intervention (n = 179; 97.3%; CI: 93.8–99.1), and main take-away lessons (n = 171; 92.9%; CI: 88.2–96.2) were best reported. However, for Seguel-Moraga et al.54 the best results were clinical findings 91.5% and introduction 81.1%. Finally, for Moradi et al.55 the highest scores were introduction at 77%, additional information at 75%, patient information at 65%, and abstract at 66%.
Regarding the CARE elements with the poorest adherence, it was observed that timeline, therapeutic intervention, follow-up and outcomes, and patient perspective showed 0% adherence, followed by diagnostic assessment (n = 1; 5.5%). These results were similar to those obtained by Ravi et al.55 for patient perspective 0%, informed consent 2.8%, and timeline 4.6%. On the other hand, Yang et al.56 identified medical, family, and psychosocial history (n = 13, 7.1% CI 3.8–11.8), diagnostic assessment of prognostic characteristics (n = 3, 1.6% CI 0.3–4.7), and follow-up and outcomes (n = 12, 6.5% CI 3.4–11.1) as the elements least reported. For Seguel-Moraga et al.,58 the elements with the lowest adherence were patient perspective 0%, timeline 1%, and informed consent 2%. Finally, for Moradi et al.,59 the lowest scores were for patient perspective 1% and keywords 3%.
Regarding the date of implementation of the CARE guidelines, according to Seguel-Moraga et al.58 cases published before implementing CARE (n = 171; mean = 14.3 ± 2.6) and after CARE (n = 30; mean = 14.7 ± 2.7) showed no statistically significant differences (p = .39). These results contrast with those reported by Yang et al.56 who found that, after the CARE guidelines, keywords (OR = .42; 95% CI: .19–.92; p = .03), introduction (OR = .35; 95% CI: .15–.83; p = .017), and discussion (OR = .19; 95% CI: .06–.56; p = .003) were better reported. Ravi et al.55 concluded that adherence to the CARE guideline increased in journals with impact factor >1 (OR = 16.4; CI: 9.3–17.8; p < .001). In contrast, Yang et al.56 found no statistically significant difference after setting the cut-off point for impact factor at <1.8 (mean = 13.3; ±2.3) versus impact factor ≥1.8 (mean = 13.6; ±2.4) (p = .4977).
A systematic review of clinical case reports published in indexed journals is required to contrast this association in the context of nursing care. However, Ravi et al.55 reported higher overall adherence in specialist journals (n = 21; mean = 64.81; ±8.7) compared to general journals (n = 6; mean = 58.15; ±7.9) (p < .001) and super-specialist journals (n = 9; mean = 59.14; ±9.4) (p < .001). In terms of the websites consulted, of the n = 164 journals that indicated publishing clinical cases, only n = 7 indicated in the guidelines to authors the need to adhere to the CARE guidelines, implying a very low number; these results coincide with the review conducted by Ravi et al.,55 in which only n = 1 journal out of n = 36 had adopted the CARE guidelines.
Following these contrasting results, the reviews by Ravi et al.,55 Sequel-Moraga et al.,58 Moradi et al.,59 and Yang et al.56 noted that clinical case reports are deficient in adhering to CARE standards, showing a general lack of essential elements. Although more comprehensive studies are needed to conclude the quality of case reports,59 this scenario suggests that journals could improve their quality by requiring authors, reviewers, and editors to use CARE guidelines or their extensions.55,58
In the context of nursing care, as per the proposals by Tirado-Pedregosa et al.35 and Siedlecki,34 the following aspects should be addressed to produce a CARE compliant case report: presentation of the case through a precise title and detailed exposition of the relevance and pertinence of the problem being addressed, including a theoretical rationale with a nursing perspective; a concise and exhaustive description of the patient, including relevant socio-demographic data and a brief history taking, clinical history, nursing assessment, and physical examination that provides the relevant findings for the case; the process followed to establish the diagnostic reasoning and differential diagnosis, detailing the therapeutic approaches used and the choice of interventions, activities, care, and procedures performed as justified from the scientific evidence; the main findings and the clinical progression of the patient and the response to the CP including a chronological description, highlighting important changes in the evolution of health status, responses to interventions and relevant events. Furthermore, a discussion is required including analysis and interpretation of the findings and clinical challenges supported by the existing literature. Finally, conclusions should be described, highlighting “take-away” lessons, key points, and practical considerations arising from the case. These reports should also provide a nursing perspective including details on patient follow-up and interdisciplinary collaboration.
The limitations of this research study are that it did not have a systematic literature review process, which requires extending the searches conducted in Medline to the rest of the main national and international databases. It would also be necessary to extend the review and registration of the standards to authors in other journals included in SJR categories other than those consulted, and to examine the journals indexed with other bibliometric indicators of reference and impact.
When contrasting the CARE guidelines with the checklist for writing a clinical case by Tirado-Pedregosa et al.35 and the elements proposed by Siedlecki34 and the stages of the NP, there is a lack of adjustment in relation to the number and sequence of the basic elements necessary to comprehensively report a clinical case with a nursing perspective, which shows the importance of developing a CARE extension for these reports. To conclude, the intrinsic and structural methodological characteristics of the NP, together with the specificity of the CPs, imply poor adherence to CARE standards, as shown by the variability in the scientific literature of the clinical case reports consulted. It is therefore necessary to unify criteria to guide researchers, authors, reviewers, and editors of scientific journals and improve the rigour and quality of the published reports.
Among the implications for clinical practice, it should be noted that, at present, there is no specific guideline for reporting nursing case reports adjusted to the specific verification elements of the NP. These regulatory shortcomings could be addressed by a specific extension of the CARE standards to better reflect the nursing perspective, and which is adapted to the methodological characteristics of the NP.
FundingNo specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research study.
Conflict of interestsThe authors have no conflict of interests to declare.