To describe the frequency and typology of the presenting symptom of women diagnosed of breast cancer in Spain and their socio-demographic profile.
MethodsDescriptive study nested in a population epidemiological study (MCC-SPAIN) in 10 Spanish provinces. Between 2008 and 2012, 836 histologically confirmed incident cases of breast cancer were recruited who reported some symptom prior to diagnosis in a direct computerized interview. For the comparison of 2 discrete variables, the Pearson Chi square test was used.
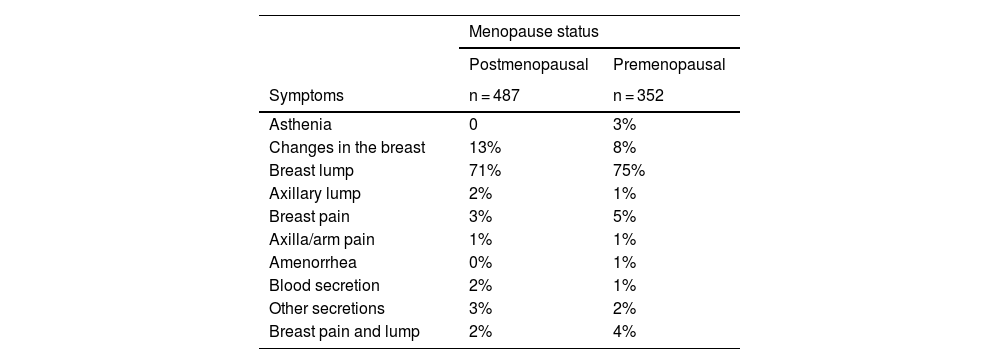
ResultsThe most frequent presenting symptom among women who reported at least one symptom was noticing a “lump in the breast” (73%), followed far behind by noticing “changes in the breast” (11%). Geographic heterogeneity was observed in the frequency of the presenting symptom, as well as with menopausal status. No association was observed between the type of presenting symptom and the rest of the sociodemographic variables explored, except for the educational level in which women with a higher educational level tended to proportionally report other symptoms different from the “lump in the breast” more frequently than less educated. Postmenopausal women reported noticing changes in the breast (13%) more frequently than premenopausal women (8%), although without reaching statistical significance (P = .056).
ConclusionsThe most frequent presenting symptom is “breast lump”, followed by “breast changes”. There could be sociodemographic heterogeneity in the type of presenting symptom to be taken into account by nurses in their socio-sanitary interventions.
Describir la frecuencia y tipología del síntoma de presentación de las mujeres diagnosticadas de cáncer de mama en España así como su perfil socio-demográfico así como.
MétodoEstudio descriptivo anidado en un estudio epidemiológico poblacional (MCC-SPAIN) en 10 provincias españolas. Entre 2008 y 2012 se reclutaron 836 casos incidentes histológicamente confirmados de cáncer de mama que refirieron algún síntoma previo al diagnóstico en entrevista directa informatizada. Para la comparación de 2 variables discretas se empleó el test de la Chi cuadrado de Pearson.
ResultadosEl síntoma de presentación más frecuente entre las mujeres que refirieron como mínimo un síntoma fue notarse un bulto en la mama (73%), seguido de lejos por notar cambios en la mama (11%). Se observó heterogeneidad geográfica en la frecuencia del síntoma de presentación, así como con estado menopáusico. No se observó asociación entre tipo de síntoma de presentación y el resto de variables sociodemográficas exploradas, salvo para nivel de estudios en que las mujeres con un nivel de estudios mayor tendieron a reportar proporcionalmente otros síntomas diferentes al nodo en la mama con mayor frecuencia que las mujeres con menos estudios. Las mujeres postmenopáusicas refirieron notar cambios en la mama (13%) con mayor frecuencia que las mujeres premenopáusicas (8%), aunque sin llegar a la significación estadística (P = ,056).
ConclusionesEl síntoma de presentación más frecuente es la aparición de un “bulto en la mama”, seguido por “cambios en la mama”. Podría existir heterogeneidad sociodemográfica del tipo de síntoma de presentación a tener en cuenta por las enfermeras en sus intervenciones socio-sanitarias.
Worldwide, breast cancer is the most common type, followed by lung and prostate cancer, and its rate of incidence in women is three times that of the rates of colorectal or lung cancer.1 The incidence of breast cancer varies widely around the world, and it is highest in the developed countries.1 Nevertheless, over and above reproductive factors, endocrine disruption and genetic predisposition, hardly any factors are known which lead to a relevant increase in the risk for breast cancer, so that early detection is important.2,3
Surviving breast cancer is directly proportional to its stage at the moment it is diagnosed.4 Breast cancer can initially be categorized as subclinical, with no associated symptoms although it can be detected by early diagnosis techniques.4 The importance of screening programmes can therefore be underlined. These programmes are gaining ground and are a priority in health programmes for women. A clinical phase follows, in which a series of symptoms may indicate the presence of breast cancer.5 It is very important for medical professionals to be attentive in this phase, and patients should also be motivated to request social and medical care.6 In both cases it is important to be aware of the warning symptoms of breast cancer. The most important sign is the presence of a “lump or swelling”, and in fact this is the only sign which is included as a potential sign or symptom for referral to specialized care from primary care in the protocols for the latter in the breast cancer detection process and programme of, for example, the Regional Government of Andalusia.6 Other less common symptoms may also be present, such as “changes in the breast” (nipple retraction or flattening, increased breast size, erosion, a nipple scab or itching), “axillary ganglia”, or “secretion through the nipple”.7 Although these symptoms do not automatically require referral for the specific study of breast cancer, their cause should be investigated.
Nurses play a fundamental role in the prevention of this disease, at the levels of primary, secondary and tertiary prevention.8 Nurses in primary care as well as those in specialized oncology departments should acquire the necessary knowledge about breast cancer risk factors, and they should also know how to recognise its most common signs and symptoms. The role of nurses in primary prevention stands out among their functions in the clinical process (such as in lifestyle advice and health promotion), as well as in secondary prevention (such as in screening programmes, where a relevant question is whether there have been any previous symptoms), in the diagnostic process (in women with a high or a low level of suspicion), during treatment, follow-up and in the palliative care phase when this is necessary.8 Likewise, as it is highly important to promote equal access to social and medical oncological care, it is also important to identify the sociodemographic characteristics which may be associated with the onset of breast cancer symptoms.
This work aims to describe the frequency and typology of the presenting symptom of breast cancer, as well as the sociodemographic profile of the women diagnosed with this disease in Spain.
MethodDesignA descriptive study nested within a population-based epidemiological study (MCC-SPAIN).
Study population and contextMCC-SPAIN is an epidemiological case-control multicase population-based study that was undertaken in 10 Spanish regions from 2008 to 2013.9–15 All of the cancer cases were recently diagnosed incidents that were histologically confirmed for breast, prostate, colorectal and stomach locations.15
Sample and inclusion and exclusion criteriaThe breast cancer cases were recruited in 18 hospitals in 10 Spanish regions. All of the participants had to have lived in the region for at least 6 months prior to recruitment, and they had to be able to complete the epidemiological questionnaire. The inclusion criteria for the breast cancer group were: diagnosis of breast cancer (C50, D05.1, D05.7), histologically confirmed cancer, aged from 20 to 85 years and having lived in the hospital’s catchment area (as defined by each participating hospital) for at least 6 months before selection. The exclusion criteria included: communication impediments (mentally disabled, speech problems), or a previous diagnosis of cancer in the location studied.
Data gatheringThe information about the presenting symptom and sociodemographic factors was obtained by a direct computerized interview with the patients. The questions about the presenting symptom included: When did you start to feel ill? and What was the first thing that you noticed then? The literal remarks about symptoms were reclassified into the following categories: “asthenia”, “changes in the breast”, “lump in the breast”, “lump in the axilla”, “pain in the breast”, “pain in the axilla”, “amenorrhea”, “secretion of blood”, “other secretions”, and “painful lump in the breast”. When more than one presenting symptom was mentioned, the least common one was assigned.
Variables and instrumentsThe following were codified as discrete qualitative variables: recruitment province (10 categories), age (23–51; 52–61; 62–66; 67–74; 75–85), educational level (less than primary, primary, secondary, university or higher), marital status (single, married, separated/divorced, widow), smoker (non-smoker, ex-smoker, smoker), exclusively a housewife (yes/no), social class according to their job (4 categories), number of live births (none, one, two, three or more), body mass index (MBI: less than 18.5; 18.5–24.9; 25–29.9; 30 or more), family history of breast cancer (no history of cancer in first degree family members, first degree family member with cancer, first degree family member with breast cancer).
Data analysisStandardized tests were used for the statistical analysis.16,17 Pearson’s Chi-squared test was used to compare 2 discrete variables, or alternatively Fisher’s exact test was used when more than 20% of the boxes had a number of cases less than or equal to five.16 The Student or ANOVA tests were used to analyse the relationship between quantitative variables and categorical variables with 2 levels, or categorical variables with more than 2 levels, respectively. The Kruskal-Wallis test was used to compare continual variables that did not follow a normal distribution and discrete variables with more than 2 categories.17 The level of statistical significance was set at 5%. All of the P are bilateral. Version 21 of SPSS for Windows was used for the statistical analysis.
Ethical considerationsThis study was undertaken according to Helsinki Declaration guidelines, and it was approved by the Ethics Committee of each recruiting centre. The patients were supplied with the contents of the information sheet, which was also explained to them, and all of the women involved in the study gave their informed consent.
ResultsOf the total number of 2448 eligible cases contacted, 1738 cases of breast cancer who completed the study questionnaire were recruited (a 71% response rate). After excluding 40 women without information about their symptoms, 761 with breast cancer that had been diagnosed without previous symptoms, 98 women who mentioned symptoms that commenced after the diagnosis and three cases with interviews of dubious quality, 836 women remained (48.2% of 1738) who had symptoms prior to diagnosis. They form the final sample used in this study.
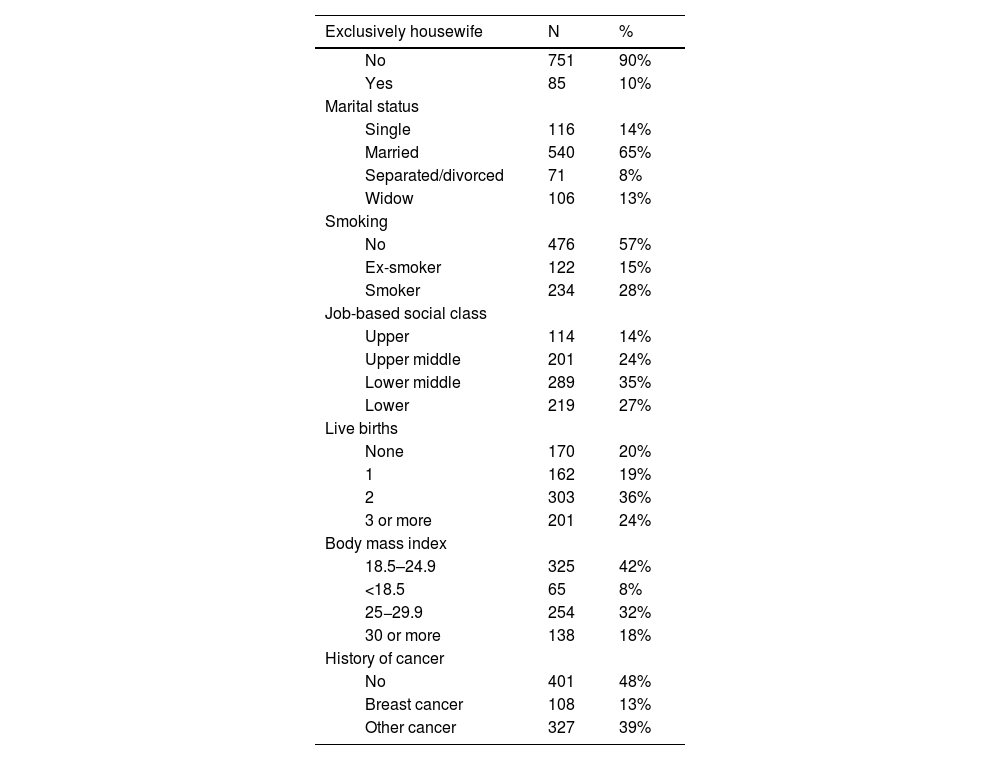
Table 1 shows the sociodemographic characteristics of the population that are not displayed in Tables 2 to 5. The majority of the women were married, middle or lower class, non-smokers, with two or more pregnancies to term, a normal body mass index and no history of cancer.
Sociodemographic characteristics of the participants.
| Exclusively housewife | N | % | |
|---|---|---|---|
| No | 751 | 90% | |
| Yes | 85 | 10% | |
| Marital status | |||
| Single | 116 | 14% | |
| Married | 540 | 65% | |
| Separated/divorced | 71 | 8% | |
| Widow | 106 | 13% | |
| Smoking | |||
| No | 476 | 57% | |
| Ex-smoker | 122 | 15% | |
| Smoker | 234 | 28% | |
| Job-based social class | |||
| Upper | 114 | 14% | |
| Upper middle | 201 | 24% | |
| Lower middle | 289 | 35% | |
| Lower | 219 | 27% | |
| Live births | |||
| None | 170 | 20% | |
| 1 | 162 | 19% | |
| 2 | 303 | 36% | |
| 3 or more | 201 | 24% | |
| Body mass index | |||
| 18.5–24.9 | 325 | 42% | |
| <18.5 | 65 | 8% | |
| 25−29.9 | 254 | 32% | |
| 30 or more | 138 | 18% | |
| History of cancer | |||
| No | 401 | 48% | |
| Breast cancer | 108 | 13% | |
| Other cancer | 327 | 39% | |
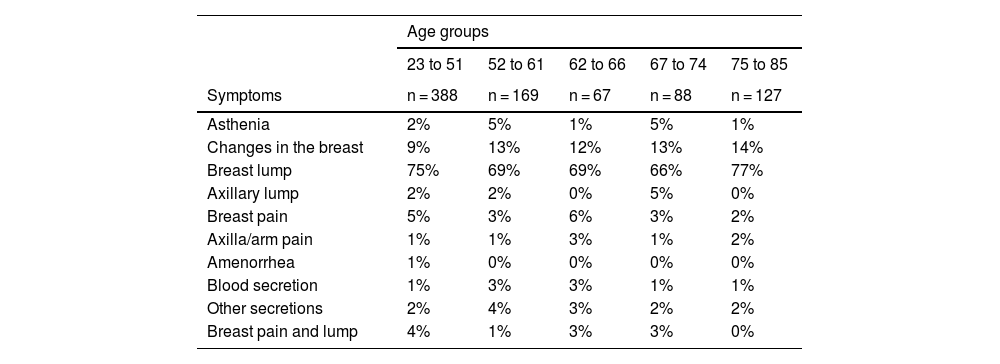
Association between presenting symptom of breast cancer and age.
| Age groups | |||||
|---|---|---|---|---|---|
| 23 to 51 | 52 to 61 | 62 to 66 | 67 to 74 | 75 to 85 | |
| Symptoms | n = 388 | n = 169 | n = 67 | n = 88 | n = 127 |
| Asthenia | 2% | 5% | 1% | 5% | 1% |
| Changes in the breast | 9% | 13% | 12% | 13% | 14% |
| Breast lump | 75% | 69% | 69% | 66% | 77% |
| Axillary lump | 2% | 2% | 0% | 5% | 0% |
| Breast pain | 5% | 3% | 6% | 3% | 2% |
| Axilla/arm pain | 1% | 1% | 3% | 1% | 2% |
| Amenorrhea | 1% | 0% | 0% | 0% | 0% |
| Blood secretion | 1% | 3% | 3% | 1% | 1% |
| Other secretions | 2% | 4% | 3% | 2% | 2% |
| Breast pain and lump | 4% | 1% | 3% | 3% | 0% |
Chi squared P = .072.
Association between presenting symptom of breast cancer and recruitment province.
| Recruitment provinces | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Asturias | BCN | Cantabria | Girona | Gipuzkoa | Huelva | León | Madrid | Navarra | Valencia | |
| Symptoms | n = 44 | n = 123 | n = 58 | n = 17 | n = 96 | n = 61 | n = 125 | n = 201 | n = 86 | n = 28 |
| Asthenia | 9% | 0% | 3% | 6% | 3% | 0% | 2% | 1% | 1% | 18% |
| Changes in the breast | 11% | 12% | 19% | 18% | 14% | 16% | 6% | 9% | 9% | 7% |
| Breast lump | 64% | 75% | 57% | 71% | 73% | 72% | 81% | 73% | 77% | 61% |
| Axillary lump | 0% | 2% | 2% | 6% | 1% | 3% | 0% | 2% | 1% | 0% |
| Breast pain | 5% | 4% | 12% | 0% | 5% | 0% | 5% | 2% | 6% | 0% |
| Axilla/arm pain | 2% | 2% | 2% | 0% | 1% | 0% | 1% | 0% | 0% | 7% |
| Amenorrhea | 2% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 1% | 0% |
| Blood secretion | 0% | 1% | 0% | 0% | 2% | 0% | 0% | 3% | 2% | 0% |
| Other secretions | 5% | 2% | 2% | 0% | 1% | 3% | 2% | 4% | 1% | 4% |
| Breast pain and lump | 0% | 2% | 3% | 0% | 0% | 5% | 1% | 5% | 1% | 4% |
Chi squared P < .001.
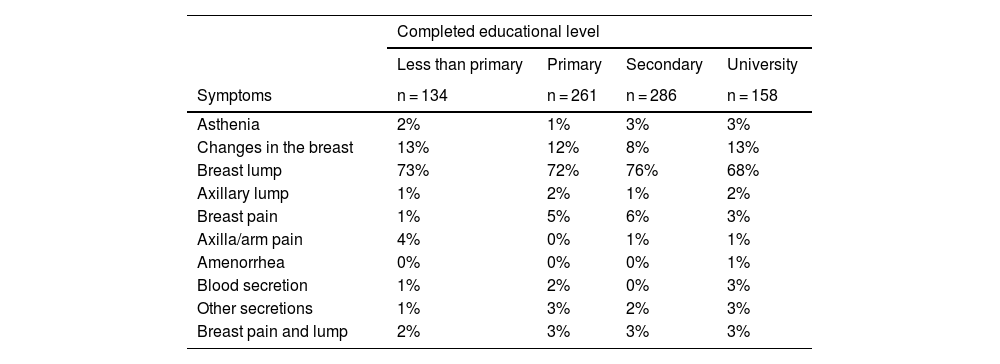
Association between presenting symptom of breast cancer and educational level.
| Completed educational level | ||||
|---|---|---|---|---|
| Less than primary | Primary | Secondary | University | |
| Symptoms | n = 134 | n = 261 | n = 286 | n = 158 |
| Asthenia | 2% | 1% | 3% | 3% |
| Changes in the breast | 13% | 12% | 8% | 13% |
| Breast lump | 73% | 72% | 76% | 68% |
| Axillary lump | 1% | 2% | 1% | 2% |
| Breast pain | 1% | 5% | 6% | 3% |
| Axilla/arm pain | 4% | 0% | 1% | 1% |
| Amenorrhea | 0% | 0% | 0% | 1% |
| Blood secretion | 1% | 2% | 0% | 3% |
| Other secretions | 1% | 3% | 2% | 3% |
| Breast pain and lump | 2% | 3% | 3% | 3% |
Chi squared P = .59.
Association between presenting symptom of breast cancer and the menopause.
| Menopause status | ||
|---|---|---|
| Postmenopausal | Premenopausal | |
| Symptoms | n = 487 | n = 352 |
| Asthenia | 0 | 3% |
| Changes in the breast | 13% | 8% |
| Breast lump | 71% | 75% |
| Axillary lump | 2% | 1% |
| Breast pain | 3% | 5% |
| Axilla/arm pain | 1% | 1% |
| Amenorrhea | 0% | 1% |
| Blood secretion | 2% | 1% |
| Other secretions | 3% | 2% |
| Breast pain and lump | 2% | 4% |
Chi squared P = .056.
The most common presenting symptom in the women who mention at least one symptom was that they noticed a “lump in the breast” (73%), followed a long way behind by noticing “changes in the breast” (11%). “Pain in the breast” (4%), “asthenia”, “secretions other than blood”, and a “painful lump in the breast” at 3% each one all scored less than 5%. A “lump in the axilla” was the first symptom in only 2% of cases, and lastly “secretion of blood from the breast” or “pain in the axilla or arm” only represented 1%. Among the “changes in the breast” retraction of the nipple, retraction of other parts of the breast, a hard breast, itching in the breast and changes in the shape or coloration of the nipple all stood out.
A slight tendency was observed between increasing age and a higher frequency of mentioning “changes in the breast” (P = .072), although there was no clear patter n for the other symptoms (Table 2).
Table 3 shows the association between the recruitment province and the presenting symptoms. The outstanding finding here is a certain degree of variability in the proportion of women with a “lump in the breast” depending on the province (from 57% in Cantabria up to 81% in León). The variation in symptoms was greatest for “changes in the breast”, which occurred up to 3 times more often in Cantabria (19%) than was the case in León (6%) or Valencia (7%).
Regarding the association between the presenting symptom and the patient’s educational level (Table 4), a certain tendency was found for them to express a presenting symptom other than a “lump in the breast” as their educational level rose. Nevertheless, a “lump in the breast” was the most prevalent symptom for the patients of all the educational levels (P = .059).
Table 5 shows the association between the presenting symptom and the menopause, with differences bordering on statistical significance (P = .056) as the postmenopausal women mentioned noticing “changes in the breast” (13%) more often than those who were premenopausal (8%).
Respecting the other sociodemographic variables, no association, tendency or pattern were observed between the presenting symptom of the breast cancer and the marital status of the women. The frequency with which a “lump in the breast” was found only varied from 69% to 76% for the different categories of marital status. Nor were any differences found in the distribution of the most common presenting symptom between those women who were solely housewives and those who were not (10% in both groups). No pattern at all was found when their socioeconomic level according to their job was crossed with their presenting symptom.
No differences were found in terms of whether or not they smoked and the type of presenting symptom. Although the women with a BMI higher than 30 had a lower prevalence of “lump in the breast” (65%), in those with a BMI lower than 18.5 and the highest prevalence of “changes in the breast” (18%) in women with a normal BMI, the differences were not found to be statistically significant. Hardly any differences were observed in the prevalence of mentioning “lump in the breast” with different numbers of pregnancies to term (71%–75%). Nor was any association found between the presenting symptoms of the tumour and a first-degree family history of breast cancer.
DiscussionFrom the primary prevention viewpoint,8 the data from the population study confirm the high prevalence of noticing a “lump in the breast” as the presenting symptom, although “changes in the breast” was mentioned by no less than 10% of the symptomatic women. The most important added value of this study consists of its contribution to secondary and tertiary prevention. The relatively relevant geographical differences that were detected in reporting the frequency of symptoms are surely associated with cultural factors. Although the presence of a “lump in the breast” is always the most common symptom, differences amounting to 24 percentage points were found between the province where “lump in the breast” was the most frequent symptom (81% in Leon) compared to the province where it was the least common (Cantabria, at 57%). The opposite pattern was found for “changes in the breast” in both provinces, where it was mentioned three times more often by women in Cantabria (19%) than it was by those in León (6%). On the other hand, women with a higher educational level were found to be more likely to report symptoms other than a “lump in the breast” than those with a lower educational level. This may indicate the need to insist more intently with uneducated women on whether they had noticed anything other than a “lump in the breast”, in secondary prevention as well as in the diagnosis and to detect possible side effects after treatment has commenced. A similar recommendation may be made due to the possible tendency towards a higher probability of mentioning “changes in the breast” with increasing age and especially postmenopausal women in comparison with premenopausal ones. The increase in age leads to a rise in oncological breast pathology. These women are subjected to less conservative treatments because they are diagnosed in advanced stages.18 The differences in the diagnosis of premenopausal and postmenopausal women should be interpreted while taking into account changes in the breasts and hormonal alterations. Furthermore, the criteria which should be applied also have to be taken into account, including age and being able to take part in screening programmes. On the other hand, a family history of cancer or breast cancer does not seem to influence the type of presenting symptom. The symptoms of breast cancer are relevant for treatment, so that they can be differentiated from any possible side effects of the therapy that is used. There can be no doubt that continuous clinical training and updating the knowledge of medical personnel in clinical epidemiological advances regarding our patients with breast cancer will improve the efficacy of our medical departments, bringing forward early diagnosis and improving patient management.
Some Autonomous Communities such as Andalusia have protocols which define the inclusion criteria for the breast cancer detection process and programme (2017). These protocols take certain symptoms and clinical signs into consideration as suspicious: a palpable nodule, pathological secretion (unilateral, single pore and spontaneous), and changes in the areola nipple complex (inversion, retraction, ulceration, thickening, oedema or inflammation). The meaning of symptoms associated with changes in the breast (the second most common presenting symptom in our study as an alarm signal) should be evaluated in population-based prospective studies. The WHO underlines the importance of having reliable referral routes from primary health care institutions to district hospitals and specialized oncological centres. These protocols can always be updated, and an updated referral protocol makes it possible to shorten waiting times between the suspicion of a tumour and diagnosis of the disease.
Knowledge of breast cancer symptoms has advanced thanks to multiple studies of women diagnosed with the condition.2 The WHO World Initiative against Breast Cancer has the aim of reducing the worldwide mortality due to cancer by 2.5% per year, thereby preventing almost 2.5 million premature deaths due to breast cancer from 2020 to 2040 in women under the age of 70 years. Although early detection programmes meet their set objectives, we should not forget that the said programmes are applied in a specific age band. It is important to educate the population about breast cancer symptoms, as this would permit early detection outside the programmes for this purpose. Many patients currently state that access to Primary Care is difficult, so that the population should be given enough resources to ensure that they do not visit at too late a stage. It is important to emphasize that although self-examination does not replace a mammography, it is a way of raising the alarm so that a doctor is consulted in case of any suspicion. The important role of nurses stands out here. According to the results of a review study which evaluated the effects of interventions managed by nurses, including education, patient reminders, advice and guidance, nurse interventions were found to double the rate of mammography acceptance, clinical breast examinations and regular self-examination of the breasts.19 It should also be pointed out that intervention by nurses also improved knowledge about cancer, belief in early detection and the cases in which pre-cancerous lesions were detected.19 Equally, a study undertaken of 133 Brazilian nurses in 38 basic health units concluded that the training and the time used in activities for the early detection of breast cancer had a positive influence.20
Although it is based on a multicentre population study with incident cases confirmed histologically, this study has limitations respecting the interpretation of its results. The information about symptoms was obtained directly from the patients, without being checked against their clinical histories, and this may give rise to poor data classification.21 Although it was based on 836 symptomatic patients, the low frequency of the majority of symptom types hinders obtaining sufficient statistical power to detect whether any important differences exist for the sociodemographic variables and symptoms other than a “lump in the breast”.
To conclude, the most frequent presenting symptom was the appearance of a “lump in the breast”, followed by “changes in the breast”. Although the frequency of the type of presenting symptom may vary according to sociodemographic variables, new studies would be required to examine these questions in greater depth, as they are highly important for the identification of different profiles in the design of specific nursing interventions.
FundingThis study was financed by grants PI12/00150 and PI17CIII/00034 of the Carlos III Health Institute-FEDER-Una manera de construir Europa, as well as by “Acción transversal del cáncer”, approved by the Ministry of Science on 11 October 2007, and other competitive grants from the Carlos III Health Institute-FEDER (PI08/1770, PI08/0533, PI08/1359, PI09/00773, PI09/01286, PI09/01903, PI09/02078, PI09/01662, PI11/01403, PI11/01889-FEDER, PI11/00226, PI11/01810, PI11/02213, PI12/00488, PI12/00265, PI12/01270, PI12/00715, PI14/01219, PI14/0613, PI15/00069, PI17/02286), of the Fundación Marqués de Valdecilla (API10/09), of the Consejería de Salud de la Junta de Andalucía (2009-S0143), of the Fundación Caja de Ahorros de Asturias and by Oviedo University, by the Agencia de Gestión de Ayudas Universitarias y de Investigación (AGAUR) of the Beca de la Generalitat de Catalunya2017SGR723, of the Asociación Española Contra el Cáncer (AECC) Fundación Científica grant GCTRA18022MORE. Huelva University. Junta de Andalucía (Fondos FEDER)UHU-202077.
AuthorshipAll of the authors contributed substantially (1) to the conception and design of the study, or data gathering, or data analysis and interpretation, (2) to writing the draft version of the paper or the critical review of the intellectual content, and (3) in the definitive approval of the version presented here.
Conflict of interestsThe authors have no conflict of interests to declare.
To all of the patients who took part in the study, as without their collaboration it would not have been possible.