Family centered developmental care (FCDC) are a philosophy of care in the neonatal care units (NICU), based on the control of sensory stimulation the adequate position and of newborn and the family involvement of cares. Nursing staff are the main providers of this care. Sanitary measure to control of the COVID-19, such as the use of masks, isolation of positive cases and capacity limit, conditioned the implementation of FCDC.
ObjectivesTo understand the meaning of the experience of the nursing staff of a neonatal intensive care unit (NICU) on the implementation of the FCDC, under the sanitary measures imposed for the containment of COVID-19.
MethodsA qualitative study was conducted from the descriptive phenomenological paradigm in which NICU nurses were recruited. The qualitative data collection was carried out through open-ended and semi-structured interviews. These were analyzed respectively through a preliminary narrative analysis and a thematic analysis of the informant nurses’ narratives and discourses.
ResultsThree open-ended and 7 semi-structured interviews were conducted from which three main topics emerged: 1) changes in the FCDC derived from the sanitary restrictions implemented for the containment of COVID-19; 2) changes in interpersonal relationships in the context of a pandemic, and 3) transition to normality.
ConclusionsThe nurses of NICU perceived changes in the implementation of the FCDC due to the containment of COVID-19, that modified the relationship with the parents of NB, accelerating their training as caregivers, and involved the implementation of new measures such as video calls.
Los cuidados centrados en el desarrollo y la familia (CCDF) son una filosofía de atención dentro de las unidades de cuidados neonatales (UCIN) basada en el control de los estímulos ambientales, el correcto posicionamiento y manejo de los recién nacidos (RN) y la implicación de las familias en sus cuidados. Las enfermeras son los principales proveedores de estos cuidados. Las medidas sanitarias implantadas para el control de la pandemia por la COVID-19, como el uso de mascarillas, el aislamiento de casos positivos, el mantenimiento de la distancia de seguridad y la limitación de aforos, han condicionado la implementación de los CCDF.
ObjetivosComprender el significado de la vivencia de las enfermeras de una UCIN sobre la implementación de los CCDF, bajo las medidas sanitarias impuestas para la contención de la COVID-19.
MétodosSe llevó a cabo un estudio cualitativo desde el paradigma fenomenológico descriptivo en el que participaron enfermeras de una UCIN. La recogida de los datos cualitativos se realizó mediante entrevistas abiertas y semiestructuradas. Estas se analizaron respectivamente mediante un análisis narrativo preliminar y un análisis temático de las narrativas y discursos de las informantes.
ResultadosSe realizaron 3 entrevistas abiertas y 7 semiestructuradas, de las que surgieron tres temas principales: 1) cambios en los CCDF derivados de las restricciones sanitarias implementadas para la contención de la COVID-19; 2) cambios en las relaciones interpersonales en contexto de pandemia, y 3) transición hacia la normalidad.
ConclusionesLas enfermeras de una UCIN percibieron cambios en la implantación de los CCDF por las medidas de contención de la COVID-19, que modificaron la relación con los progenitores de los RN, acelerando su formación como cuidadores, y supusieron la implementación de nuevas medidas, como las videollamadas.
Family-centred developmental care (FCDC) is a philosophy of care based on interventions aimed at optimising the neurodevelopment of newborns admitted to neonatal intensive care units (NICU), and facilitating an active role from families in their care. Some of the interventions that make up this philosophy of care, such as skin-to-skin contact and training the family in the management of the newborn, appear to have positive effects on the cardio-respiratory status of the newborn and the reduction of stress as well as fostering the emotional bonding of the newborn with his or her parents.
Provision of this care was affected by the health restrictions imposed against COVID-19, especially the limitations on the accompaniment of newborns, the maintenance of interpersonal safety distance, and the isolation of mothers and fathers, and of the newborn itself if they tested positive for the virus.
What it contributes?The study shows the experience of nurses in a NICU in relation to the adaptation of their care work to the COVID-19 containment measures for the appropriate administration of FCDC. The objectives of this philosophy of FCDC were mainly to foster bonding between newborns and their parents and to facilitate the transition to the next stages of life and care.
This is of great interest, given that the pandemic resulting from COVID-19 was a novel and uncertain situation, which posed a great challenge to the performance of health care by health professionals. In this sense, there have been several publications on the experience of nurses in intensive care units during the pandemic context, but there are few studies on what happened in the NICU and more specifically in relation to FCDC.
Study implicationsSpecial situations involving social distancing measures and extraordinary precautions in interpersonal relationships, such as those implemented by COVID-19, condition the application of FCDC in NICUs. Some consequences of these measures are impossible to mitigate, given the importance of direct interaction between newborns, their families and nursing professionals for the FCDC. However, the results of the study present some complementary measures such as the use of technological supports such as video calls with families or a greater performance of the nurses’ teaching work, adapting and speeding up the training process for parents as caregivers. These measures have been maintained and contribute to improving the FCDC.
In the year 2020 in Spain, approximately 7% of births occurred early before 37 weeks of gestation, a percentage that has been maintained over the last two years.1 Two per cent of this 7% corresponds to births below 28 weeks or very preterm, among which those born between 22 and 25 weeks are identified as extreme preterm. Those born above 32 weeks are considered moderate preterm and those born between 34 and 35 weeks are considered late preterm. In 2019, the neonatal mortality rate (mortality between 0 and 28 days of life) was 2 deaths per 1000 live births in Spain, one of the lowest in Western Europe (average rate 2.3 per 1000 live births).2,3
The potential health risks of preterm births are proportional to the weight and weeks of gestation (higher risk with weight <1500 g; gestation <26 weeks). The main complications in these infants are related to respiratory immaturity, haemodynamic instability and infections.4
The reference service for the care of preterm infants is the NICU. These are hospital units dedicated to the care of preterm newborns or those with other morbid conditions, with specialised staff and technical support. Within the NICU, technical advances such as non-invasive ventilation, non-invasive monitoring systems such as amplitude electroencephalography, transcutaneous bilirubinometer and multi-parameter monitors have improved care in these units.5,6
CCDF is based on interventions aimed at optimising neurosensory and emotional development and facilitating an active role of families in the care of the NB.7 Specifically, the World Health Organisation defines CCDF as “a broad range of interventions designed to reduce the physical and neurological stress of preterm infants in the NICU”.8 The basis of these strategies is the monitoring of environmental stimuli (light, sound, humidity and temperature), the appropriateness of positioning and handling, the safeguarding of sleep and the recognition of the family as a fundamental pillar in the hospitalisation and life of the RN.9,10 The philosophy of the FCDC seeks to encourage the application of methods such as skin-to-skin contact, in addition to training the family in the management of the child and promoting bonding between mothers and fathers and the newborn.10
The implementation of this care is not only a matter of procedures, but of a paradigm shift in the attitudes of health professionals in the care of NBs and their families.11 The role of nurses is fundamental in implementing FCDC and integrating the family in the care of the NB. Nurses are responsible for educating the family on hospital admission, during hospitalisation and at the time of discharge, in addition to acting as a figure available to listen to and resolve doubts.12
In Spain, information has been available on the implementation of FCDC since 1999, with the greatest implementation being observed between 2006 and 2012.13 Since 2020, the COVID-19 pandemic has required the implementation of health measures and changes in the application of FCDC in NICUs, especially conditioned by the limitations on hospital visits and the reduction in the length of stay of mothers and fathers in the units. unidades14,15 In addition to these restrictions, other measures were implemented, such as the permanent use of masks, social distancing and limited capacity in NICUs.16,17
In general, the pandemic affected the care work of health personnel and had a significant impact on the care of NBs and their families in NICUs.18 However, in the face of this health emergency scenario and taking into consideration that nurses are essential in the implementation of the FCDC, only one study has been located that describes the experiences of NICU nurses during the pandemic, but without addressing the model of care.19 For this reason, it is of interest to know, from the nursing perspective, the impact of the pandemic, in relation to the incorporation of prevention measures against COVID-19, on the implementation of FCDC in the NICU.
Therefore, the general objective of the present study was to understand the meaning of the NICU nurses’ experience of the implementation of the FCDC under the health measures imposed for the containment of COVID-19. The specific objectives were: 1) to understand the nurses’ perception of the changes arising from the health measures imposed against COVID-19; 2) to describe the role of NICU nurses in relation to the integration of the family in the FCDCs, under the health restrictions imposed against COVID-19; 3) to identify new methodologies for implementing the FCDCs under the health measures imposed against COVID-19.
MethodDesignIn response to the proposed objectives a qualitative study was conducted from the paradigm of descriptive phenomenology based on the philosophy of Husserl.20
ScopeThe study was conducted during the months of March and April 2022, two years after the beginning of the COVID-19 pandemic in Spain, in the NICU of a tertiary level hospital.
SampleThe sample consisted of NICU nurses from a tertiary level hospital in Madrid. Purposive sampling was used in the context of the investigation, in order to gather initial information on the phenomenon to be studied. The inclusion criteria were: 1) being a nurse who had worked in the hospital’s NICU for some time between March 2020 and March 2022 and 2) having training on the FCDC. The exclusion criteria were established: 1) not working in the participating NICU during the data collection period due to leaving the service, sick leave, vacation or leave of absence.
Data collectionData collection was carried out in two phases, in which the individual interview was used as a tool to obtain information. All the interviews were conducted in a separate room within the service of the participating NICU, to facilitate the accessibility of the respondents to the interviews, as well as to ensure their privacy and confidentiality. The dates and times of the interviews were agreed with the participants through their email. Each interview had an estimated maximum duration of 50 min. All interviews were audio recorded and field notes were taken. The semi-structured interviews were carried out cumulatively and sequentially, until the information was saturated.
In the first phase, open interviews were conducted in order to explore an unknown field, to get to know the participants and their experiences, given the scarcity of qualitative studies on FCDCs during the pandemic to date. The question that was asked was “How have the FCDCs been carried out during the pandemic in the NICU?” Two weeks later, after the transcription and preliminary narrative analysis, a second phase of semi-structured interviews was carried out to probe into key aspects detected in the initial interviews. The script for these interviews consisted of 3 open-ended questions related to the objectives of the study and organized according to their relevance in the initial interviews: 1) “What changes have you perceived in care from the health service measures against COVID-19?; 2) How has the relationship with families been and their integration of care for their child after the health restrictions imposed in response to COVID-19?; 3) What new methodologies have been implemented to maintain FCDCs during the COVID-19 pandemic?
Data analysisThe qualitative data obtained from the open interviews were transcribed and analysed by two researchers through preliminary narrative analysis of the participants’ narratives. This analysis allowed a natural approximation to the subjectivity of the informants, which facilitated the construction of stories and the elaboration of the script of the semi-structured interviews.21
The data from the semi-structured interviews were analysed using the technique of thematic analysis of narratives and discourses from the descriptive phenomenological paradigm,21 according to Braun and Clarke.22,23 Two researchers became familiar with the qualitative data extracted by transcribing the recordings of the interviews into text, reading and rereading them, which were complemented with field notes. They generated the initial codes of the most relevant aspects. Subsequently, the codes were compiled into possible topics and subtopics, eliminating redundant information.
Through the construction of concept maps, they identified units of topics and subtopics that helped describe and understand the experience of the participants. In this way, they generated definitions and names for each topic and subtopic. Finally, they related the topics and subtopics with the study objectives and its theoretical framework. To ensure the transparency of the study, the transcripts were sent to the participants by email and they were informed of the results, if they so desired.
Methodological accuracyThe reliability of the collected qualitative data was verified by comparing the coding of the two investigators who coded the transcripts independently. Subsequently, the consistencies and discrepancies between them were identified and agreed.
The thematic analysis of the narratives and discourses of the respondents was carried out in parallel by a person familiar with the qualitative phenomenological methodology and by a professional from the study group. The emerging topics and subtopics were then compared and unified to maintain the reliability of the results. Throughout the research, the criteria of methodological rigor in qualitative research proposed by Guba and Lincoln24 were followed. In addition, for the verification of the qualitative data collected, the application of different data collection methods (open interview, semi-structured interview and researcher’s field notes), the verification of the content of the transcripts of the interviews by the interviewers themselves and the presentation of the preliminary thematic analysis to the participants were used as control techniques. To control the rigor and quality of the qualitative methodology, the Consolidated Criteria for Reporting Qualitative Research COREQ)25 criteria were followed.
Ethical considerationsThe study was previously authorised by the Research Commission of the Hospital’s Research Institute. The study was carried out under the indications of the Declaration of Helsinki. The processing of personal data complied with the provisions of EU Regulation 2016/679 of the European Parliament and of the Council of April 27, 2016 on the protection of natural persons with regard to data processing. And the free circulation of these data and the Organic Law Organic Law 3/2018, of December 5, on the protection of personal data and guarantee of digital rights.
Prior to any data collection, the participants were informed orally and with the delivery of the information sheet about the study objectives and procedures and the ethical considerations, and they were asked to sign an informed consent. Before the start of the interviews, permission was requested from the participants to record them. Anonymity was maintained through a simple coding process, assigning each participant an alphanumeric code. All data and voice recordings were encrypted and archived on an external hard drive with access code. Once the data necessary for the fulfilment of the objectives had been extracted, this material was completely destroyed.
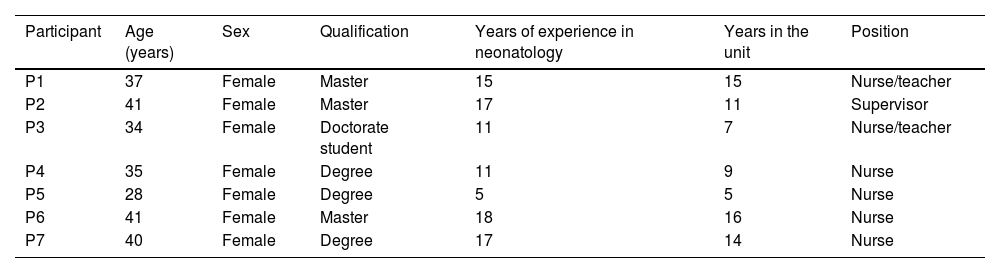
ResultsTo achieve the proposed objectives, 7 nurses who were active during the COVID-19 pandemic period in the hospital’s NICU participated in the study. All the participants were women between the ages of 28 and 41, nursing graduates. Three had master’s postgraduate training and 1 was enrolled in a doctoral programme. All had experience in the NICU between 5 and 16 years (Table 1).
Participant characteristics.
| Participant | Age (years) | Sex | Qualification | Years of experience in neonatology | Years in the unit | Position |
|---|---|---|---|---|---|---|
| P1 | 37 | Female | Master | 15 | 15 | Nurse/teacher |
| P2 | 41 | Female | Master | 17 | 11 | Supervisor |
| P3 | 34 | Female | Doctorate student | 11 | 7 | Nurse/teacher |
| P4 | 35 | Female | Degree | 11 | 9 | Nurse |
| P5 | 28 | Female | Degree | 5 | 5 | Nurse |
| P6 | 41 | Female | Master | 18 | 16 | Nurse |
| P7 | 40 | Female | Degree | 17 | 14 | Nurse |
Three open interviews and 7 semi-structured interviews were conducted. The 3 nurses who agreed to ask the open-ended questions also participated in the semi-structured interviews two weeks later. After the thematic analysis of the semi-structured interviews, 3 main topics were obtained, from which 8 sub-topics were identified.
Topic 1. Changes in the FCDC derived from the health service restrictions implemented for the containment of COVID-19Subtopic 1.1. Negative overall changesAmong the aspects that make up the FCDC, all the respondents highlighted the restrictions to perform the kangaroo method as the most negative change. The nurse is in charge of positioning the NB on the carrier’s chest, but the need to maintain interpersonal distance made it impossible to approach the fathers and mothers. “No father or mother could be denied the kangaroo method, but as long as they did it themselves… you could be there a bit, assisting with the cables, instruments and suchlike, but the main point was that they did it” (P1)
They also referred to the reduction in visits to the NICU by mothers and fathers as negative changes. The restrictions on movement in the streets, together with the parents' fear of infecting their children, reduced their presence during visiting hours. In addition, both parents could not be simultaneously in the NICU, having to take shifts that affected breastfeeding. Visits from siblings and grandparents were prohibited. “That lack of closeness, that lack of contact, I think it interfered a lot with breastfeeding… the parents were no longer able to take part in the caring for the baby because they couldn’t be there or there could only be one of them… I don’t know the statistics, but I can say that they came less, they spent fewer hours with their children” (P3)
Another of the most difficult experiences they report was the case of mothers with a positive COVID result. These mothers had to remain in total isolation from their admission to the Hospital. After giving birth they were separated from the newborn and skin-to-skin contact was denied to them. In these cases, the newborn was hospitalized in the NICU under strict isolation and with a ban on visits, some newborns staying up to 15 days without contact with family members. As knowledge about the disease and the control of the pandemic increased, the visit of a relative outside the main nucleus with a negative PCR test began to be allowed. “We have had parents who have spent ten days, fifteen days without being able to see their son who was in hospital…” (P7)
Among the changes imposed, the respondents recognised positive aspects that helped to facilitate the application of the FCDC. The mothers and fathers maintained access to the unit, but to maintain the interpersonal safety distance, the physical approach of the health team to them was limited. For this reason, the learning time for parents in the management of NBs was accelerated, in relation to the time spent pre-pandemic. The teaching work of nurses was intensified to expedite the assumption of the role of caregivers of the mothers and fathers. “Visits were never prohibited… We have always worked a lot with parents… we always try to tell them that the sooner they are autonomous and independent to pick up their child, the better because there is less manipulation and the child suffers fewer position changes. And they did it soon… well, in a relatively short time, but it is true that now with the pandemic they do it much sooner.” (P1)
Video calls were also implemented as a method so that mothers and fathers isolated by the virus could meet, see and be informed about the status and evolution of the newborns. This measure has been maintained and its use has been expanded for families who live in far away and cannot go to the hospital daily. “We made video calls every day, morning and afternoon or morning or afternoon, depending a bit on the availability of the nurse, but she stayed with my father, they gave us WhatsApp and the video call was made on WhatsApp with a tablet provided by the service.” (P4) “We all have the means to be able to make video calls. If we have a child admitted and the parents cannot come for whatever reason, I think it will continue.” (Q7)
As it was a pandemic caused by a new virus (SARs-CoV-2), the implementation of the new measures went through an exploratory period. The respondents stated that ignorance generated a period of changes and uncertainties. The implemented action protocols were constantly modified, even within periods of 2 or 3 days. These variations raised doubts in practice and, in some cases, even inconsistency in the information provided to mothers and fathers. “Suddenly I couldn’t see any of them, how could only one be there, how could they be there for half an hour, how could there suddenly be two, but then suddenly things started to get worse and only one could be there… that misinformation in saying” No, but your partner has told me that I can stay. “Okay, well, something has changed and I didn’t find that out because of course, since information received is ever changing, you don’t know what to do at any one time in any one day.” (Q3) “There were not many clear things that could be said, every other day a protocol changed, every other day an idea changed… what do we do?… what they say is effective today, tomorrow is not, so we have done it wrong and now we are in danger.” (P5)
One of the first protocols prohibited the use of the kangaroo method, which caused discomfort and disagreements in the team, given the benefits that this method brings to the development of premature infants. Despite the prohibition, the nurses decided to go ahead with the application of the method, reinforcing the measures that guaranteed the safety of mothers, fathers and newborns, as well as nurses. “Well, at the beginning of feeding, in the end you comfort that child with suction, its hands to its mouth, but it is definitely not the same, and with regards to the children who had oxygen, well, bad adaptations or transient tachypnea or well… Children who are not accompanied by their parents, who do not have a comprehensive follow-up regime, are children who take longer to wean themselves off oxygen, to learn to eat, that is to say, I don’t know this for sure, it’s true, but I’m sure they logically took longer” (P6)
On the other hand, part of the adaptation of the nurses was to develop the criteria to apply exceptions, such as allowing the presence of the family in the mourning process. “There was no explanation for a child who was going to die… you have to identify what is happening and in that case you have to let them both in and that’s what was done” (P2)
Regarding the feelings that the pandemic aroused in the respondents, one of the most repeated concepts was “fear”. Fear on the part of mothers and fathers as they feared contracting the virus and infecting their children. Fear on the part of nurses for working in a hospital with infected people admitted to it and fear of contact with families as a possible source of contagion. “I think that the fear they had was of going into the hospital…many reported that they were afraid of entering the hospital, in case they got infected on the way and could transmit it to the children.” (P1) “We would have preferred for no one to come, but of course, our idea had been to bring parents closer and then this came about … so it kind of slows you down and changes your chip of not letting anyone in because there is a risk.” (P3)
Some participants pointed out that their greatest fear was the possibility that COVID-positive mothers would not survive and not get to meet their children. “Through the glass of the obstetrics ward beds, the mother told us what the girl was going to be called and then she left, I mean, she had her glasses on, she could sit up, sit on the bed and she said “She’s going to be called Virginia” and well, that was terrifying because you didn’t know if that mother was going to see her daughter girl again.” (Q6)
The participants indicated that their relationship with the NBs remained the same as it had been before the pandemic. Initially, an attempt was made to reduce physical contact to avoid infecting them and to reduce the possibility of being infected by a newborn from a COVID-positive mother. Once it was known that there was no transmission of the virus from the mother to the foetus through the placenta, physical contact with the newborn was maintained as usual. The limitations of distance and direct interaction with the newborn were maintained while they were accompanied by their parents. “I don’t think so… I think that with the baby there was not such a fear, we quickly appreciated that the babies were barely affected by COVID and that it was not even transmitted from the mother to the baby when it was in the womb, so I think that fear soon disappeared.” (P2) “It is not the same to be touched with a glove as it is to be touched by skin, the contact is skin-to-skin, but I have to admit that at the beginning I wore gloves to work, so perhaps that contact was less, you are being touched by plastic, you are not being touched by warm, soft skin…” (P3) “Well, in my case, perhaps I am a little more reticent about closeness, because you often have to be on top of the child with the father on top of you, so there is no distance at all…” (P4)
In general, the participants commented that, despite the time of uncertainty and stress for the families due to the state of the newborns and the evolution of the SARs-CoV-2 infections, the mothers and fathers were understanding and cooperative. The quality of relationships between nurses and parents was not affected. Mothers and fathers accepted and respected the new restrictions and were grateful for initiatives such as videoconferencing, which mitigated the impossibility of NICU visits. “Really grateful because they said that they got to know a colleague a lot because she always showed up with the baby, right? She took him, “cuddled” him and made the video call so that the parents could see that the baby was well loved and welcomed, and the child was comfortable.” (P1) “Well, the best service in the hospital by far compared to the rest… in fact, the parents have totally shown us their gratitude. The support that was given to them, as much as we were able, because nobody knew… we became nurses, psychologists, everyone, without really being them, and well, trying to do it in the best possible way and with the best will.” (P2)
Furthermore, the participants highlighted their teaching role linked to the development of the FCDC and that it contributed to the promotion of interpersonal relationships with families: the training received on the management of their children was the vehicle for mothers and fathers to face restrictions and encourage their participation in care. “What we try to do is encourage that as much as possible, that is, encourage parents to have autonomy in caring for their babies as soon as possible.” (P2)
However, some of the accounts of the interviewees show that the pandemic generated duality in the relationships between professionals and families. On the one hand, mothers and fathers found the nurses to be people they could talk to and trust. However, on the other hand, there were those who felt that the pandemic emotionally distanced families from the team because, since there was a physical distance, it was unlikely that bonds would be formed beyond receiving clinical information. “It’s hard for me to tell a father to leave when his son is sick, I’m repeating myself again… I, as a nurse, say “how can they separate me from my daughter in her first few hours of life, are we crazy?… and the doubts, who do you ask? Well, whoever you trust the most, and trust is given by closeness, I am sure many parents have been left with doubts, they have not asked us things because of that lack of closeness, of empathy…, of everyone forming a team, I think that was lost for a while.” (P3)
In this sense, one respondent reflected on how difficult it was to be exposed to contact with the families of newborns, while they were deprived of accompanying their infected relatives. She explains that, as professionals, they know their role, but it seemed unfair to them to be deprived of contact with their loved ones, while they were exposed to the same illness that distanced them from their family.
Subtopic 2.3. Between nursesThe respondents commented that the moment that generated the greatest conflict was when, due to proximity restrictions, the nurses refused to perform the kangaroo method. This led to disagreements because they all recognized that this practice was a fundamental right. Differences also arose as to whether or not to allow the participation of mothers and fathers, given that there were established protocols that in some exceptional situations required further consideration, such as in the case of NBs in palliative care. “The problem that we had in nursing was the issue of the kangaroo method with… parents using that method because of the proximity that exists when a professional transfers the incubator or crib to the parents or vice versa. It was that, the mouth-nose proximity despite wearing a mask. So, well, yes, there was a lot of talk, the nurses initially refused, with immense pain in our hearts…” (P1) “Well, to reach agreements of this type, there was a great difference of opinion and a lot of discomfort, that is, there were times when there was a lot of discomfort from the nursing team, the medical team, in general.” (P2)
The experiences narrated by the nurses participating in this study about the modifications carried out in a NICU for the application of the FCDC during the COVID-19 pandemic, suggested three main themes. These themes emphasise the modifications in aspects related to the interaction between nurses, mothers and fathers and newborns, a cardinal aspect of the FCDC, and why the respondents referred to their work during the pandemic as being a difficult period. Most of the changes that conditioned the application of the FCDC during the pandemic, which respond to the objectives set out in this study, were those derived from the isolation and social distancing measures and not from the established hygiene measures.
In relation to the first objective, two points emerge: some changes that were perceived as negative and others perceived as positive. Regarding the negatives, the narrations of the nurses interviewed, as in the study by Coşkun et al., reveal that maintaining the interpersonal safety distance was the main condition for carrying out the kangaroo method, promoting breastfeeding and training of mothers and fathers.19 Although these changes were observed in all maternity services, Kang et al., point out that they had a special impact on the NICUs, since these are fundamental activities within the FCDC.26
Regarding the positive changes, these respond to the third objective set out in this study on the implementation of new methodologies to implement the FCDC under the healthcare measures imposed against COVID-19. To counteract the lower presence of parents in the NICU, the respondents highlighted the novel use of video calls that were well received by mothers and fathers and professionals. Pre-pandemic publications, such as those collected in the meta-analysis by Dol et al., also show good acceptance of the use of this technology in the NICU, which seems to strengthen the feeling of closeness of the family with newborns.27 However, although video calls have been defined as a successful initiative, they do not replace the presence and direct physical contact with the RN promoted by the FCDC. In this regard, Dol et al., pointed out that video calls seem to have no impact on the health status of hospitalized newborns, but they do have an impact on reducing stress in the family.27
In response to the second objective proposed, in the reports on the relationship of nurses with parents, a duality is present. As in the study by Coşkun et al., there are those who did not consider that the COVID-19 measures affected interaction and those who felt a certain distance from the families.19 This ambivalence in speech has also been observed in other studies of ICU nurses, so we could say that this phenomenon seems to be due to individual factors.28,29
In the development of FCDCs, several studies highlight the teaching role of nurses in developing the parental role and reducing the anxiety and stress generated by the admission of a child to the NICU.30,31 In this regard, the nurses in this study described their involvement in FCDC during the pandemic prominently as teachers. It has not been possible to contrast this opinion, given that the current literature on the role of nurses during the pandemic is mostly focused on clinical practice, i.e., modifications related to the use of equipment, techniques and mobility of units.32
Finally, the main limitation of this study is due to the fact that the participants belonged to the same NICU specialised in the FCDC. Another limitation is related to the fact that information saturation was achieved with 7 interviews, while a recent review concludes that between 9 and 17 interviews are necessary to achieve it,33 although these authors point out that this can be achieved with smaller homogeneous samples. Given these limitations, it would be advisable to conduct multicentre studies in different NICUs.
ConclusionsIn relation to the COVID-19 containment measures, the nurses in one NICU perceived changes that conditioned the application of the FCDC, such as a reduced presence of the mothers and fathers for the NBs, limitations in the application of the kangaroo method and the constant adaptation to new protocols for action. These changes conditioned the nurses’ direct relations with the parents. At the same time, the maintenance of the FCDC required the implementation of video calls and a greater performance of the nurses’ teaching work, adapting and speeding up the training process for parents as caregivers.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThis research has not received specific support from public sector agencies, the commercial sector or non-profit entities.
Please cite this article as: Martin-Caballero MB, Arrogante O, Martín-Casas P, Ortiz-Gutiérrez R. Modificaciones de los cuidados centrados en el desarrollo y la familia en cuidados intensivos neonatales durante la pandemia por COVID-19 en un hospital de España: un estudio cualitativo. Enferm Intensiva. 2023. https://doi.org/10.1016/j.enfi.2023.05.001