To establish the presence of alarm fatigue, the clinical relevance of alarms and the stimulus-response time of the health team in an Adult Intensive Care Unit.
MethodDescriptive, quantitative, observational study, developed in the Multipurpose Adult Intensive Care Unit. Population made up of health personnel and the ICU teams. The method used was non-participant observation. Follow-up was carried out over 120h in three months. The variables studied were number of alarms activated, time elapsed between the alert sound of the blood pressure parameter, heart rate and oximetry and the response of the health personnel who attended the alarm. A descriptive statistical analysis was carried out.
Results5147 alarms were detected, on average 43 alarms/h, of these 52.8% corresponded to multiparameter monitors and the rest to other equipment. Of those generated by multiparameter monitors, 37.3% were blood pressure, 33.4% oximetry and 29.3% heart rate. The clinical relevance was low in 42.7%, medium in 49.8% and high in 7.5%. The stimulus response time was between 0 and 60s for 37% of the alarms; however, 42.5% had no response, which is why they are considered fatigued. A statistically significant relationship was found between the response time and the clinical relevance of the alarms (p=0.000).
ConclusionsThe presence of alarm fatigue was evident; with predominance of clinical relevance in the middle and low ranges. The health personnel responded within the time established for timely attention to the non-fatigued alarms.
Establecer la presencia de fatiga de alarmas, la relevancia clínica de las alarmas y el tiempo estímulo-respuesta del personal de salud en una Unidad de Cuidados Intensivos (UCI) Adultos.
MétodoEstudio descriptivo, cuantitativo, observacional, desarrollado en una UCI Adulto Polivalente. Población formada por personal de salud y los equipos de la UCI. El método empleado fue la observación no participante. Se realizó seguimiento durante 120 horas en tres meses. Las variables estudiadas fueron: número de alarmas activadas, tiempo transcurrido entre el sonido de alerta del parámetro de presión arterial, frecuencia cardíaca y oximetría y la respuesta del personal de salud que atendió la alarma. Se efectuó análisis estadístico descriptivo.
ResultadosSe detectaron 5.147 alarmas, en promedio 43 alarmas/hora, de éstas 52,8% correspondieron a monitores multiparamétricos y el restante a otros equipos. De las generadas por los monitores multiparamétricos, 37,3% fueron de presión arterial, 33,4 de oximetría y 29,3% de frecuencia cardíaca. La relevancia clínica fue baja en 42,7%, media en 49,8% y alta en 7,5%. El tiempo de estímulo-respuesta fue entre 0 y 60 segundos en 37% de las alarmas; sin embargo, el 42,5% no tuvo respuesta, por lo cual se consideran fatigadas. Se encontró relación estadísticamente significativa entre el tiempo de respuesta y la relevancia clínica de las alarmas (p = 0,000).
ConclusionesEl alto número de alarmas sin respuesta, refleja la presencia de fatiga de alarmas en la unidad de estudio, con predominio de relevancia clínica en los rangos medio y bajo.
The evidence for alarm fatigue in ICUs has advanced to the level of systematic reviews, allowing it to be identified as a highly frequent problem in ICUs.
There are no studies that measure its incidence in Colombia, therefore we contribute to the development of knowledge of this phenomenon and highlight the important work of nurses in this area as the main responders to the needs of critical patients.
Implications of the studyAddressing alarm fatigue as a frequent problem in ICUs exposes the need to make adjustments in clinical practice, teaching and nursing management, specifically towards the personalisation of monitoring and awareness of increased irrelevant noise in ICUs, which has high negative impact and increases the risks to the safety of critically ill patients. It is a challenge for nursing research to continue developing studies towards minimising alarm fatigue and its consequences in critically ill patients.
Intensive Care Units (ICU) are highly complex hospital services where specialist care is provided to critically ill patients who require timely and quality care.1 The units have a variety of biomedical equipment to help support impaired functions, monitor vital signs and provide safe care minimising errors.2
One of the priority, standard and constant interventions during a patient's stay in ICU is non-invasive haemodynamic monitoring,3 which provides simultaneous information on physiological variables such as heart rate, respiratory rate, blood pressure and oxygen saturation. These multiparametric monitors have alarms that indicate adverse situations, an important factor in accurate and timely decision-making.
Despite the importance of monitors, their use in ICUs produces noise that sometimes exceeds 120dB,4 a situation that can lead to exhaustion and a failure to respond; this has been termed alarm fatigue.5 Fatigue is associated with a large number of alarms sounding at the same time, which makes it difficult to identify those that are clinically significant or relevant; causing relevant alarms to be neglected, silenced or ignored by health professionals.6
A systematic review identified the high prevalence and severity of alarm fatigue in developed countries; added to the 566 annual reports of the Food and Drug Administration (FDA) of patient deaths related to monitor alarms.7
A study conducted in Brazil reported that the mechanical ventilator generated the greatest number of audible alarm signals, followed by non-invasive arterial pressure (NIAP), the physiological parameter that produced the most fatigue or failure to respond to alarms, followed by SpO2 and ECG.6 Furthermore, a study in a Tokyo Adult ICU determined that 6.4% of the alarms were clinically relevant and that those triggered most frequently corresponded to blood pressure (33.5%), oxygen saturation (24.2%) and electrocardiogram (22.9%).8
All health professionals involved in critical patient care work with monitoring equipment and systems, particularly nurses, as they monitor at the bedside. They are also reported as responding most to alarms.9 However, a qualitative study conducted with 406 nurses in the United States reported desensitisation to alarms associated with hearing contamination, modification of parameters, lack of staff and obsolete equipment.10
The Emergency Care Research Institute (ERCI),11 the agency that monitors healthcare practices and devices in the United States, annually reports on the health hazards associated with the use of technology. In 2015, the Top 10 report first included hazards related to alarms, because of inadequate interaction between people and the devices. This is supported by multiple reports of alarm-related deaths and serious injuries.
Based on reports of adverse events caused by alarm failures, the Joint Commission proposed National Patient Safety Goals for 2015, with a focus on reducing the damage associated with clinical alarm systems.12 It is noteworthy that, in Colombia, until very recently, this issue was included in the priorities of patient safety and adverse event reporting.
The large amount of biomedical equipment, together with the high sensitivity and low specificity of alarms, can contribute to a delay in response time or indifference of health personnel, generating risk situations for the patient. Therefore, the objective of this research was to determine the clinical relevance of multiparametric monitor (MM) alarms and the stimulus-response time of the health team in the Adult ICU of a University Hospital.
MethodologyA descriptive, observational, prospective study, conducted in a Multipurpose Adult ICU in 2016, for three consecutive months, with a total of 120h of observation, 40 per month.
The ICU, with an average occupancy rate of 90%, had 21 beds equipped with all haemodynamic and ventilatory support equipment and a NIHON KOHDEN: PVM-2701 monitor at the bedside of each patient. The patients were surgical and internal medicine patients. The staff available to the unit were three intensive care physicians, three nurses, three therapists and 10 nursing assistants working in 6-h rotating shifts.
Study population: comprised health professionals: intensive care physicians, nurses, therapists, and nursing assistants, as well as the ICU medical technology devices. The following inclusion criteria were considered in selecting the study subjects: working in the ICU, being on duty during the observation periods and freely and spontaneously agreeing to participate. The 21 vital signs monitors located in each ICU cubicle were taken as the equipment. Thus, the study addressed the entire population of health personnel and ICU monitors, and therefore no sample or sampling was performed.
Study variables: Number of alarms activated, clinical relevance of the alarms, and time elapsed between the alert sound of the basic haemodynamic parameters NIAP, heart rate (HR), oxygen saturation (SpO2) and response of health personnel attending the alarm.
The haemodynamic parameters NIAP, HR and SpO2 were selected for monitoring because all ICU patients undergo this monitoring, and monitors are programmed to activate alarms in case of any variability in these three parameters that would represent a risk for the patient. Other parameters, such as invasive parameters, were omitted because not all the patients had them.
Data collection tools: Two data record sheets were designed, constructed from the literature review and with the contributions of three intensive care physicians and five intensive care nurses, who worked in other units. The first allowed data collection from all the equipment and the alarms activated during each day of observation. The second facilitated follow-up of the alarms activated by each monitor (NIAP, FC and SPO2), clinical relevance and their classification.13–15 Low relevance (alarm that does not require immediate action, but should be checked), Medium relevance (alarm followed by a diagnosis, therapeutic decision or solution of the technical problem), High relevance (alarm with direct clinical impact, which may compromise the life of the patient). This also recorded the healthcare professional who attended and interpreted the alarm and the stimulus-response time.
Data collection: After the endorsement of the institutional Ethics Committee, a meeting was held with the coordinators and care staff of the ICU, to provide information about the project, objectives, and methodology to be followed. After resolving any queries, the staff freely agreed to participate in the study, individually signing their informed consent, which authorised observation during the time of the study, in accordance with the ethical and legal principles inherent to scientific research.
The data was collected over three months, assigning 40h per month, 10 days of each month at random, with observation shifts of 4h during the day, to capture the variability of care. The information was collected by three student nurses specialising in intensive care, previously trained, with no work relationship with the institution, but recognised by the unit staff, since they had done their internship in this ICU earlier. Each was assigned seven beds for the respective follow-up, and therefore the unit staff knew in advance the days that they were collecting data, in accordance with the ethical guidelines.
The HR, NIAP and SpO2 alarms were physically monitored. Stimulus-response time information was counted with three chronometers, previously calibrated. Counting, in seconds, started from the moment the alarm was activated until the response by health personnel.
Statistical analysis: The physical records were attached to a database in Microsoft Excel. For this purpose, descriptive statistics, relative and absolute frequency distribution of the study variables were used. Data limits were calculated with 95% CI. Pearson's X2 test was applied in the bivariate analysis. All tests were identified as significant with a p<0.05 value. SPSS version 25 software was used for data processing.
Ethical considerations: The ethical principles for research on human beings (Declaration of Helsinki),16 the scientific, technical and administrative standards for health research in Colombia (Resolution 8430/1993)17 and the code of ethics for nurses (Law 911 of 2004)18 were considered in the development of the study. The classification of this research study was minimal risk.
ResultsA total of 5147 alarms were recorded in the monitoring time, for an average of 171 alarms per day and 43 per hour. Of these, 2718 (52.8%) corresponded to multiparametric monitors, the remainder to other equipment such as mechanical ventilators, intravenous medication infusion pumps, haemodialysis equipment, nutrition pumps, among others.
The alarms of the multiparameter monitors corresponded by 37.3% to the NIAP parameter, 33.4% to oxygen saturation and 29.3% to heart rate. In the same patient, two alarms were activated simultaneously in 35% of the cases, three in 15% and one in 50%.
The clinical relevance of the alarms was low in 42.4% of cases, medium in 50.1% and high in 7.5%. According to the measurement parameter, the relevance for SpO2 was low in 95.8%, medium in 2.8% and high in 1.3%; for HR it was low in 15.3%, medium in 72.1% and high in 12.4%, and for NIAP it was low in 16.4%, medium in 74.4% and high in 9.1%.
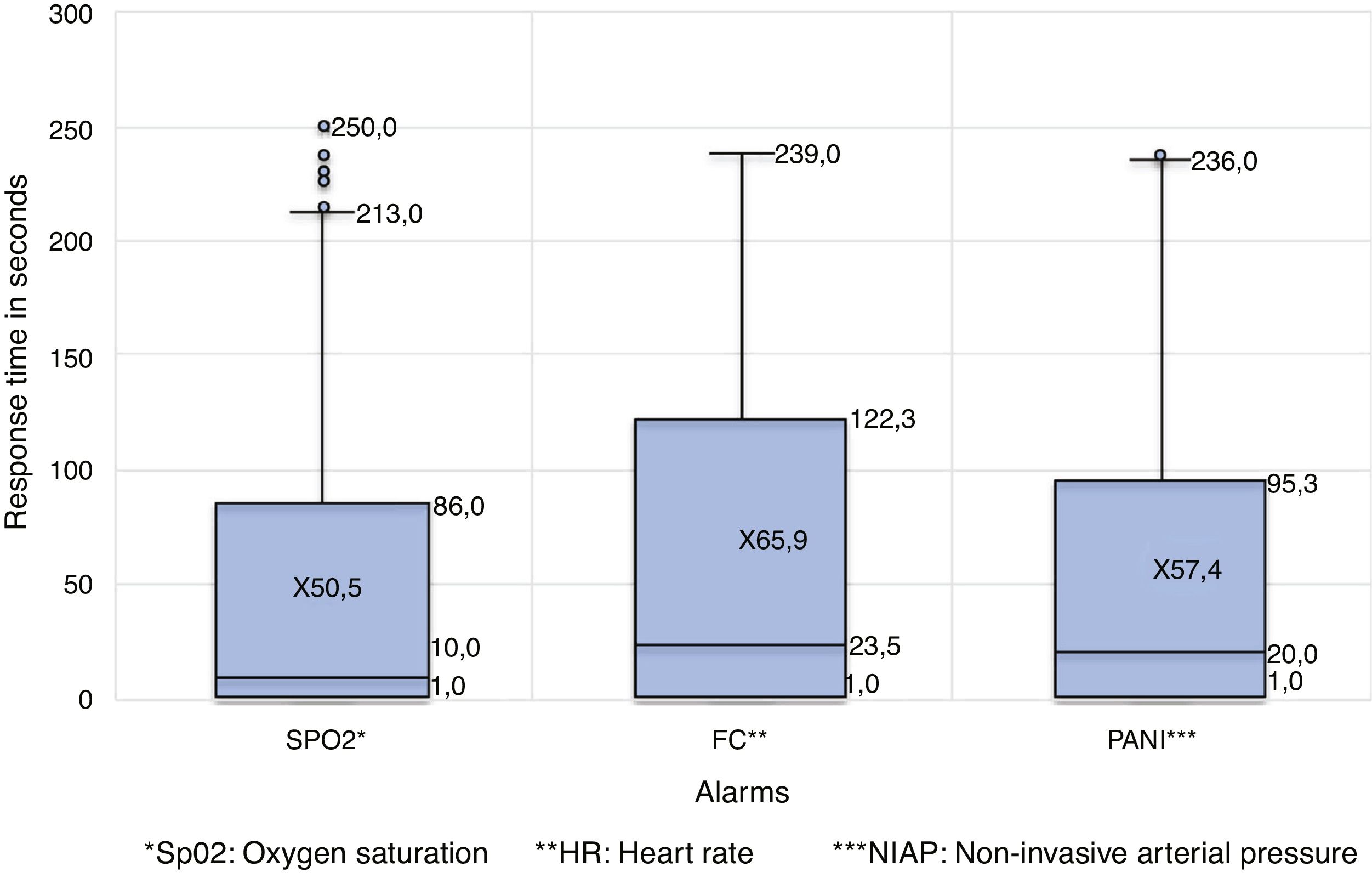
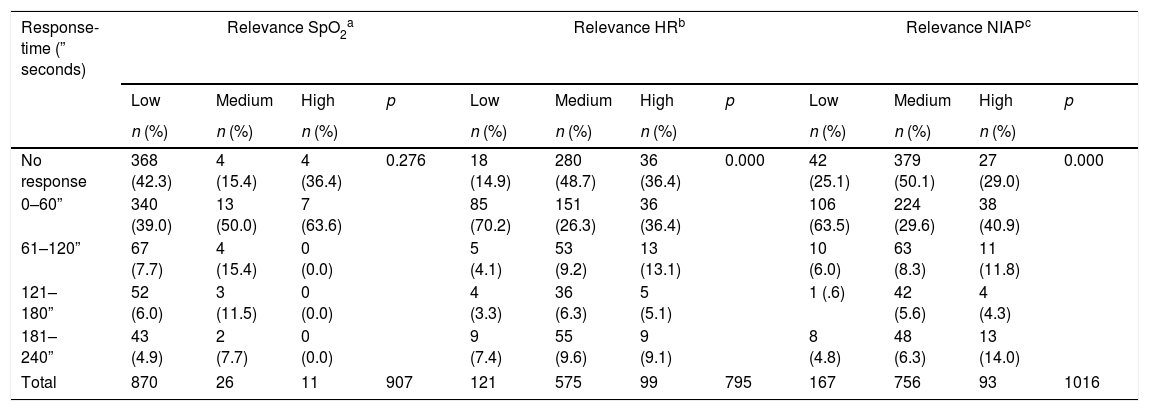
The stimulus-response time was taken as a continuous variable in seconds, but in the analysis it was stratified to determine the percentage of range in which the professionals reacted to the alarm, which ranged from 0 to 240s or from 0 to 4min in 57.2%. In turn, 42.6% of the cases did not receive a response from ICU health personnel, which is evidence of alarm fatigue. Fig. 1 details the response time according to the type of alarm (SpO2, HR and NIAP) and Table 1 shows the response time according to the relevance of the SpO2, HR and NIAP alarms.
Distribution of frequency and response time according to the clinical relevance of the alarms.
| Response-time (” seconds) | Relevance SpO2a | Relevance HRb | Relevance NIAPc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | p | Low | Medium | High | p | Low | Medium | High | p | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| No response | 368 (42.3) | 4 (15.4) | 4 (36.4) | 0.276 | 18 (14.9) | 280 (48.7) | 36 (36.4) | 0.000 | 42 (25.1) | 379 (50.1) | 27 (29.0) | 0.000 |
| 0–60” | 340 (39.0) | 13 (50.0) | 7 (63.6) | 85 (70.2) | 151 (26.3) | 36 (36.4) | 106 (63.5) | 224 (29.6) | 38 (40.9) | |||
| 61–120” | 67 (7.7) | 4 (15.4) | 0 (0.0) | 5 (4.1) | 53 (9.2) | 13 (13.1) | 10 (6.0) | 63 (8.3) | 11 (11.8) | |||
| 121–180” | 52 (6.0) | 3 (11.5) | 0 (0.0) | 4 (3.3) | 36 (6.3) | 5 (5.1) | 1 (.6) | 42 (5.6) | 4 (4.3) | |||
| 181–240” | 43 (4.9) | 2 (7.7) | 0 (0.0) | 9 (7.4) | 55 (9.6) | 9 (9.1) | 8 (4.8) | 48 (6.3) | 13 (14.0) | |||
| Total | 870 | 26 | 11 | 907 | 121 | 575 | 99 | 795 | 167 | 756 | 93 | 1016 |
Among the variables of response time and clinical relevance of the alarm, a statistically significant association was evidenced (p=0.000) in HR and BP. In 50.7% of the cases response was by one person, in 5% by two, in 0.6% by three and in 1.1% by four. Nursing assistants or technical staff were the most responsive to alarms (40.5%), followed by nurses 10.3%, therapists 8.9% and physicians 7.2%.
DiscussionIt is usual for alarms to sound continuously in an ICU; Wilken et al. in 201719 reported 150–350 alarms per day, of which 80% to 95% were not actionable; Drew et al.20 had similar findings, 187 per day. Solvoll et al. in Norway in 201721 recorded 2800 alarms in one week, while Bridi et al.4 recorded 5.3 alarms per hour in daytime service. In this study, there was alarm fatigue in 42.6%; Oliveira et al.22 found 66.03% with this condition. In 50% of the cases, between two and three alarms per patient sounded simultaneously, a result that is disturbing if we take into account that more than one alarm sounding at the same time may be a precipitating factor of adverse events in ICU.
McClure et al.,23 monitoring a neonatal ICU, found that 12% of the alarms were due to cardiovascular events and 80.5% to respiration or oxygenation-related readings; in our case, 70.7% corresponded to cardiovascular events and 29.2% to oxygen saturation. These results are consistent with the diseases with the highest incidence in both neonatal and adult ICUs.
Of the alarms heard in this study, 57.6% were of medium and high relevance, indicating the need for priority or immediate attention, while in the study by Johnson et al.24 this characteristic was present in between 1% and 36% of cases.
Both Oliveira et al.22 and the authors of this study found that those who responded most frequently to alarms belonged to the group of nurses, technicians and professionals; 31.06% in the first and 50.8% in the second; the other responses were from other members of the interdisciplinary team. The response time in this paper was between 0 and 240s or 4min for the SpO2, NIAP and HR parameters, defining criteria of alarm fatigue according to peer reviewer consensus, who took the resuscitation guidelines as the benchmark, which indicate that after 4min of cerebral hypoxia the damage is irreversible, i.e., between 0 and 4min, while Oliveira et al. identified between 8 and 10min for the same parameters, of great importance because they report high-impact haemodynamic changes and rapid negative progression in critically ill patients.
The scientific evidence confirms that alarm fatigue is a multicausal problem, evident and frequent in Intensive Care Units; it may be associated with inappropriate alarm settings, persistent atrial fibrillation and non-actionable events or events of little clinical value such as changes in central venous pressure and brief peaks in ST segments,20,25 as well as constant noise from different equipment, both medical and non-medical; all of which may generate desensitisation in health personnel.
There are measures to reduce the consequences of alarm fatigue, including reducing the repetition of several alarms in the same patient,26 minimising noise in ICUs,27 and decreasing the number of low severity alerts and medication alarms. It is also useful to instruct care staff on how and why alarms are generated.25
The high percentage of alarms with no response, most of them of medium and high clinical relevance, leads to alarm fatigue; a finding perhaps related to desensitisation in health care personnel by continuous exposure to these noises. This risk behaviour can compromise patient safety, even leading to fatal outcomes that affect quality of care.
ConclusionsThe results show the presence of alarm fatigue in the Multipurpose Adult ICU, a finding that can delay timely care or desensitise health personnel, which can jeopardise patient safety, even leading to fatal outcomes.
In most cases, the clinical relevance of the alarms was in the medium and low ranges.
In cases where health personnel responded, this was within the established terms to ensure timely and quality care.
Alarm fatigue must be promptly identified to implement interventions that mitigate the risks to which critically ill patients are exposed.
Limitations of the studyGiven the large number of alarms from ICU equipment that induce alarm fatigue, measuring the decibels of noise would have been interesting to take corrective action. We also consider it appropriate to extend this study to other units in the city and to carry out monitoring through video recording.
FundingThis research was directly funded by the investigators and forms part of the projects of the Cuidar research group of the Nursing Programme of the Universidad Surcolombiana.
Conflict of interestsThe authors have no conflict of interest to declare.
The authors express their gratitude to the participants in this study, care staff from the ICU-A of the Hospital Universitario Hernando Moncaleano Perdomo, who through their participation enabled the realisation of this research study and recognised the need to address the issue of alarms in ICU.
Please cite this article as: Andrade-Méndez B, Arias-Torres DO, Gómez-Tovar LO. Fatiga de alarmas en Unidad de Cuidados Intensivos: relevancia y tiempo de respuesta. Enferm Intensiva. 2020;31:147–153.