Examine the construct validity of the Barthel Index in adult inpatient units.
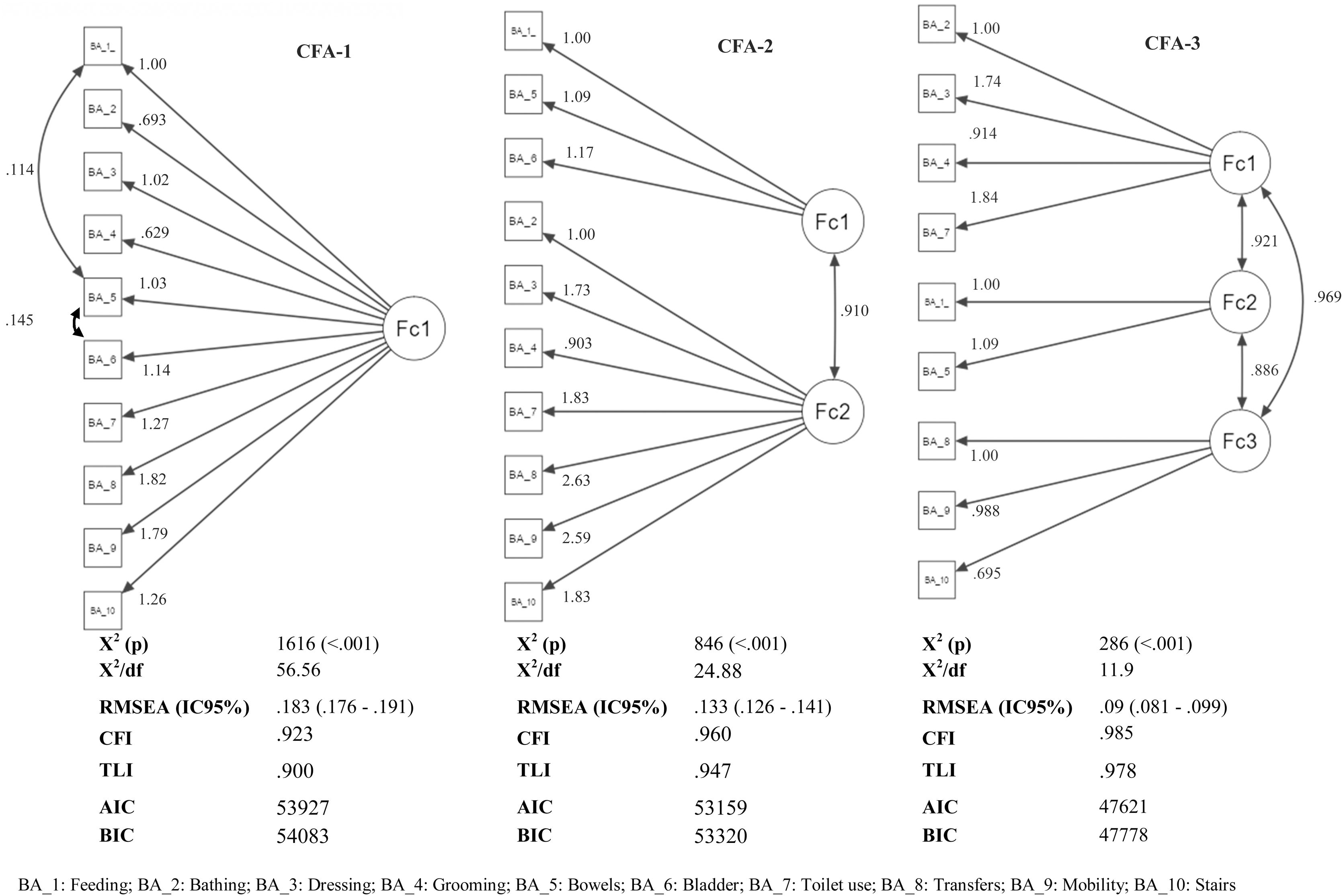
MethodA secondary analysis was performed on a sample of 1342 adult patients admitted to inpatient units. A confirmatory factor analysis of the Barthel Index did not confirm its unidimensional structure (CFA-1). Therefore, two methods were explored to find a solution with a better fit. The sequence of the classical exploratory and confirmatory factor analysis methods was carried out (CFA-2). In contrast, a Gaussian graphical model and confirmatory factor analysis (CFA-3) were performed. Three models were compared on the basis of several goodness-of-fit indicators.
ResultsCFA-1 results (χ2 = 161,616; P < .001; RMSEA = .183) indicated a poor fit between the model and the data. Exploratory factor analysis provided a model with two dimensions that explained 86% of the variance and improved the goodness-of-fit in CFA-2 (χ2 = 846; P < .001; RMSEA = .133). The Gaussian graphical model, by removing the item ‘Bladder’, offered a solution with three dimensions that improved the goodness-of-fit compared to the previous models (χ2 = 492; P < .001; RMSEA = .09).
ConclusionThe Barthel Index is not a unidimensional measure of functional capacity when applied to adult inpatient units. The best-fitting model has a three-dimensional structure (Hygiene; Feeding and disposal; Mobility) that relates to the domains of care needs.
Examinar la validez de constructo del Índice de Barthel en unidades de hospitalización de adultos.
MétodosSe realizó un análisis secundario en una muestra de 1.342 pacientes adultos ingresados en unidades de hospitalización. El análisis factorial confirmatorio del Índice de Barthel no confirma su estructura unidimensional (CFA-1). Se exploraron dos métodos para encontrar una solución con un mejor ajuste. Se realizó la secuencia de los métodos clásicos de análisis factorial exploratorio y confirmatorio (CFA-2). Se realizó un modelo gráfico gaussiano y un análisis factorial confirmatorio (CFA-3). Se compararon tres modelos sobre una base de varios indicadores de bondad de ajuste.
ResultadosLos resultados del CFA-1 (χ2 = 161,616; P < .001; RMSEA = 0.183) indicaron un mal ajuste entre el modelo y los datos obtenidos. El análisis factorial exploratorio proporcionó un modelo con dos dimensiones que explicaba el 86% de la varianza y mejoró el indicador de bondad de ajuste en CFA-2 (χ2 = 846; P < .001; RMSEA = 0.133). El modelo gráfico gaussiano ofreció una solución con tres dimensiones que mejoró la bondad de ajuste con respecto a los modelos anteriores al eliminar el ítem continencia vesical, (χ2 = 493; P < .001; RMSEA = 0.09).
ConclusionesEl Índice de Barthel no es una medida unidimensional de la capacidad funcional cuando se aplica en unidades de hospitalización de adultos. El modelo que mejor se ajusta tiene una estructura tridimensional (Higiene; Alimentación y eliminación; Movilidad) que se relaciona con los dominios de los cuidados básicos.
The assessment of functional capacity provides information on the level of dependency of people. One of the most widely used instruments for its assessment is the Barthel Index, being a unidimensional measure that assesses functional capacity.
What it provides:This study provides results on the structure of the Barthel Index presenting a three-dimensional model that provides more accurate information on the care needs of people admitted to inpatient units.
Functional capacity assessment provides essential information on the dependency level of individuals and has a quantitative and qualitative impact on the intensity of care required by patients in inpatient units.1
One of the most widely used and accepted tools for assessing functional capacity is the Barthel Index (BI). Initially, the BI was developed to assess the evolution of patients with musculoskeletal and neuromuscular processes in rehabilitation services,2 but its power to detect situations of functional dependence has led to its use being generalised to different types of users and levels of care.
The BI is a unidimensional measure that assesses functional ability through the performance of 10 basic activities of daily living, with scores ranging from 0 (totally dependent) to 100 (totally independent) points2 (see supplementary material 1). Its validity and reliability in people over 65 years of age has been tested in different care settings.1 However, this limits its validity when applied to the general population in inpatient units, and no studies carried out in Spain were retrieved. Moreover, some studies suggest that the number of items and the unidimensional structure3 of the BI should be revised as it may vary according to the type of patient. Thus, the main objective of this study was to examine the construct validity of BI in adult inpatient units.
MethodsA secondary analysis was conducted on a sample of 1342 patients admitted to adult inpatient units between June and December 2020. We used anonymised data extracted from the electronic health record from one of the hospitals participating in the Nursing Assessment Project (VALENF for its acronym in Spanish). The general objective of this project was to design and validate an instrument that integrates the assessment of functional capacity, the risk of falls, and the risk of pressure ulcers. This project was approved by the Ethics and Research Committee of the Centre (Ref: VALENF. 12/01/2021).4
The VALENF Project database includes a large number of variables related to nursing assessment. Specifically, this study included the following variables: grouped age (<85; 65–84; 35–64; 18–35), sex (male; female), inpatient unit, type of process (medical; surgical), type of admission (scheduled; emergency), coronavirus disease 2019 (COVID-19) (positive; negative) and the overall score and the score of the BI items performed during the nursing assessment on admission.
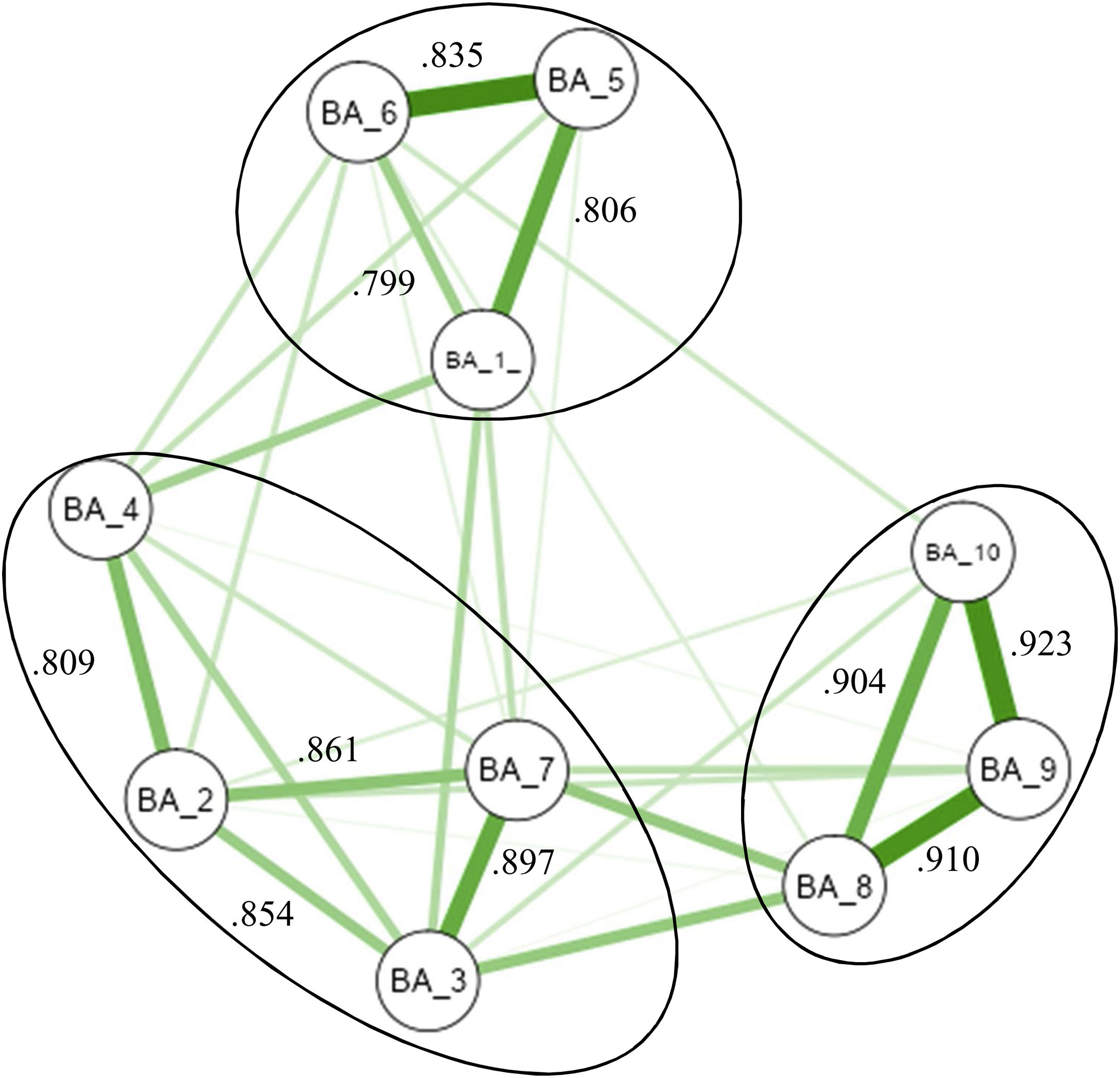
The descriptive analysis of the sample was performed according to the nature of the variables. A bivariate analysis of the BI score was also performed using the Mann-Whitney U test (two groups) or Kruskal-Wallis (three groups). The construct validity of the BI was first studied using Confirmatory Factor Analysis (CFA), using the maximum likelihood estimation technique and respecting its original structure (CFA-1).3 Based on the results, two methods were explored to determine the factor structure of the BI with a better model-data fit. On one hand, a 2-factor solution was obtained by performing an Exploratory Factor Analysis (EFA) using the minimal residuals extraction procedure and Oblimin rotation5 (Kaiser-Meyer-Olkin = 0.954; Barlet's χ2 = 20376; df = 45; P < .001); then, a second CFA was run on this model (CFA-2). On the other hand, partial correlations were analysed through a Gaussian graphical model using the extended Bayesian information criterion as a fitting parameter.6 Based on these results, a third CFA with a three-factor solution was performed (CFA-3).
The absolute goodness-of-fit7 indicators used were chi-square (χ2, small scores indicate good fit), ratio of χ2 to degrees of freedom (χ2/df < 5 indicates an adequate fit), and Root Mean Square Error of Approximation (RMSEA ≤ 0.1 indicates an adequate fit). The incremental goodness-of-fit indicators were Comparative Fit Index (CFI ≥ 90 indicates good fit) and Tucker-Lewis Index (TLI ≥ 0.90 indicates good fit). The parsimony fit indicators used to compare the three CFAs were the Akaike Information Criteria (AIC) and Bayesian Information Criteria (BIC) (lower values indicate better fit). In addition, an individual item extraction was performed to explore possible improvements in goodness of fit and a post-hoc analysis of the models’ performance through the correlation matrix of the residuals, to detect items that could be removed or grouped into new dimensions.8 The analysis was performed using JAMOVI 1.6.23 software.
ResultsDescription of the sampleThe majority of the sample, 63.5% (n = 852), were aged > 65 years, 51.9% (n = 695) were male, and 17.7% (n = 237) were COVID-19 positive patients. The traumatology unit accounted for 51.3% (n = 689) of the cases. Further, 71.5% (n = 959) of the sample were medical in origin, and 87.7% (n = 1177) were emergency admissions. The mean BI score was 76.1 (±35) points, with significant differences according to age, sex, nursing unit, type of process, type of admission, and being a COVID-19 patient (P < .001).
Construct validityThe CFA-1 results indicated a good fit of the original BI structure against the model with zero variance but did not confirm an adequate model-data fit (Fig. 1). In the post-hoc analysis, a correlation of residuals > 0.1 was observed between the items ‘Feeding’ and ‘Bowels’ (0.114), as well as between the items ‘Bowels’ and ‘Bladder’ (0.145).
Next, the EFA explained 86% of the cumulative variance with a two-factor solution. The first factor grouped the items Feeding, Bowels, and Bladder (59.1% of the variance), and the second factor grouped the remaining items (29.9% of the variance). Fig. 1 shows how the CFA-2 goodness-of-fit indicators improved slightly with respect to the CFA-1 model, although there continued to be no good model-data fit. In the post-hoc analysis, no relevant correlations were observed in the residuals, and individual item extraction did not improve the goodness of fit.
Finally, the analysis of partial correlations provided three groups of items in the Gaussian graphical model (Fig. 2). The first grouped the items Bathing, Dressing, Grooming, and Toilet use, the second grouped the items Feeding, Bowels, and Bladder, and the third grouped the items Transfers, Mobility and Stairs. The goodness of fit improved with respect to the CFA-1 and CFA-2 models, although there continued to be no good model-data fit (χ2 = 491; P < .001; df/χ2 = 15.3, RMSEA = 0.103; CI95% = 0.095–0.112; CFI = 0.978; TLI = 0.968; AIC = 52,803; BIC = 52,975). However, the removal of the item ‘Bladder’ improved the values of all indicators, resulting in a model that fit with the sample data (χ2 = 286; P < .001; df/χ2 = 11.9, RMSEA = 0.09; 95%CI = 0.081–0.099; AIC = 47,621; BIC = 47,778).
DiscussionOur results indicate that BI is not a unidimensional measure of functional capacity in inpatient units, contrary to what has been suggested by previous studies.9 In our case, the χ2 results invalidated the unidimensional model (CFA-1); however, the sample size could mask a valid model. Furthermore, the RMSEA values indicated that there was not a good model-data fit; the AIC and BIC results improved in the other models. In addition, three items showed residual correlations, justifying a revision of the BI structure. In such cases, researchers often look for solutions with fewer items that maintain a good fit, but the validity of the measurement may be affected if items are reduced, leading to an attenuation paradox.8 BI structures with fewer items have already been explored but to avoid this potential bias and maintain their clinical utility, we decided to use other procedures.
Thus, Lake et al.4 concluded that the dimensions of BI may vary depending on the type of patient. Specifically, these authors obtained a two-dimensional structure of the BI, identical to our CFA-2 (bodily functions and mobility) model, although there was no good model-data fit in our case. However, EFA and CFA were run on the same sample, which is not a routine procedure, but it allows the control of measurement errors that are beyond the scope of EFA.
Furthermore, the Gaussian graphical model offered a new three-dimensional solution that exhibited the best indicators (CFA-3), although the Bladder item was removed in order to find a good model-data fit. Thus, the first-dimension grouped items related to Hygiene (bathing, dressing, grooming, toilet use), the second-dimension grouped items related to Feeding and Elimination functions (Feeding and Bowels), and the third-dimension items related to Mobility (Transfer, Mobility, Stairs). According to Mueller et al.,1 the unidimensional structure of the BI and the aggregate score limit its usefulness in clinical practice, masking particular aspects of functional ability that influence the intensity of care.
Further studies are needed to confirm this new structure of the BI and to use other methodological approaches, such as structural equation models or item-response theory. Regardless, we identified a valid three-dimensional model of BI (Hygiene; Feeding and disposal; Mobility) that recognises domains related to care needs10 and may provide more accurate information on patients’ functional capacity for better decision making in inpatient units.
Conflict of interestAuthors have no conflicts of interest to disclose.
The manuscript has been read and approved by all authors.
FundingThis work has been funded by the Universitat Jaume I, [grant number UJI-A2020-08].