To identify the prevalence of pre-pregnancy overweight/obesity in pregnant women and its relationship with socio-demographic factors and to describe the maternal and perinatal outcomes in a Barcelona hospital (Spain).
MethodA descriptive cross-association study, with retrospective data collection, was performed Barcelona Hospital. The data of 5447 pregnant women who delivered at >=23 weeks of gestation were included. Body Mass Index (BMI) data were categorised into World Health Organization classifications. p values <.05 (two-tailed) were considered significant. Logistic regression models were performed.
ResultsThe prevalence of pre-pregnancy obesity was 8.4% and 18.9% for overweight. Gestational diabetes was more frequent in pre-pregnancy overweight/obesity (OR 1.92: 95% CI 1.54–2.40 and OR 3.34: 95% CI 2.57–4.33), as were preeclampsia (OR 2.08: 95% CI 1.55–2.79 and OR 3.35: 95% CI 2.38–4.71), induction of labour (OR 1.19: 95% CI 1.02–1.38 and OR 1.94: 95% CI 1.57–2.10), caesarean section (OR 1.41: 95% CI 1.21–1.65 and OR 2.68: 95% CI 2.18–3.29), prematurity (OR 1.28: 95% CI 1–1.65 and OR 1.79: 95% CI 1.32–2.44) and macrosomia (OR 1.87: 95% CI 1.43–2.46 and OR 2.03: 95% CI 1.40–2.93).
ConclusionsOne in four pregnant women had pre-pregnancy overweight or obesity. This study shows the relationship between pre-pregnancy overweight or obesity with adverse maternal and perinatal outcomes.
Identificar la prevalencia de obesidad o sobrepeso preconcepcional y su relación con los factores sociodemográficos, y describir los resultados maternos y perinatales en un hospital de Barcelona (España).
MétodoEstudio descriptivo de asociación cruzada, con recogida de datos retrospectiva en un hospital de la ciudad de Barcelona (España). Se analizó la información de 5.447 embarazadas con parto≥23 semanas de gestación. El índice de masa corporal fue categorizado según la clasificación de la Organización Mundial de la Salud. Se realizó un análisis estadístico bilateral asumiendo un valor α igual a 0,05. Se realizaron modelos de regresión logística.
ResultadosLa prevalencia de obesidad preconcepcional fue del 8,4% y la del sobrepeso, del 18,9%. Las gestantes con obesidad o sobrepeso preconcepcional presentaron con mayor frecuencia diabetes gestacional (OR 1,92; IC 95% 1,54 a 2,40 y OR 3,34; IC 95% 2,57 a 4,33), preeclampsia (OR 2,08; IC 95% 1,55 a 2,79 y OR 3,35; IC 95% 2,38 a 4,71), inducción del parto (OR 1,19; IC 95% 1,02 a 1,38 y OR 1,94; IC 95% 1,57 a 2,10), cesárea (OR 1,41; IC 95% 1,21 a 1,65 y OR 2,68; IC 95% 2,18 a 3,29), prematuridad (OR 1,28; IC 95% 1 a 1,65 y OR 1,79; IC 95% 1,32 a 2,44) y macrosomía (OR 1,87; IC 95% 1,43 a 2,46 y OR 2,03; IC 95% 1,40 a 2,93).
ConclusionesUna de cada 4 gestantes presentó sobrepeso u obesidad preconcepcional. Se observó relación entre el sobrepeso u obesidad preconcepcional con la presentación de resultados maternos y perinatales adversos.
Obesity is an increasingly prevalent public health problem in our society. Preconception obesity is a risk factor for complications during pregnancy and delivery, as well as for the appearance of perinatal complications.
What this contribute?The prevalence of obesity and preconception overweight observed in a Barcelona hospital was lower than in other Spanish cities. This study points out the relationship between some sociodemographic factors and pregnancy in women with an inadequate Body Mass Index. Preconception overweight and obesity were associated with adverse maternal and perinatal outcomes.
Obesity is an increasingly more prevalent health problem in our society.1 Women who begin pregnancy with a Body Mass Index (BMI)>25kg/m2 are at higher risk of maternal adverse outcomes.2 In Europe, the prevalence of pre-pregnancy overweight and obesity is between 26.8% and 54%.3 However, there are scarce data concerning pre-pregnancy obesity women who lives in the Mediterranean region.4
At the same time, socio-demographic and obstetric factors seem to be related to women beginning pregnancy with overweight and obesity.5
The socio-demographic characteristics, as well as the diet and lifestyles of pregnant women of southern Europe, could differ from the women of central-northern Europe, and therefore, it could influence perinatal outcomes.
The aims of this study were to identify the prevalence of pre-pregnancy overweight/obesity in pregnant women and its relation with socio-demographic factors and to describe the maternal and perinatal outcomes in a hospital of Barcelona city (Spain).
MethodStudy design and setting.We conducted a descriptive cross association study, with retrospective data collection, of all pregnant women who gave birth in a high maternity complexity hospital in “Clinic Hospital of Barcelona” from January 1, 2015 to December 31, 2016 in Barcelona (Spain).
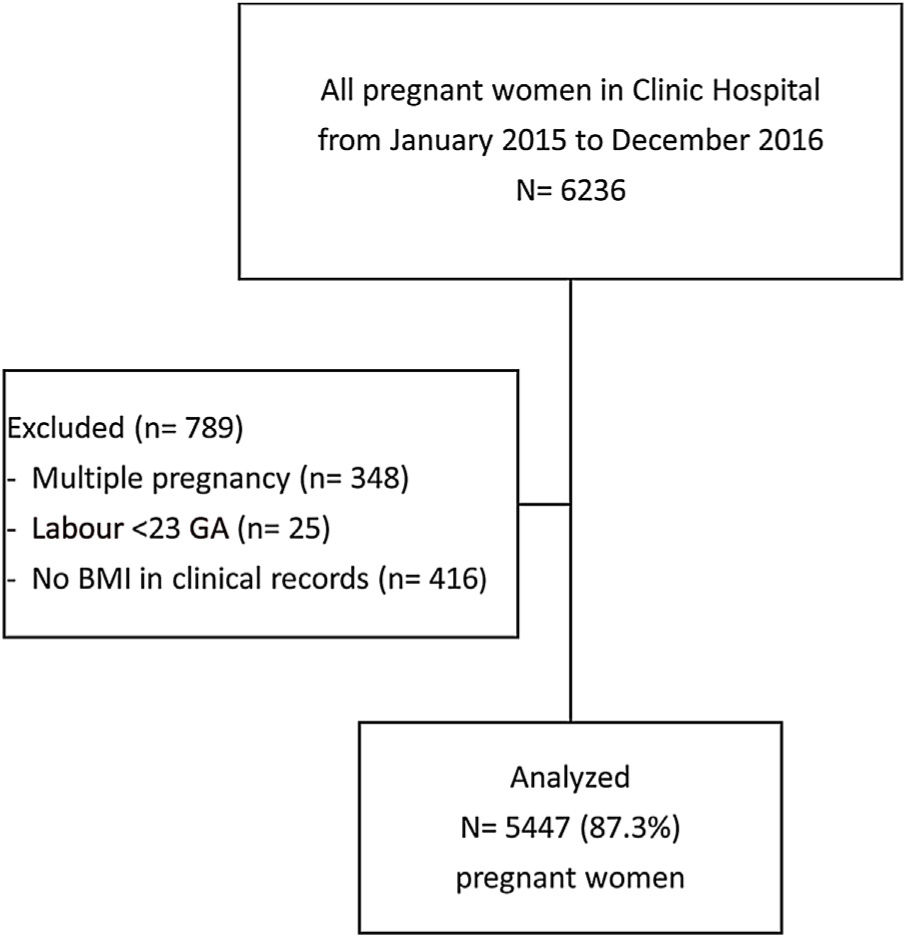
Study populationThe inclusion criteria were women with delivery after 23 weeks of gestational age (GA). Multiple pregnancies and women in whom the pre-pregnancy BMI was not available in the electronic medical record were excluded from the study.
Study variablesThe following variables were collected: woman's age in complete years, pre-pregnancy BMI in kg/m2 based on the weight reported by the woman herself6 and classified into the following categories: underweight (BMI<18.5kg/m2); normal weight (BMI between 18.5 and 24.9kg/m2); overweight (BMI between 25 and 29.9kg/m2) and obesity (BMI≥30kg/m2),7 country of origin (Spanish, foreign), educational level (primary, secondary, higher), employed (yes, no), previous births (yes, no), gestational diabetes was defined as women with diabetes onset during pregnancy,8 preeclampsia was defined as women with hypertension onset during pregnancy,9 type of onset of labour (induction, spontaneous, elective caesarean section), type of delivery (spontaneous vaginal birth, instrumental, caesarean section). The variable of GA of the newborn was categorised as premature (<37 GA), term (37–41.6 GA) and post-term (≥42 GA).10 The weight of the neonate was classified as underweight (<2500g), normal weight (2500–3999g) and macrosome (≥4000g).
Data collectionThe data was obtained, retrospectively, from the hospital's computerised medical record system. In February 2017, the hospital information area carried out an automated and anonymised extraction of all the records of women with labour assisted during the two years of study, and the data was downloaded in an “Excel” spreadsheet to which only the research team had access.
Statistical analysisDescriptive data are presented as number and percentage, and the mean and standard deviation (SD).
Bivariate analysis was performed between the socio-demographic variables and the pre-pregnancy BMI. For the comparison of the categorical variables, Chi-Square test was used. To compare quantitative variables, variance analysis (ANOVA) was performed.
Adjusted multinomial logistic regression was performed with the objective of identifying the socio-demographic and obstetric factors related to the pre-pregnancy BMI, where BMI was assumed a nominal variable taking the normal weight category as the reference group of women. Logistic regression models were performed to evaluate the perinatal and maternal results related to pre-pregnancy BMI of pregnant women. Adjusted Odds Ratio (OR) and 95% confidence intervals (95% CI) were calculated for each model. All statistical tests were bilateral and p values <0.05 were considered significant Descriptive analyses were carried out with the statistical package IBM SPSS version 25®, and multivariate analyses were performed with the statistical package SAS version 9.4® (SAS Institute, Cary, NC, USA).
Ethical considerationsAuthorisation was obtained from the Ethics and Clinical Research Committee of the Clinic Hospital of Barcelona, Code: HCB/2017/0309. At all times the anonymity and confidentiality of the data were preserved in accordance with the Spanish Organic Law 3/2018, of December 5, about Protection of Personal Data and guarantee of digital rights. The informed consent was exempt because the data were obtained from medical records.
ResultsA sample of 6236 women who were assisted at delivery was obtained. Of these, 348 women with multiple births, 25 with delivery before 23 GA, and 416 women in whom the pre-pregnancy BMI did not appear in the computerised medical record were excluded. Finally, the data of 5447 pregnant women (87.3%) were analysed (Fig. 1).
The mean pre-pregnancy BMI was 23.4kg/m2 (95% CI 23.3–23.5). The prevalence of women with pre-pregnancy overweight was 18.9% (n=1032, 95% CI 17.3–20.2), and the prevalence of women with pre-pregnancy obesity was 8.4% (n=458, 95% CI 7.6–9.7). Thus, the percentage of the studied women who presented pre-pregnancy overweight or obesity was 27.3% (n=1490, 95% CI 26.2–28.5).
Table 1 shows the socio-demographic and obstetric characteristics and their relationship with the pre-pregnancy weight status of the pregnant women included in the study. Table 2 shows the results of multinomial logistic regression between the socio-demographic and obstetric characteristics and pre-pregnancy BMI.
Socio-demographic and obstetric characteristics and relationship with the pre-pregnancy weight status of pregnant women.
| Total | Underweight | Normal weight | Overweight | Obesity | p value | |
|---|---|---|---|---|---|---|
| n=5447 | n (%) | n (%) | n (%) | n (%) | ||
| n=278 (5.1) | n=3679 (67.5) | n=1032 (18.9) | n=458 (8.4) | |||
| Age: years | ||||||
| Means (SD) | 32.9 (5.4) | 31.5 (5.9) | 33.1 (5.2) | 32.7 (5.6) | 32.3 (5.8) | <0.001* |
| Country of origin | n=5447 | n=278 | n=3679 | n=1032 | n=458 | |
| Spanish | 3527 (64.8) | 186 (5.3) | 2467 (69.9) | 589 (16.7) | 285 (8.1) | |
| Foreign | 1920 (35.2) | 92 (4.8) | 1212 (63.1) | 443 (23.1) | 173 (9) | <0.001** |
| Educational level | n=5218 | n=265 | n=3554 | n=983 | n=416 | |
| Primary | 655 (12.6) | 29 (4.4) | 336 (51.3) | 192 (29.3) | 98 (15) | |
| Secondary | 1567 (30) | 66 (4.2) | 950 (60.6) | 374 (23.9) | 177 (11.3) | |
| Higher | 2996 (57.4) | 170 (5.7) | 2268 (75.7) | 417 (13.9) | 141 (4.7) | <0.001** |
| Employed | n=5282 | n=269 | n=3589 | n=1000 | n=424 | |
| Yes | 3862 (73.1) | 189 (4.9) | 2758 (71.4) | 665 (17.2) | 250 (6.5) | <0.001** |
| No | 1420 (26.9) | 80 (5.6) | 831 (58.5) | 335 (23.6) | 174 (12.3) | |
| Previous births | n=5447 | n=278 | n=3679 | n=1032 | n=458 | |
| Yes | 1766 (32.4) | 78 (4.4) | 1079 (61.1) | 398 (22.5) | 211 (11.9) | <0.001** |
| No | 3681 (67.6) | 200 (5.4) | 2600 (70.6) | 634 (17.2) | 247 (6.7) | |
n=number; SD=standard deviation.
Results of multinomial logistic regression between the socio-demographic and obstetric characteristics and pre-pregnancy BMI.
| Underweight | Overweight | Obesity | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 0.95 (0.92–0.97) | 1.02 (1.00–1.03) | 1.01 (0.99–1.03) |
| Country of origin | |||
| Spanish | Reference | Reference | Reference |
| Foreign | 0.91 (0.69–1.21) | 1.23 (1.05–1.44) | 0.84 (0.67–1.05) |
| Educational level | |||
| Primary | Reference | Reference | Reference |
| Secondary | 0.90 (0.57–1.44) | 0.75 (0.61–0.94) | 0.73 (0.55–0.97) |
| Higher | 1.25 (0.79–1.96) | 0.37 (0.29–0.45) | 0.26 (0.19–0.36) |
| Employed | |||
| Yes | 0.78 (0.57–1.07) | 0.81 (0.68–0.96) | 0.63 (0.49–0.79) |
| No | Reference | Reference | Reference |
| Previous births | |||
| Yes | 1.06 (0.80–1.41) | 1.36 (1.16–1.58) | 1.86 (1.50–2.31) |
| No | Reference | Reference | Reference |
OR=Odds Ratio adjusted; 95% CI: 95% confidence interval.
It was found that there was relationship between maternal age, country of origin, educational level, employment status, and having previous births, with women's pre-pregnancy BMI.
Pregnant women with a lower mean age were more frequently underweight. Foreign women had more frequently overweight compared to women of Spanish origin. Women with a secondary or higher education presented less frequently pre-pregnancy overweight and obese than pregnant women with a primary education. Overweight or obese were also less frequent among employed women. Finally, women who had had previous births more frequently started pregnancy with pre-pregnancy overweight or obesity than nulliparous women (Table 2).
Regarding the relationship between BMI with maternal complications, gestational diabetes and preeclampsia during pregnancy were more frequent among women with pre-pregnancy overweight and obesity (Table 3).
Relationship between the pre-pregnancy weight status of pregnant women and the prevalence of gestational diabetes and preeclampsia.
| Gestational diabetes | p value | OR (95% CI) | |||
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Total | 5447 | 501 (9.2) | 4946 (90.8) | ||
| Underweight | 278 (5.1) | 15 (5.4) | 263 (94.6) | 0.75 (0.44–1.28) | |
| Normal weight | 3679 (67.5) | 261 (7.1) | 3418 (92.9) | Reference | |
| Overweight | 1032 (18.9) | 132 (12.8) | 900 (87.2) | 1.92 (1.54–2.40) | |
| Obesity | 458 (8.4) | 93 (20.3) | 365 (79.7) | <0.001* | 3.34 (2.7–4.33) |
| Preeclampsia | |||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Total | 5447 | 264 (4.8) | 5183 (95.2) | ||
| Underweight | 278 (5.1) | 11 (4) | 267 (96) | 1.13 (0.60–2.11) | |
| Normal weight | 3679 (67.5) | 130 (3.5) | 3549 (96.5) | Reference | |
| Overweight | 1032 (18.9) | 73 (7.1) | 959 (92.9) | 2.08 (1.55–2.79) | |
| Obesity | 458 (8.4) | 50 (10.9) | 408 (89.1) | <0.001* | 3.35 (2.38–4.71) |
n=number.
Regarding labour outcomes, it was observed that women with pre-pregnancy overweight and obesity started labour, more frequently, by induction or by elective caesarean section (Table 4).
Relationship between pre-pregnancy weight status of pregnant women and labour outcomes.
| Total | Type of onset of labour | |||||
|---|---|---|---|---|---|---|
| n (%) | Spontaneous | Induction | Elective caesarean | |||
| n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | ||
| Total | 5447 | 3379 (62) | 1612 (29.6) | 456 (8.4) | ||
| Underweight | 278 (5.1) | 191 (68.7) | 67 (24.1) | 0.79 (0.60–1.06) | 20 (7.2) | 0.96 (0.60–1.55) |
| Normal weight | 3679 (67.5) | 2372 (64.5) | 1049 (28.5) | Reference | 258 (7) | Reference |
| Overweight | 1032 (18.9) | 612 (59.3) | 321 (31.1) | 1.19 (1.02–1.38) | 99 (9.6) | 1.49 (1.16–1.91) |
| Obesity | 458 (8.4) | 204 (44.5) | 175 (38.2) | 1.94 (1.57–2.10) | 79 (17.2) | 3.56 (2.67–4.76) |
| n (%) | Type of delivery | |||||
|---|---|---|---|---|---|---|
| Spontaneous vaginal birth | Instrumental | Caesarean section | ||||
| n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | ||
| Total | 5447 | 3610 (66.3) | 451 (8.3) | 1386 (25.4) | ||
| Underweight | 278 (5.1) | 203 (73) | 25 (9) | 0.99 (0.64–1.52) | 50 (18) | 0.75 (0.54–1.03) |
| Normal weight | 3679 (67.5) | 2530 (68.8) | 316 (8.6) | Reference | 833 (22.6) | Reference |
| Overweight | 1032 (18.9) | 649 (62.9) | 81 (7.8) | 1 (0.77–1.29) | 302 (29.3) | 1.41 (1.21–1.65) |
| Obesity | 458 (8.4) | 228 (49.8) | 29 (6.3) | 1.02 (0.68–1.52) | 201 (43.9) | 2.68 (2.18–3.29) |
n=number; OR=Odds Ratio; 95% CI: confidence interval.
Concerning the perinatal outcomes, the prevalence of premature new-borns was higher in women with pre-pregnancy overweight and obesity. Concerning neonate weight, the new-borns of women with pre-pregnancy overweight more frequently presented macrosomia, while in women with pre-pregnancy obesity neonates were more frequently underweight or presented macrosomia (Table 5).
Relationship between pre-pregnancy weight status of pregnant women and perinatal outcomes.
| n (%) | Term | Premature | Post-term | |||
|---|---|---|---|---|---|---|
| n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | ||
| Total | 5447 | 4890 (89.8) | 419 (7.7) | 138 (2.5) | ||
| Underweight | 278 (5.1) | 250 (89.9) | 17 (6.1) | 0.88 (0.53–1.47) | 11 (4) | 1.45 (0.77–2.73) |
| Normal weight | 3679 (67.5) | 3322 (90.3) | 256 (7) | Reference | 101 (2.7) | Reference |
| Overweight | 1032 (18.9) | 920 (89.1) | 91 (8.8) | 1.28 (1–1.65) | 21 (2) | 0.75 (0.47–1.21) |
| Obesity | 458 (8.4) | 398 (86.9) | 55 (12) | 1.79 (1.32–2.44) | 5 (1.1) | 0.41 (0.17–1.02) |
| n (%) | Neonatal weight | |||||
|---|---|---|---|---|---|---|
| Normal weight | Underweight | Macrosoma | ||||
| n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | ||
| Total | 5447 | 4675 (85.8) | 477 (8.8) | 295 (5.4) | ||
| Underweight | 278 (5.1) | 251 (90.3) | 21 (7.6) | 0.87 (0.55–1.38) | 6 (2.2) | 0.46 (0.20–1.05) |
| Normal weight | 3679 (67.5) | 3204 (87.1) | 308 (8.4) | Reference | 167 (4.5) | Reference |
| Overweight | 1032 (18.9) | 860 (83.3) | 88 (8.5) | 1.06 (0.83–1.36) | 84 (8.1) | 1.87 (1.43–2.46) |
| Obesity | 458 (8.4) | 360 (78.6) | 60 (13.1) | 1.73 (1.29–2.33) | 38 (8.3) | 2.03 (1.40–2.93) |
n=number; OR=Odds Ratio; 95% CI: 95% confidence interval.
This exploratory study shows that the prevalence of women with pre-pregnancy overweight was 18.9% and with pre-pregnancy obesity was 8.4%, that is, that 27.3% of the women in this study had an inadequate BMI to start the pregnancy.
In concordance with previous studies, was observed that foreign women, unemployed women, or with lower educational level had more odds to present pre-pregnancy overweight and obesity. Moreover, perinatal complications were more frequent in women with a BMI>25kg/m2.11
Our prevalence of pre-pregnancy overweight of 18.9% and 8.4% of pre-pregnancy obesity were lower than the prevalence reported in other Spanish studies.12–14 Likewise, our prevalence of pre-pregnancy obesity was 8.4%, which was lower than the 9.6% of 301 women studied in Aragón,12 the 17.1% of 6558 women in Canary Islands13 and the 13.3% of 16609 women in Basque Country.14
Regarding the prevalence of overweight in other European countries, the value in the present study was like that reported in Croatia (19%).3 However, these values are much lower than those reported in Northern Ireland (29.8%).3 Prevalence of 8.4% of pre-pregnancy obesity in our study was higher than in Croatia (7.8%) but lower than the United Kingdom (20.4–25.6%).3
Like other studies, socio-demographic and obstetric factors were related with the pre-pregnancy BMI of women.5,15 In Spain, the BMI of adult Spanish women generally increases with age.12,13 In this study, foreign women presented more frequently pre-pregnancy overweight compared to Spanish women.16 In addition, women with a lower education level, or who were unemployed or who had had previous births were more frequently overweight and obese pre-pregnancy.5,15
Regarding data on pregnancy complications, gestational diabetes and preeclampsia were more frequent among women with pre-pregnancy overweight or obesity as in the exploratory study of Yang17 and in the cohort study of Schummers.18
Regarding labour outcomes, it was observed that the probability of induction increased with an increase in pre-pregnancy BMI, reaching an OR of 1.94 in women with pre-pregnancy obesity, like what has been described in previous studies.19,20
In this study, the percentage of women with pre-pregnancy obesity who underwent caesarean section (43.9%) was higher than that in a retrospective cohort study conducted in Canary Islands (18.7%),13 in a historical cohort study in Basque Country (25.7%)14 and with a descriptive study conducted in Castilla-La Mancha (34.9%).21
In line with the results of a meta-analysis by Dai et al., in 2018, maternal pre-pregnancy overweight and obesity in our study increased the probability of macrosomia in the newborn22; and the macrosomia increases the intrapartum complications and neonatal sequelae.23 As in the study by Kim et al., in 2017, prematurity being more frequent in women with pre-pregnancy overweight and obesity.24 The high rate of prematurity observed in our women could have increased the rates of underweight in our newborns, particularly in obese women who increased the probability of having an underweight neonate with an OR of 2.
Therefore, the identification of women with excess weight prior to conception should be implemented, and care should be adapted to the individual characteristics of women to improve maternal and perinatal outcomes. In addition, sensitive and proactive care must be provided, recognising and reporting possible risks to women, with counselling about diet and physical activity to facilitate an adequate weight before and during pregnancy seeking well-being in women.25 Thus, midwives and obstetricians should implement actions promoting health,26 these include diet and physical activity to achieve optimal health conditions during pregnancy.2,27
At present, there is not much data available about pre-pregnancy overweight and obesity and its relation to maternal outcomes in Spain. The study has been carried out in a hospital that attends high obstetric complexity in Barcelona, a city that has a diverse cultural population.
To our knowledge, this is the largest study to describe prevalence in a Mediterranean city in Spain providing pre-pregnancy weight status of 5447 women and allowing comparison with other studies at an international level.
However, this study did not get data of 416 women (12.7% of the sample) in whom the pre-pregnancy BMI was not available in the electronic clinical records. In addition, although gestational weight gain is an independent factor that can influence maternal and perinatal outcomes, we were not able to provide this gain, because this variable was not always available, in the electronic clinical records, so caused heterogeneity of the hospital registry at the end of pregnancy.28 Therefore, we suggest improving the quality of our hospital records, and obstetricians and midwives should report data on pregnant women's weight gain.29
Since this was a descriptive study, a relationship was observed between socio-demographic and obstetric factors and the presentation of a high BMI, so the causal inference is limited. Indeed, studies on the multifactorial origin of obesity involve a prospective cohort design that allows controlling for other variables that may influence the results such as lifestyle, culture, or religion.
This results provide knowledge about the prevalence of women with pre-pregnancy overweight and obesity in a high maternity complexity hospital of Barcelona (Spain), and that this prevalence was lower than majority of countries on Europe.
This study shows the relationship between some socio-demographic factors with begin the pregnancy with an inadequate BMI, and the relationship between pre-pregnancy overweight or obesity with adverse maternal and perinatal outcomes.
FundingThis study had been funded in partially by the “Nurse and Society Foundation” as part of the Nurse Research Projects Grants (PR-389/2019) Barcelona, Spain.
Elena González-Plaza received a research grant from “La Pedrera Foundation” (Nurse intensification grant) Barcelona, Spain.
We are grateful to Mrs. Mariuxi Burgos for reading this manuscript.