Delayed meconium expulsion is a cause of bowel obstruction in the extremely premature newborn (<28 WGE) weighing less than 1500g at birth.
ObjectiveTo evaluate the efficacy of conservative treatment in the prevention of meconium obstruction in very-low-birth-weight preterm infants.
MethodDescriptive and retrospective study performed at the Neonatal Intensive Care Unit of a tertiary level hospital. All very-low-birth-weight preterm infants who were born during the study period, from August 2016 to January 2017, and who had meconium obstruction were included.
ResultsA sample of 42 newborn infants was obtained. Regarding the expulsion of meconium, 57.1% of the sample spontaneously ejected meconium, while 42.9% received different treatments. Of these, 72.2% were treated with saline enemas, 16% with acetylcysteine enemas, 16% with Gastrografin® and none required surgical treatment.
ConclusionConservative treatment seems to be an effective therapeutic measure for the prevention of meconium obstruction in very-low-birth-weight preterm infants since it achieved the expulsion of meconium without having to apply surgical treatment.
El retraso en la expulsión de meconio es una causa de obstrucción intestinal en el recién nacido (RN) extremadamente prematuro (< 28 SEG) con un peso inferior a 1.500g al nacimiento.
ObjetivoEvaluar la eficacia del tratamiento conservador en la prevención de la obstrucción meconial en RN prematuros de muy bajo peso.
MétodoEstudio descriptivo y retrospectivo realizado en la Unidad de Cuidados Intensivos Neonatales de un hospital de nivel terciario. Se incluyó a todos los RN prematuros extremos de bajo peso que nacieron durante el periodo del estudio, desde agosto del 2016 hasta enero del 2017, y que presentaban obstrucción meconial.
ResultadosSe obtuvo una muestra de 42 RN. Respecto a la expulsión de meconio, un 57,1% de la muestra expulsó meconio de forma espontánea, mientras que un 42,9% recibió los diferentes tratamientos conservadores. De estos, un 72,2% fueron tratados con enemas de suero fisiológico. Del 27,8% restante, un 16% con enemas de N-acetilcisteína, 16% con Gastrografin® y ninguno precisó tratamiento quirúrgico.
ConclusiónEl tratamiento conservador parece ser una medida terapéutica efectiva para la prevención de la obstrucción meconial en los RN prematuros de muy bajo peso, ya que logró la expulsión de meconio sin tener que aplicar tratamiento quirúrgico.
Prematurity meconium obstruction is a functional bowel obstruction in extremely premature newborns (<28 WGA) with very low birth weight (<1.500g) caused by the inability to evacuate meconium. This is considered a different condition to meconium plug syndrome, its aetiology seems to be related to the combination of the high viscosity of meconium and the low motility of the premature bowel.
Early diagnosis based on clinical suspicion, exploration and the presence of a major perinatal risk factor, leads to the establishment of appropriate treatment, which reduces morbimortality of the newborn. Clinical features may be abdominal swelling, marked bowel loops on examination, delay in meconium expulsion, vomiting, enteral nutrition intolerance but without any signs of peritonitis. With regard to treatment, there is little available evidence and different lines of treatment are presented from conservative to surgical.
What does this paper contribute?This is a descriptive study, with just one centre and with a small sample. This research study suggests the effectiveness of early conservative treatment administration in line with a specifically designed protocol.
Treatment for preterm meconium obstruction is highly varied and there is little evidence. As a result this study is relevant and highlights the importance and safety of conservative treatment in the prevention of meconimum obstruction to achieve meconimum expulsion without the need for surgical treatment.
This study is the starting point for further research studies to demonstrate the effectiveness of conservative treatment, using a larger sample, and prolonged follow-up to analyse all possible complications and with the inclusion of several hospitals. It also contributes to generating greater scientific knowledge allowing us to offer better evidence-based care.
Implications of the studyThe most obvious implication for clinical practice is underlining the usefulness of nursing research, which leads to evidence-based, safe and quality care. This case is also an example of how a standardised and protocolised nursing procedure can advance the nursing profession in improving care. For the new protocols to be useful and to become established effectively professional nurses teaching and training is required.
Meconium obstruction in the very low birth weight infant is defined as a functional bowel obstruction in extremely premature newborns (NB) (<28 WGA) with a birth weight below 1500g secondary to the accumulation of thick meconium.1–4
Throughout history different terms have been used for meconium obstruction, but it was in 1986 when Amodio et al.5 described it for the first time as preterm microcolon. Later, in 2004, the term meconium obstruction in the very low birth weight infant2 came into use.
This clinical condition may also be called “meconimum obstruction syndrome”, “delayed meconimum expulsion syndrome” or “meconium syndrome”.2,4 Although this is a benign condition,6–8 it may lead to temporary meconium ileum and meconium obstruction syndrome,2 as well as serious complications such as necrosis or rupture.6–8
Aetiology appears to be related to the combination of excessively viscous meconium and low bowel motility due to the immaturity of the NB. It occurs in patients with risk factors, which mainly affect the small intestine.6–10
The detection of risk factors therefore helps to lead to early diagnosis and an appropriate treatment reducing morbimortality in newborns. These factors are: extreme preterm and low birthweight (<1500g) and perinatal comorbidity such as: small for their gestational age, maternal high blood pressure, preeclampsia/eclampsia, maternal diabetes, delay in intrauterine growth, placenta abruption, caesarian and prenatal magnesium sulphate leading to a depressive effect in the intestinal smooth muscle cells.6–8
Regarding clinical features, meconium obstruction in very low birth weight preterm infants may present asymptomatically, i.e. the majority of newborns present with a low quantity of meconium expulsions. If there are clinical signs they are abdominal swelling with marked bowel loops, and possibly presentation of vomiting or yellowish-green fluid. They characteristically present as “benign” with no signs of peritonitis.6–10
Clinical suspicion is highly important for diagnosis, as is examination and the presence of any perinatal risk factors. To this end, different diagnostic tests are used: plain X-ray (the dilated bowel loops are apparent), abdominal ultrasound scan (a dilated small bowel was observed filled with meconium) and enema of contrast medium (indicated with diagnostic and therapeutic intention which shows a dilation of the small bowel and a possible microcolon with filling defects). It is important to highlight that the blood test has little diagnostic power given that on the majority of occasions, no changes or alterations are observed.6–10
The treatment of this situation is highly varied and little evidence exists, and there no consensus has been reached about which is the best treatment. Its objective is to evacuate the accumulation of meconium by stimulating the peristalsis or reducing viscosity.3 Treatment may be conservative, such as physiological or glycerine serum enemas, or surgical, which is used when there is persistent obstruction or the presentation of bowel perforation.1,2,6–8
In different systematic reviews there is no evidence regarding any preventative treatment. In the clinical trials included in these, glycerine suppositories are used, and osmotic contrast and physiological enemas. Even so, evidence is such that early treatment may reduce complications.6,7,11–14
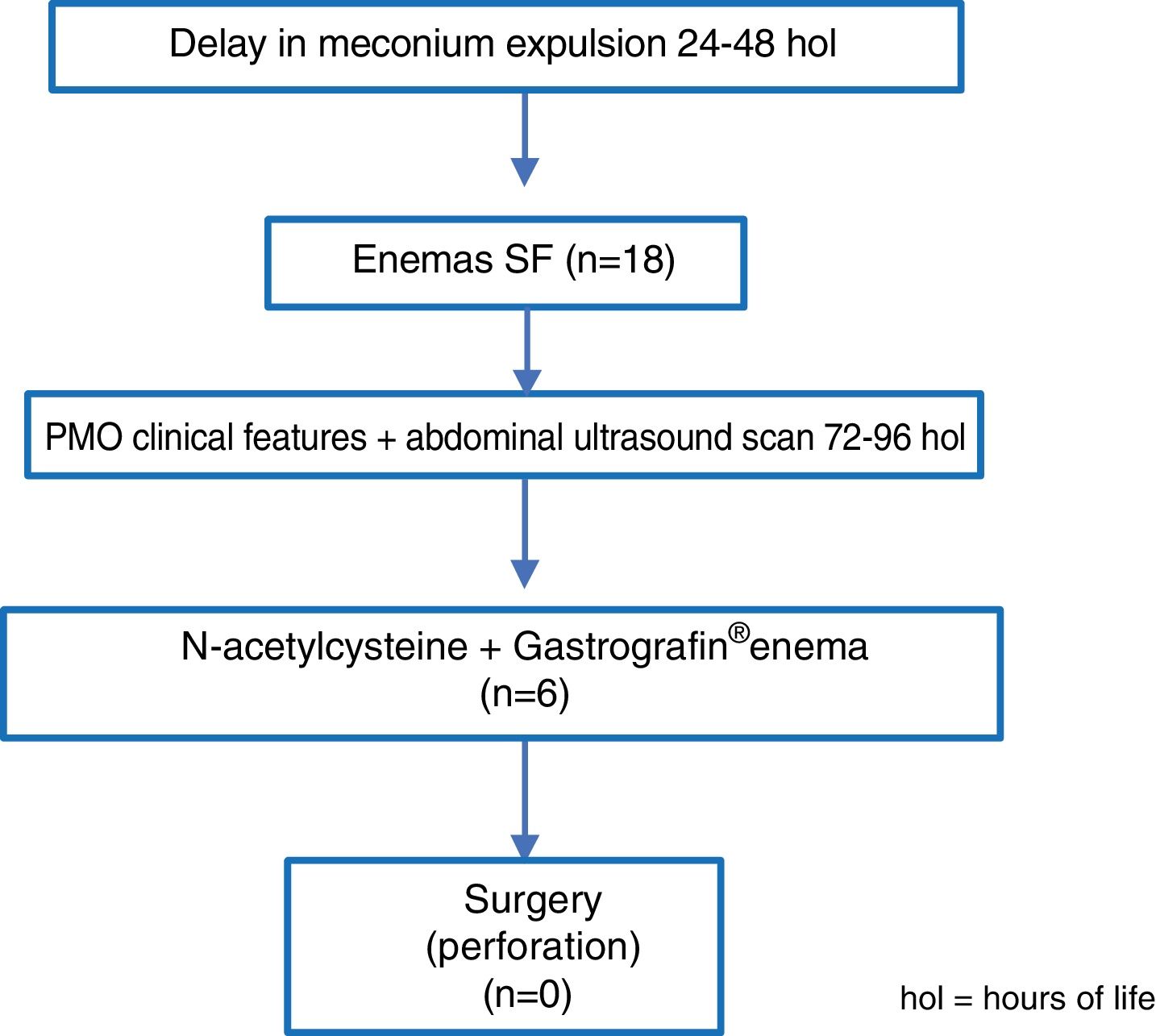
Derived from this, it was decided to protocolise preterm patient care when there was a risk of PMO. To do this a standardized protocol was designed in the Neonatal Unit of this hospital. “The treatment used” according to the protocol of the study consists in: firstly, initiating conservative treatment. If after 24–48h of life meconium has not been evacuated or it was scarce, physiological serum enemas of 5–10ml/kg will be administered every 12h for 48h. After 3–4 days, when there is suspicion of meconium obstruction in very low birth weight preterm infants, abdominal ultrasound scan will be requested. If signs of this condition are confirmed, N-acetylcysteine enemas of by gastric tube of 1–5ml to 10% every 6h and Gastrografin® enemas diluted to a third with physiological saline solution guided by ultrasound will be administered. To do this the tube will be inserted as high as possible without force and the contrast will be administered. It is therefore important to exhaustively monitor the NB for risk of perforation due to the increase of bowel pressure. The procedure may be repeated every 24–48h and up to 4 or 5 attempts will be made depending on the patient's clinical condition.6–10
Surgical treatment will be carried out on all patients who present with bowel perforation or when conservative treatment has not been effective.6–10
The main objective of the study was to assess the effectiveness of the early application of conservative treatment in the prevention of PMO in low weight preterm newborns (<1500g). The specific objectives were to assess the efficacy of the different lines of conservative treatment and to analyse the appearance of complications in conservative treatment.
MethodThis was a descriptive and retrospective research study. Firstly, a review of the scientific literature was made with a bibliographical search during June and July 2016 to become familiar with the current state of the meconium obstruction and design the theoretical framework of the investigation. The data bases consulted were: PubMed, Cuiden, Lilacs, Cochrane, Cuidatge and SciELO. For the search we used the following descriptors in Health Sciences: “bowel obstruction”; “meconium”, “newborn”, and “nurses” and for those of the Medical Subject Headings (MeSH): intestinal obstruction; meconium; infant, newborn; enema y nurses. The boolean operators used were “AND” and “OR”.
Once the relevant consent forms had been obtained from the hospital and with the approval of the chief of service and supervisor, recruitment of the NB was initiated, from the month of August 2016 to January 2017. Data was also obtained from the same period of the previous year (2015–2016), i.e. prior to the imitation of conservative treatment according to the protocol. Firstly, the parents were informed about the option to participate in the study and once informed consent had been obtained, the data were included for posterior review. Once the recruited newborns had been selected, review of the clinical file was obtained to collect data and incorporate them into the data bases created in IBM SPSS Statistics V.20 for subsequent statistical analysis.
The study environment was a tertiary level Neonatal Intensive Care Unit, and the total number of patients admitted there in 2016 was 365. The target population were extremely premature newborns, under 28 WGA and with very low birth weight (<1500g), which are those with the highest risk of obstruction due to gastrointestinal immaturity. For sample selection the following inclusion criteria were established:
- –
Extreme premature newborns (<28 WGA).
- –
Newborns with very low birth weight (<1500g).
- –
Admitted to the Neonatal Intensive Care Unit.
- –
Prior obtainment of informed consent.
And as exclusion criteria:
- –
Newborn with bowel malformations.
- –
Death.
The treatment used in the newborns diagnosed with meconium obstruction in very low birth weight preterm infants was that established in the protocol of the previously commented upon unit.
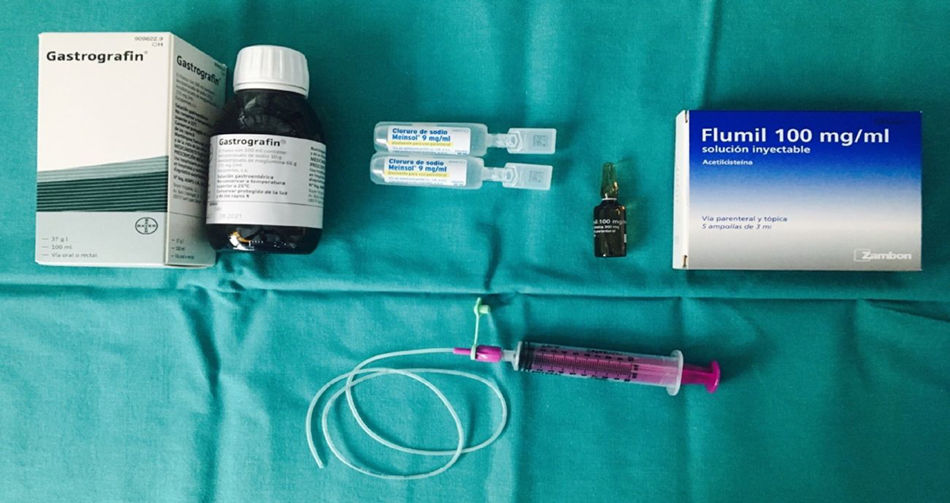
The material used during the study was: .9% physiological serum, enteral feeding tube 4Fr and 6Fr, vaseline, 10ml syringe, N-acetylcysteine, ultrasound scan and Gastrografin® (Fig. 1).
Data analysis was performed with the IBM SPSSS® V. 20 statistical package. Descriptive statistical tests were used, such as central positioning and dispersion measures. For quantitative variables the mean and standard deviation were calculated whilst for qualitative variables frequencies and percentages were presented. Bivariate analysis was then performed, using the Student's t-test for 2 quantitative variables and the Chi-square test, as for qualitative variables and the Pearson correlation for qualitative and quantitative variables.
ResultsIn the period from August 2015 to January 2016, prior to the establishment of the protocol, 99 preterm newborns with a birth weight under 1500g were born. Out of these, 6 were diagnosed with PMO, amounting to 5% of the total. Out of these 6 NB, 4 presented with the complication of perforation, which accounted for 66.7% and finally the 6 of them underwent surgery to treat the PMO, corresponding to 100% of surgical interventions.
During the same period of the years 2016 to 2017, 42 preterm newborns with a weight under 1500g were born, of whom 18 were diagnosed with PMO which was 42.9% of the total.
With regard to clinical characteristics and demographics of the total of those included in the 2016–2017 period, 42.2% of them were female and 57.8% male, with a mean weight of 1042±245g and a mean WGA of 27.7±2.7.
With regard to the different treatments used, the 18 NB diagnosed with PMO and included in the 2016–2017 period were treated with physiological serum enemas. Out of all of these, 12 NB expulsed the meconium and the obstruction was resolved, which led to success in meconium evacuation of 66.7%. The 6 patients for whom the physiological serum enema was not effective, were administered N-acetylcystein through an orogastric tube and ultrasound guided Gastrografin® enemas, which were effective in the 6 NB, with treatment success thus reaching 100%. None of the NB with PMO therefore had to undergo surgery (Fig. 2).
No complications arose relating to the conservative treatment nor were any bowel perforations observed in the NB.
When comparing the results obtained previously to the application of the protocol and posterior results, a statistically significant difference was observed in the complications (p=.01), which was 66.7% in the previous ones and 0% in the posterior ones. Furthermore, when comparing surgical interventions a significant difference was also observed (p=.001), since prior to the protocol 100% of the NB underwent surgery and in subsequent years this was 0%.
DiscussionDifferential diagnosis between a PMO and a delay in normal meconium evacuation15 is complex since the latter is common in preterm newborns who usually evacuate the meconium between the second and fifth day of life.16 In fact, out of the total of preterm newborns included in the study, 93 (2015–2016) and 24 (2016–2017) expulsed meconium spontaneously within the first 3 days, and possible PMO was therefore rejected, whilst 6 (2015–2016) and 19 (2016–2017) were finally diagnosed with meconium obstruction. This shows that although the incidence of PMO has not yet been established, its diagnosis is increasing.3,6–8,17
Suspicion of obstruction exists when there is a delay in meconium expulsion and abdominal swelling,6–8 with the latter being one of the initial symptoms.18 When associated risk factors are also involved early detection may be made and treatment initiated.6–8 This will enable us to avoid possible complications, such as persistent obstruction, intestinal ischemia (due to increase in intraluminal pressure)17 or bowel perforation which therefore lead to surgery.15 In this study, preventative measure such as rectal stimulation with physiological saline solution after birth helps to prevent PMO,15 and is the first line treatment carried out both in the Unit of this study context6–8 and the study of Kim et al.19 However, studies such as that of Hatanaka et al.20 and Arnoldi et al.21 do not use this as first line treatment, as determined by their protocols. Efficacy of rectal stimulation with physiological saline solution was observed, since according to our study of the 18 very low birth weight preterm newborns who received it an effect was noted in 12 (66.7%) and in the Kim et al.19 study, of the 22 who received it beneficial effects were noted in 5 (22.7%).
In some NB very low in weight, this rectal stimulation was ineffective and did not lead to complete evacuation,15 and as a result in this case, following the unit protocol, in the 6 preterm very low weight newborns where no beneficial effect was noted rectal stimulation with N-acetylcysteine was made and had positive effects in all of them. This second line treatment was also used in the Arnoldi et al.21 study as first line, with beneficial results in 100% of cases, whilst in the Kim et al.19 study it was used as third line and administration was oral.
Finally it is important to underline that several authors9,18–20 consider the administration of a Gastrografin® enema as the best treatment for PMO, which when administered early increases the success rate and reduces the cases of very low birth weight NB who require surgery. It also reduces morbimortality. However, these statements contrast with studies like that of Copeland et al.,3 who observed a reduction in enema with contrast success to relieve meconium in the ileum. In our study 6 very low birth weight preterm newborns (33.3%) required an enema with Gastrografin®, and this had a positive effect on them all. Conservative treatment was therefore successful and no surgical intervention was required.
It is also true that some studies have reported incidences in both gastric tube N-acetylcysteine administration because it may lead to hypernatremia, hipovolemia and mucosa ulceración,1 and in the enema with Gastrografin®, which may cause bowel perforation due to the increase in intraabdominal pressure. 18,22 According to the Copeland et al.22 study, Gastrografin® also increases any risk of hypovolemic shock, inflammation and ischemic enterocolitis. In this study22 bowel perforation was observed in 2.7% of the very low weight newborns, in the study by Cho et al.17 9.1% were recorded whilst in our study this did not occur in any of the preterm NB.
Since treatment exists without any fixed established guidelines and is therefore highly varied, further studies are needed where early diagnosis would play a key role in preventing the development of the condition and its exacerbation. Moreover, randomized clinical trials are essential to demonstrate the efficacy of different lines of treatment so that the possible presentation of complications may be minimized, since the different lines of treatment are not exempt from adverse effects.
With regard to the limitations of this research study, we would state that the sample used in the study is small, with the possibility that a difference in the treatment was not recorded, and it would therefore be useful to increase it in future lines of research. To this limitation we would add the fact that the study was in a single centre and we would recommend conducting multicentre studies to recruit larger population groups.
ConclusionsConservative treatment in NB analysed in this study was effective in the prevention of meconium obstruction in very-low-birth-weight infants. The increase in diagnosis of these patients means that conservative treatment may be initiated earlier and this could have an impact on increasing success rates. The different lines of treatment were effective for reducing complications and surgical interventions. This has improved the healthcare and safety of the preterm newborns.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Solaz-García AJ, Segovia-Navarro L, Rodríguez de Dios-Benlloch JL, Benavent-Taengua L, Castilla-Rodríguez DY, Company-Morenza MA. Prevención de la obstrucción meconial en recién nacidos prematuros de muy bajo peso. Enferm Intensiva. 2019;30:72–77.