Purpura fulminans (PF) is a serious complication of sepsis resulting from a set of alterations characterised by the development of ecchymotic haemorrhagic lesions and skin necrosis.
AimTo analyse the efficacy and safety of the topical application of HOFA compound, in the cutaneous microcirculation of PF lesions in paediatric patients affected by sepsis.
Material and methodsA prospective quasi-experimental pre-test/post-test single-group conducted in a Paediatric Intensive Care Unit of a third level hospital was performed. Paediatric patients aged 0–18 years with sepsis were included. Somatic oximetry values were measured before and after application of HOFAs every 4h over the first three days of the patients’ hospitalisation. Patient’s socio-demographic and clinical variables and somatic oximetry by placing a sensor for measuring tissue perfusion on the area with PF were determined.
ResultsFour patients were recruited, with a median age of 98 months. The purpuric lesions measured were mainly located on both feet and hands and, in two patients, also on the lateral malleoli and calves of both lower extremities. A total of 225 measurements were obtained, with mean pre-intervention scores of 71.17±15.65% versus 73.68±14.83% post-intervention. Statistical significance (p<0.001) was observed upon comparison of the pre- and post-intervention measurements.
ConclusionsEarly and continued application of HOFAs in the management of sepsis-induced PF is an effective and safe practice in the cases analysed. In more than half of the episodes analysed, an increase in tissue microcirculation was observed after the application of HOFAs, with no adverse events.
La púrpura fulminante (PF) es una complicación grave de la sepsis resultado de un conjunto de alteraciones caracterizadas por el desarrollo de lesiones hemorrágicas equimóticas y necrosis de la piel.
ObjetivoAnalizar la eficacia y la seguridad de la aplicación tópica de un compuesto de ácidos grasos hiperoxigenados (AGHO) en la microcirculación de la púrpura fulminante (PF) en pacientes pediátricos afectados de sepsis.
Material pacientes y métodoSe llevó a cabo un estudio prospectivo cuasi-experimental pretest-post-test de un solo grupo en una Unidad de Cuidados Intensivos Pediátrica (UCIP). Se incluyeron en el estudio pacientes con PF de 0 a 18 años. Para evaluar la efectividad del producto objeto de evaluación en la microcirculación de las lesiones por PF se determinaron los valores de oximetría somática antes y después de la aplicación de AGHO cada 4 horas durante los tres primeros días de ingreso de los pacientes.
ResultadosSe reclutaron 4 pacientes, con una mediana de edad de 98 meses. Las lesiones purpúricas que se midieron estaban ubicadas, sobretodo, en ambos pies y manos y, en dos pacientes, también en los maléolos laterales y gemelos de ambas extremidades inferiores. Se obtuvieron un total de 225 mediciones, observando unas puntuaciones medias pre intervención de 71.17±15.65% versus los 73.68±14.83% post intervención. Se objetivó significación estadística (p<0.001) al comparar las mediciones pre y post intervención.
ConclusionesLa aplicación precoz y continuada de AGHO en el manejo de la PF por sepsis es una práctica eficaz y segura en los casos de población pediátrica analizada. En más de la mitad de los episodios analizados se objetivó un aumento de microcirculación tisular tras la aplicación de los AGHO, sin eventos adversos.
What is known?
- •
Purpura fulminans (PF) is a severe complication of sepsis resulting from a combination of alterations characterised by the development of ecchymotic haemorrhagic lesions and necrosis of the skin.
- •
The hyperoxygenated fatty acids (HOFA) are produces composed of essential fatty acids and characterised by presenting properties such as increasing the micro blood circulation, reducing the effect of ischaemia.
What this paper contributes?
- •
Hyperoxygenated fatty acids in the treatment of purpura fulminans induced by sepsis are an effective and safe practice in the paediatric cases analysed.
- •
In over half of the episodes analysed, an increase in tissue microcirculation was observed after the application of the HOFA, without adverse events.
Implications for clinical practice
- •
Skin treatment with hyperoxygenated fatty acids is used as an adjunct to local treatment for complex and ischaemic wounds, such as purpura fulminans.
- •
Further studies are required to evaluate how other parameters or possible treatments, such as protein C and the administration of vasoactive drugs may affect the evolution of these ischaemic wounds and the development of sequelae in paediatric patients affected by sepsis.
Sepsis is defined as an ever-changing clinical and pathophysiological process caused by microbial pathogenicity and the host's response to this aggression, which may go through several stages that define its stage and severity. We can classify this type of pathology into sepsis, severe sepsis and septic shock.1 Severe sepsis is the stage with the highest mortality rate, especially when associated with septic shock.
An epidemiological study on the incidence of severe sepsis indicates that it is increasing.2 A recent review based on eight studies from different countries estimated an overall incidence of sepsis of 22–240 cases/105 persons, of severe sepsis at 13–300/105 and of septic shock at 11/105.3
If we focus on the paediatric population, sepsis records are scarce and partial. In 2010, the WHO estimated that nearly 7.6 million children under 5 years of age die annually, most of them from infectious diseases (64%). In a Spanish study conducted in seven Paediatric Intensive Care Units (PICU) published in 2014, the estimated incidence of sepsis was 5.6/105 children/year.4
A subsequent report by the WHO in 2013 estimated that more than 50% of mortality in children under 5 years of age was due to infection and that more than 6,000,000 children died per year from sepsis. All these data are reinforced by the Sepsis Prevalence Outcomes and Therapies (SPROUT) study published in 2015, which describes a hospital mortality rate of 25% for this pathology.5
Among the complications of severe sepsis, purpura fulminans (PF) is the result of a cluster of disorders characterised by the development of ecchymotic haemorrhagic lesions and skin necrosis of variable size and depth.6 FP is therefore the term used to describe these rapidly progressive haemorrhagic dermal lesions with fever, septicaemia and shock that have been observed to occur in 10%–20% of sepsis. These lesions are a skin manifestation associated with disseminated intravascular coagulation (DIC), which is caused by the infection or sepsis and also by the host response and is characterised by skin necrosis and small vessel thrombosis.7
PF is a very serious disease, which begins acutely, evolves and spreads rapidly throughout the body, affecting the lower limbs, and ends with the subsequent formation of necrotic plaques as a sign of tissue and even organ damage in the affected area.8
Another of the alterations caused by the septic process is DIC, which increases the risk of developing PF. This process develops due to an activation of blood coagulation, which generates thrombin in excess, thus forming fibrin thrombi in the microcircultion.9,10 For this reason, ischaemic lesions secondary to PF in paediatric patients with sepsis can leave serious sequelae, including limb amputation, due to thrombotic occlusion of small and medium-sized vessels.11,12
Somatic oximetry measurement can be useful for the diagnosis of peripheral vascular disease (PVD), or the determination of critical lower limb ischaemia (LLIM).13 In order to determine the degree of ischaemia that PF can cause in the microcirculation, a somatic oximetry meter can be used, a device that allows the quantification of oxygen delivery from the respiratory system to the tissues by determining its levels in the bloodstream.
Somatic oximetry is a non-invasive technique for monitoring changes in tissue oxygen metabolism. This method is based on near-infrared spectroscopy (NIRS) technology that diffuses near-infrared light photons into the patient's skin. After spreading inside the skin, some of these photons return to the skin by reflectance. By counting the number of returning photons, it is possible to conclude what the spectral absorption of the inner tissue has been and to estimate its average oxygenation. To determine tissue oxygenation by NIRS, two sensors located at two different distances from the transmitting point are used. The difference between the two signals will provide the signal corresponding to the tissue located below the sensors.14
Hyperoxygenated fatty acids (HOFA) are products composed of essential fatty acids that have undergone a hyperoxygenation process and are characterised by properties such as increasing blood microcirculation, reducing the effect of ischaemia, enhancing epidermal cell attachment, facilitating epidermal cell renewal, increasing skin resistance, protecting against friction, preventing skin dehydration, reducing skin fragility and reducing the effect of free radicals in the extracellular matrix.15
Regarding the effect of HOFA in skin care, there is experimental evidence that Mepentol® (Alfasigma, Barcelona) a compound of hyperoxygenated fatty acids with oleic and linoleic acids (essential acids), when applied topically, develops a pro-inflammatory effect that facilitates the regeneration of the skin mantle and stimulates the production of cytokines (VEGF and IL-1) by neutrophils to stimulate the formation of new blood vessels and thus accelerate healing.16 The formation of new blood vessels increases microcirculation in areas at risk of ischaemia.
In an inflammatory process, such as might occur in sepsis, oxygen free radicals have a major impact on the development of the ischaemic process. Thus, an excess of free radicals contributes to the destruction of the endothelium by causing more platelets and granulocytes to appear, inducing blood flow stasis, producing microthrombosis and, as a consequence, reducing blood flow and activating the formation of necrotic tissue. Hyperoxygenation of fatty acids has been studied to reduce the formation of free radicals.16 This is why, in accordance with the supporting evidence, the aforementioned HOFA product is used empirically in our institution in the skin care of patients with PF as a complementary measure of local treatment to minimise the extension of the areas of necrosis, with positive effects determined by direct clinical observation and evolutionary control in the PF of paediatric patients with sepsis.
The relevance and necessity of this study lies in the fact that there is no scientific evidence available in the paediatric field on the effectiveness and effect on the microcirculation of this product in the evolution of purpuric lesions due to sepsis.
Objectives- -
To analyse the efficacy and safety of the topical application of Mepentol®, a compound of hyperoxygenated fatty acids (HFOFA) in the microcirculation of purpura fulminans (PF) in paediatric patients affected by sepsis.
- -
To describe the main characteristics of patients with PF and their lesions.
- -
To determine somatic oximetry in purpuric lesions in paediatric patients affected by sepsis before and after the protocolised application of HOFA and to detect possible differences.
- -
To determine the complications that arise after topical application of HOFA to the skin of paediatric patients with PF secondary to sepsis.
A single-group prospective quasi-experimental pre-test-post-test study was conducted in a 24-bed Paediatric Intensive Care Unit (PICU) located in a tertiary maternal and paediatric hospital of national reference in Barcelona, Spain. The research was conducted from September 2017 to January 2022.
The study population consisted of patients who met the following inclusion criteria: (i) age between 0 and 18 years, and (ii) admitted to the PICU with sepsis and the presence of FP. Children presenting criteria of critical ischaemia with absence of distal pulses were excluded. Due to the absence of studies that have investigated the relationship between HOFA and FP, the present pilot study was conducted in the PICU of a tertiary hospital. Therefore, the sample calculation was not determined, but the centre's caseload of 2–3 cases per year of sepsis with these characteristics was taken as a reference. Patients were selected on a non-probabilistic and consecutive basis.
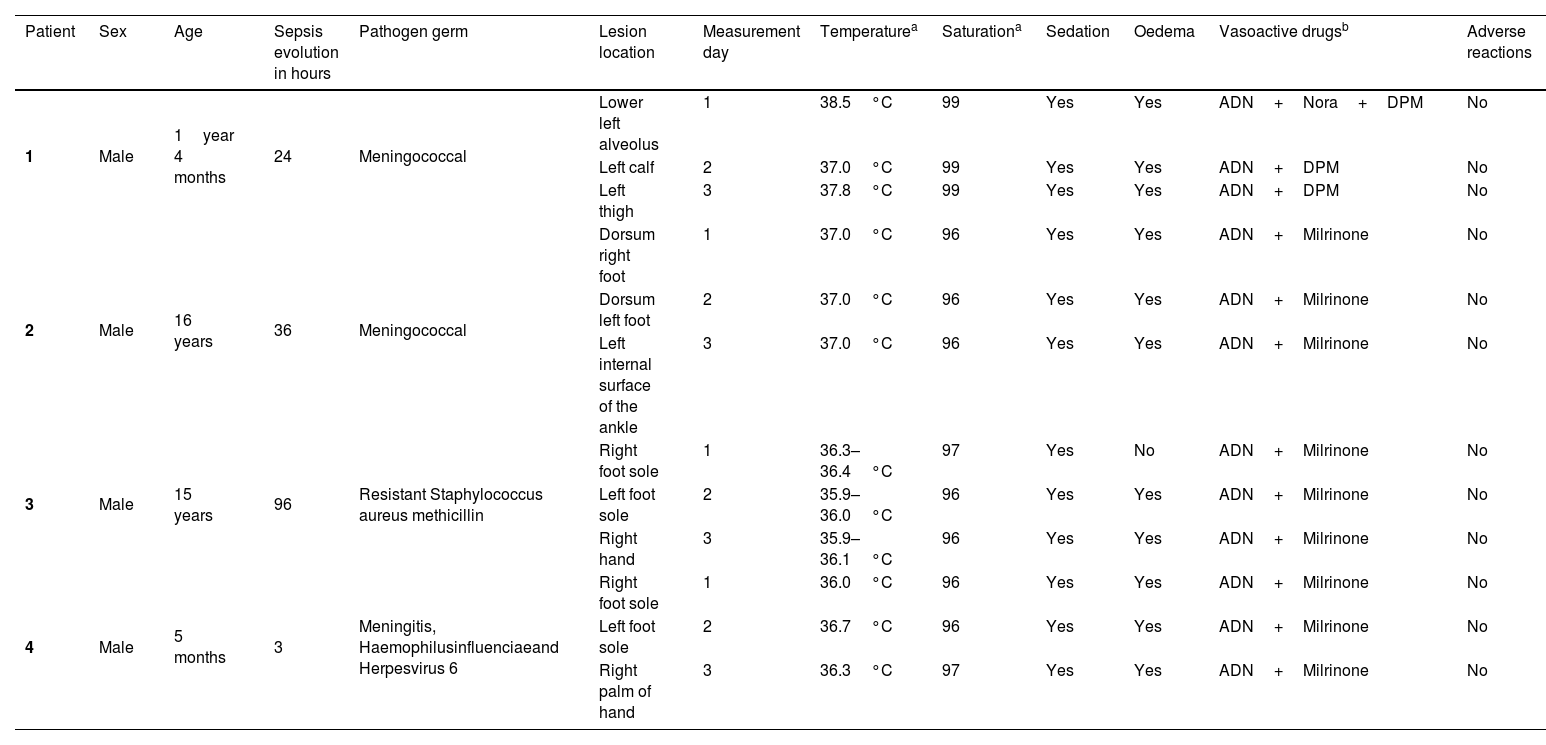
The following socio-demographic and clinical variables were recorded for each case: (i) sex (male/female), (ii) age (in months), (iii) hours of evolution of the disease, (iv) time (in days and hours) that had elapsed since the first symptoms began to appear until admission to the PICU, (v) pathogenic germ involved, (vi) location of lesions, (vii) core temperature (measured at rectal or oesophageal level), (viii) haemoglobin saturation, (ix) sedation (yes/no), (x) vasoactive drugs (yes/no), (xi) type of vasoactive drug and (xii) presence of oedema (yes/no). In addition, somatic oximetry was determined by placing a tissue perfusion measurement sensor at the FP site and potential adverse reactions to HOFA were monitored. The presence or absence of haemodynamic disturbances or skin rash after HOFA application were considered as adverse reactions.
InterventionThe main intervention in the study was the application of HOFA to the most affected purpuric areas. For this purpose, Mepentol®, a class II B medical device (topical use on intact skin and superficial skin lesions) with experimental and clinical evidence,15 was used as HOFA, which comes in a spray with a valve that prevents contamination. This product is composed of hyperoxygenated fatty acids, Equisetum arvense, which improves skin elasticity and tonicity, and Hypericum hypericum, with erythema-preventive and normalising properties and soothing and dermoprotective activity.
Data collection procedureAn ad hoc procedure and grid was designed to record all the data. This procedure consisted of:
- 1
On admission of a sepsis patient with FP, the principal investigator informed the family of the study and its objectives and requested informed consent (IC) for their participation.
- 2
Once participation was accepted, all sociodemographic and clinical variables were recorded. In addition, the 3 or 4 most affected areas with PF were identified in order to proceed with the application of HOFA and determination of somatic oximetry. Here, priority was given to the most extensive and visually necrotic lesions. In order to standardise the interventions and data collection, three training sessions lasting approximately one hour were held in morning, afternoon and evening shifts for all the nurses in the PICU where the study was carried out. The objectives and methodology of the study were explained, detailing that two sprays of HOFA should be applied and that the compound should be spread smoothly over the lesion and perilesional area. In addition, it was explained how the oximetry measurements were to be taken and recorded before and after the intervention.
- 3
For each patient, up to a maximum of 3 purpuric areas were selected for HOFA application, prioritising those most affected.
- 4
Somatic oximetry values were determined for each of the selected lesions by placing a NIRS sensor and the values were recorded.
- 5
Two sprays of HOFA were applied to the selected lesions and perilesions, spreading the product gently with the fingers.
- 6
After 30min of HOFA application, the product was gently removed with a gauze and the measurement of somatic oximetry was repeated and the values recorded.
- 7
The procedure described in points 4 and 5 was repeated every 4h during the first 3 days of the patient's admission.
To describe the variables of the patients included in the study, descriptive statistics were used with frequency measures for qualitative variables and measures of central tendency, shape and position for quantitative variables. To evaluate the effect of the intervention and somatic oximetry values before and after HOFA application, Student's t-test was performed. A 95% confidence interval was established and data were considered statistically significant if p-value <.05.
Ethical considerationsThis research was conducted in accordance with state and autonomous community regulations on clinical studies. The patient data obtained were protected in accordance with current legislation on data protection, as well as respecting the bioethical principles contemplated in the Belmont Report and the Declaration of Helsinki. Prior to conducting the study, authorisation and permission was requested from the Ethics and Clinical Research Committee of the "eliminated by review" (PIC-170-16), to ensure compliance with ethical principles and standards of good practice and good research practice, as well as from the nursing management of the centre where the study was conducted.
Before patients were included in the study, they were informed verbally and in writing of the purpose of the research and asked to sign the informed consent form. In this case, as it was a paediatric population, the patient's parents or legal guardians were asked if they wished their children to take part in the study, informing them at all times of the objective of the research, the procedure and the possibility of withdrawing from the study if they deemed it necessary. In the case of patients over 12 years of age, if they were conscious and oriented, they also gave their consent/assent after receiving the necessary information adapted to their level of understanding.
ResultsFour patients were recruited during the study period, all of whom presented a highly critical condition with hyperthermia and haemodynamic instability. Two of them died during admission. The age of the patients was 1year and 4 months; 16 years; 15 years; and 4 months (median 98 months). The main pathogenic organisms implicated in sepsis and PF occurrence were: meningococcus, resistant staphylococcus aureus meticillin, haemophilus influenciae and Herpes virus 6.
The purpuric lesions measured were mainly located on both feet and hands and, in two patients, also on the lateral malleoli and calves of both lower extremities. All patients were mechanically ventilated, continuously perfused and on inotropic support, with adrenaline, noradrenaline, dopamine and milrinone being the most commonly used drugs. The mean temperature of the patients was 36.8°C, with some moments of hyperthermia (maximum 38.5°C), and the mean haemoglobin saturation (HbSat) was 97% (Table 1). If we analyse the somatic oximetry measurements broken down by patient, we observe the following results:
- -
Patient 1 (follow-up period of 3 days):
Sociodemographic and clinical characteristics of the patients.
| Patient | Sex | Age | Sepsis evolution in hours | Pathogen germ | Lesion location | Measurement day | Temperaturea | Saturationa | Sedation | Oedema | Vasoactive drugsb | Adverse reactions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 1year 4 months | 24 | Meningococcal | Lower left alveolus | 1 | 38.5°C | 99 | Yes | Yes | ADN+Nora+DPM | No |
| Left calf | 2 | 37.0°C | 99 | Yes | Yes | ADN+DPM | No | |||||
| Left thigh | 3 | 37.8°C | 99 | Yes | Yes | ADN+DPM | No | |||||
| 2 | Male | 16 years | 36 | Meningococcal | Dorsum right foot | 1 | 37.0°C | 96 | Yes | Yes | ADN+Milrinone | No |
| Dorsum left foot | 2 | 37.0°C | 96 | Yes | Yes | ADN+Milrinone | No | |||||
| Left internal surface of the ankle | 3 | 37.0°C | 96 | Yes | Yes | ADN+Milrinone | No | |||||
| 3 | Male | 15 years | 96 | Resistant Staphylococcus aureus methicillin | Right foot sole | 1 | 36.3–36.4°C | 97 | Yes | No | ADN+Milrinone | No |
| Left foot sole | 2 | 35.9–36.0°C | 96 | Yes | Yes | ADN+Milrinone | No | |||||
| Right hand | 3 | 35.9–36.1°C | 96 | Yes | Yes | ADN+Milrinone | No | |||||
| 4 | Male | 5 months | 3 | Meningitis, Haemophilusinfluenciaeand Herpesvirus 6 | Right foot sole | 1 | 36.0°C | 96 | Yes | Yes | ADN+Milrinone | No |
| Left foot sole | 2 | 36.7°C | 96 | Yes | Yes | ADN+Milrinone | No | |||||
| Right palm of hand | 3 | 36.3°C | 97 | Yes | Yes | ADN+Milrinone | No |
Seventy-four paired measurements were performed. The mean value of pre-intervention measurements was 67.2±19.5%, while the mean value of post-intervention measurements was 70.5±18.5%. Statistically significant data (p≤.05) were obtained after comparing pre- and post-intervention measurements. At the same time, post-intervention measurements were found to be 0.8%–5.7% higher than the corresponding pre-intervention measurements.
- -
Patient 2 (follow-up time of 3 days):
Fifty-eight paired pre-post intervention measurements were carried out. The mean value of the pre-intervention measurements was 75.6±14.6% versus 79.2±12.7% post-intervention (Fig. 1). After comparing both values a p-value <.05 was observed, so we considered the result statistically significant. The post-intervention measurements were 1.7%–5.4% higher than the corresponding pre-HOFA measurements.
- -
Patient 3 (follow-up time of 3 days):
Sixty-three paired pre-post HOFA measurements were recorded. The mean value of the pre-intervention measurements was 72.6±7.4%, while the mean of the post-intervention determinations was 74.4±7.7%. When comparing the pre- and post-intervention values, statistically significant data were obtained (p≤.05). In the case of patient 3, analyses estimated differences of 0.1%–3.4% between pre- and post HOFA measurements.
- -
Patient 4 (Follow-up time of 3 days):
Thirty paired pre-post intervention measurements were assessed. The mean value of the pre-intervention measurements was 69.2±17.5%, while the mean value of the post-intervention measurements was 69.3±16.8%, with no statistically significant relationship (p=.96). It is worth considering that this patient came with a highly evolved state of sepsis and that he died three days later, which may lead us to consider why the HOFA did not have an impact on the post-application values in this patient.
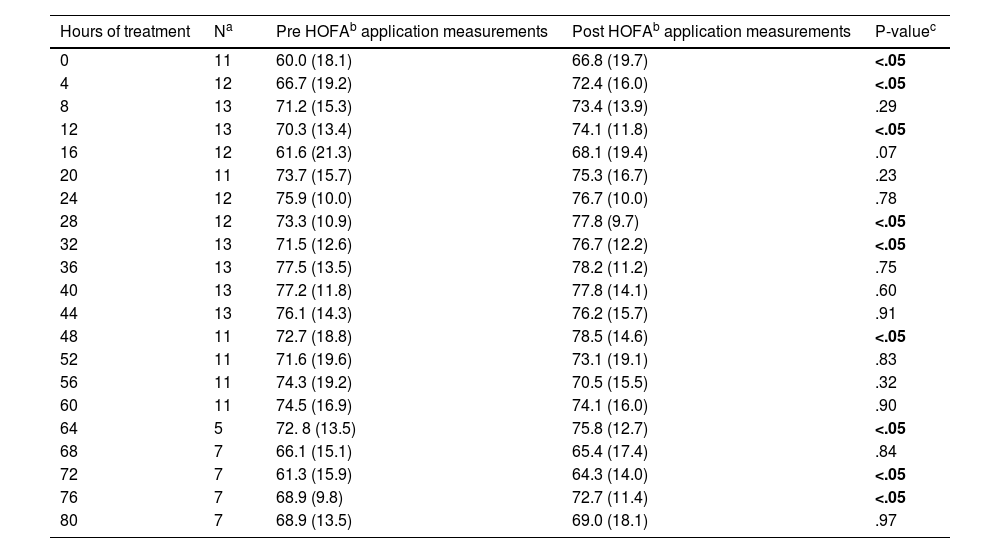
In relation to the global data recorded, a total of 225 measurements were obtained, with mean pre-intervention scores of 71.2±15.6% versus 73.7±14.8% post-intervention, with a significant relationship (p≤.05). It can therefore be seen that there is a statistically significant difference between the pre and post HOFA measurements in the globality of the data obtained, obtaining higher mean scores of between 1.3% and 3.6% in the post-intervention determinations. When analysing all the data obtained by hours, there was a tendency for the values to improve during the first hours (at the beginning, at 4, 12, 28 and 32h of HOFA application), Table 2.
Analysis of somatic oximetry according to hours of hyperoxygenated fatty acid application.
| Hours of treatment | Na | Pre HOFAb application measurements | Post HOFAb application measurements | P-valuec |
|---|---|---|---|---|
| 0 | 11 | 60.0 (18.1) | 66.8 (19.7) | <.05 |
| 4 | 12 | 66.7 (19.2) | 72.4 (16.0) | <.05 |
| 8 | 13 | 71.2 (15.3) | 73.4 (13.9) | .29 |
| 12 | 13 | 70.3 (13.4) | 74.1 (11.8) | <.05 |
| 16 | 12 | 61.6 (21.3) | 68.1 (19.4) | .07 |
| 20 | 11 | 73.7 (15.7) | 75.3 (16.7) | .23 |
| 24 | 12 | 75.9 (10.0) | 76.7 (10.0) | .78 |
| 28 | 12 | 73.3 (10.9) | 77.8 (9.7) | <.05 |
| 32 | 13 | 71.5 (12.6) | 76.7 (12.2) | <.05 |
| 36 | 13 | 77.5 (13.5) | 78.2 (11.2) | .75 |
| 40 | 13 | 77.2 (11.8) | 77.8 (14.1) | .60 |
| 44 | 13 | 76.1 (14.3) | 76.2 (15.7) | .91 |
| 48 | 11 | 72.7 (18.8) | 78.5 (14.6) | <.05 |
| 52 | 11 | 71.6 (19.6) | 73.1 (19.1) | .83 |
| 56 | 11 | 74.3 (19.2) | 70.5 (15.5) | .32 |
| 60 | 11 | 74.5 (16.9) | 74.1 (16.0) | .90 |
| 64 | 5 | 72. 8 (13.5) | 75.8 (12.7) | <.05 |
| 68 | 7 | 66.1 (15.1) | 65.4 (17.4) | .84 |
| 72 | 7 | 61.3 (15.9) | 64.3 (14.0) | <.05 |
| 76 | 7 | 68.9 (9.8) | 72.7 (11.4) | <.05 |
| 80 | 7 | 68.9 (13.5) | 69.0 (18.1) | .97 |
Post HOFA measurements were higher in 156 cases (69.3%), in 19 cases (8.4%) pre and post measurements were equal and in 50 cases (22.2%) post measurements were lower than pre intervention.
No statistically significant differences were observed between the pre- and post-intervention data for the various socio-demographic and clinical variables analysed, nor did they differ according to the anatomical area of measurement. At the same time, it was found that no complications appeared after topical application of HOFA to the skin in any of the cases studied.
DiscussionAll of the articles reviewed note the severity of sepsis processes in the paediatric population with a very high mortality rate. Among the complications derived from severe sepsis, purpura fulminans (PF) is characterised by the development of haemorrhagic and ecchymotic lesions and skin necrosis. It begins acutely and spreads rapidly over the whole body, affecting the lower limbs and ending with the subsequent formation of necrotic plaques that often lead to limb loss. Given the severity of the disease, priority is given to haemodynamic stabilisation of the patient and management of the septic condition without initially treating PF with the functional consequences that this can trigger. Even so, no paediatric studies have been found that specify the effectiveness and safety of the application of specific topical treatments to improve or reduce the progression of purpura fulminans, and no research reports evidence of the benefits of increasing tissue oxygenation in areas affected by PF, as reflected in the pilot study presented here. The present study shows that the application of hyperoxygenated fatty acids could have an impact on the treatment of PF due to sepsis, since in the first measurement after their application, and even beyond 32h, an improvement in the degree of tissue oxygenation of the lesions analysed was observed. This idea is contrasted in another study which reports the case of a neonatal patient treated in a similar way and in which an improvement in the perfusion of the purpuric lesions was observed after application of HOFA.17 In our study, 3 of the 4 patients improved their cutaneous microcirculation levels after HOFA application. In relation to the measurements, post-intervention improvements were observed in almost 70% of the measurements.
Vasoactive drug treatments are considered a risk factor for developing pressure injuries in critically ill patients, since their vasoconstrictive effect reduces peripheral perfusion.18 All the patients in the study required support with vasoactive vasoconstrictive drugs during the first day, incorporating vasoactive support with milrinone in the second, third and fourth cases, due to its vasodilator effect, to try to improve the distal ischaemia of their extremities. We could associate the benefit of this vasodilator drug to the improvement of the purpura, if this had also been applied in the first case. However, in the first patient, not only were vasodilators not used, but three different types of vasoconstrictor drugs were administered. Even so, the improvement in tissue oxygenation of the purpuric areas studied was high, so HOFA may have played an important role in this.
It is known by various authors that in sepsis, the inflammatory response that occurs develops an alteration in the DIC with an imbalance in coagulation that will lead the patient to suffer small thrombi, which are the main cause of tissue damage in the areas of smaller vessels. Part of this coagulation imbalance is the result of the loss of protein C. This protein mainly inactivates coagulation factors V and VII, which prevents thrombin generation and thrombus formation.19,20 Such is the importance of ensuring correct levels of protein C that one study describes its application in the treatment of PF in patients with congenital protein C deficiency, showing stabilisation of coagulation parameters.21 Even so, it is important to note that the evidence for the administration of human protein C concentrates and recombinant activated protein C in the management of fulminant meningococcal sepsis is disputed in the literature with unclear conclusions,22 and further studies are needed to contrast the effectiveness and safety of these treatments in the management of paediatric patients with sepsis.
Another documented therapeutic alternative in the absence of activated protein C is the administration of fresh plasma, together with anticoagulants such as heparin and warfarin. The authors of this study performed the largest series of cases of PF of non-septic aetiology, but due to congenital protein C deficiency. Patients with congenital protein C deficiency also present with ecchymosis that rapidly progresses to necrosis and gangrene, requiring debridement treatment and a high risk of amputation, as do those affected by septic PF20. For these reasons, their clinical management can serve as an example for the management of paediatric patients with PF due to sepsis.
Although the present study did not analyse the presence of protein C deficiency, a retrospective study of 94 paediatric cases administered non-activated protein C showed recovery or improvement of PF lesions in 79.8% of cases, unchanged in 13.8% and deterioration in 6.4% of cases.23 Therefore, the determination of protein C deficiency should be taken into consideration in future research and in the management of paediatric patients with PF due to sepsis.
In addition to the above, treatment of purpuric lesions requires debridement of necrotic areas, escharectomies, fasciotomies and/or amputations. This treatment should not be undertaken early. It is preferable to start when the lesion borders are well defined and demarcated and there are no signs of infection such as the presence of purulent exudate indicating deterioration of the perilesional area. Typical use of HOFA facilitates the delineation of such areas. Coverage of the debrided areas with dermal grafts and allografts is also often necessary, plus subsequent healing with advanced therapies such as negative pressure therapy.24
The differences in the composition of the different HOFA products on the market condition their possible mechanism of action, and therefore the results of this study are only applicable to the product used in the research.
LimitationsThe main difficulty and limitation of this study is the lack of studies with which to compare the results and the sample size included, as this is a pathology with a very low incidence. Although it was initially planned to include a larger number of patients, the introduction of the meningococcal vaccine in the routine vaccination schedule in Catalonia made this difficult because, fortunately, the incidence of cases of paediatric patients affected by FP due to sepsis decreased. Even so, the results obtained provide evidence to treat both those paediatric cases that are still present in the context of the study and those that occur in countries where this vaccine is not included in the systematic calendar. In addition, it is proposed to expand the sample of this pilot study, extending the research to a multicentre context.
Another limitation of the study is the design. A randomised clinical trial (RCT) should have been conducted for this study to demonstrate a direct relationship between HOFA application and improvement of microcirculation in the PF of paediatric patients with sepsis. The aforementioned sample limitation made this difficult. Furthermore, in the case of an RCT, limiting access to HOFA in some patients would have presented the research team with an ethical and moral dilemma, leaving patients without an option that has been shown to be effective and exposing them to a greater number of sequelae related to PF. Finally, it is important to note that only male subjects could be included in this research. Although no gender differences are expected to be found, this is intended to be addressed in future extensions of the study.
ConclusionsThis study shows how the early and continuous application of HOFA in the management of PF due to sepsis is an effective and safe practice in the paediatric population analysed. In more than half of the episodes analysed, an increase in tissue microcirculation was observed after the application of HOFA, with no adverse events. Even so, the impact of other variables related to the clinical management of the paediatric critical patient affected by PF due to sepsis, such as the decrease or absence of protein C and the administration of vasoactive drugs, on the evolution of these ischaemic lesions and the development of sequelae should be analysed.
FundingThis study has been fully or partially funded by the Fundación Enfermería y Sociedad del Colegio Oficial de Enfermeros y Enfermeras de Barcelona within the framework of the Ayudas competitivas a la Investigación Enfermera (PR-242/2017).
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to explicitly thank the nursing team and the medical team of the PICU of the hospital where the study was carried out, as well as the management of the centre and the Official College of Nurses of Barcelona for facilitating the study.