Patients in intensive care unit are susceptible to complications due to different causes (underlying disease, immobilisation, infection risk…). The current main intervention in order to prevent these complications is respiratory physiotherapy, a common practice for nurses on a daily basis. Therefore, we decided to carry out this bibliographic review to describe the most efficient respiratory physiotherapy methods for the prevention and treatment of lung complications in patients in intensive care, taking into account the differences between intubated and non-intubated patients.
MethodologyThe bibliographic narrative review was carried out on literature available in Pubmed, Cinahl and Cochrane Library. The established limits were language, evidence over the last 15 years and age.
ResultsTechniques involving lung expansion, cough, vibration, percussion, postural drainage, incentive inspirometry and oscillatory and non-oscillatory systems are controversial regarding their efficacy as respiratory physiotherapy methods. However, non-invasive mechanical ventilation shows clear benefits. In the case of intubated patients, manual hyperinflation and secretion aspirations are highly efficient methods for the prevention of the potential complications mentioned above. In this case, other RP methods showed no clear efficiency when used individually.
Discussion and conclusionsNon-invasive mechanical ventilation (for non-intubated patients) and manual hyperinflation (for intubated patients) proved to be the respiratory physiotherapy methods with the best results. The other techniques are more controversial and the results are not so clear. In both types of patients this literature review suggests that combined therapy is the most efficient.
Los pacientes ingresados en unidades de cuidados intensivos son susceptibles de complicaciones pulmonares por múltiples causas (enfermedad de base, inmovilización, riesgo de infección, etc.). La principal intervención para prevenirlas y tratarlas es la fisioterapia respiratoria (FR), práctica habitual en el día a día de enfermería. Por ello se realizó esta revisión bibliográfica, con el objetivo de describir los métodos de FR más eficaces para la prevención y tratamiento de las complicaciones pulmonares en los pacientes ingresados en unidades de cuidados intensivos, diferenciando paciente intubado y no intubado.
MetodologíaSe llevó a cabo una revisión narrativa de la literatura en las bases de datos Pubmed, Cinahl y Cochrane Library. Los límites fueron el idioma, la evidencia de los últimos 15 años y la edad.
ResultadosLas técnicas de expansión pulmonar, tos, vibración, percusión, drenaje postural, espirometría incentivada y los sistemas oscilatorios y no oscilatorios presentan controversia en cuanto a la eficacia como método de fisioterapia respiratoria. En cambio, la ventilación mecánica no invasiva muestra clara evidencia de su beneficio. En el paciente intubado, la hiperinsuflación manual y la aspiración de secreciones son métodos eficaces para la prevención de complicaciones respiratorias. El resto de métodos de FR aplicados de forma aislada no han demostrado una clara eficacia.
Discusión y conclusionesLas técnicas de FR que han demostrado mejores resultados son la ventilación mecánica no invasiva para el paciente no intubado y la hiperinsuflación manual para el paciente intubado. Respecto al resto de técnicas existe mayor controversia. En ambos grupos de pacientes, la literatura muestra que la terapia combinada es la más eficaz.
Patients admitted to intensive care units are susceptible to pulmonary complications of multiple causes (baseline disease, immobilisation, risk of infection, etc.). Respiratory physiotherapy is the main intervention used to prevent and treat these complications. Although routine practice in intensive care, there is controversy regarding the efficacy of the different techniques.
The aim of this review was to establish the different respiratory physiotherapy techniques and their efficacy for both intubated and non-intubated patients in intensive care units, and to select the most beneficial techniques.
Implications of the studyKnowledge of the different respiratory physiotherapy exercises will enable a care plan to be designed and record the most beneficial techniques tailored to each patient.
Understanding the benefits of the different exercises will enable us to examine their importance and their impact on the critical patient; multidisciplinary teams and postgraduate students will require training.
Further studies are recommended to examine the exercises that are controversial in the literature.
It is usual for patients following cardiovascular, thoracic or abdominal surgery, as well as patients with acute processes including sepsis or respiratory failure to be admitted to intensive care units (ICU). All of these patients can develop impaired oxygenation and/or ventilation.1–6 In addition, they are susceptible to respiratory complications due to their baseline disease, immobility and nosocomial infections.7,8 The most common complications are atelectasis, pneumonia, pleural effusion and tracheobronchial infection,9–14 pneumonia being the main cause of mortality.10,11,15,16 These complications are due to shallow breathing, increased secretions and reduced pulmonary compliance, and to changes in muscle tone and to the lung parenchyma.2,3,5,7,11,13,17–19 Other factors, such as pain, residual anaesthetic effects20 and prolonged bedrest,8,21 contribute to their development.1,2,11 Very varied percentages were found (2%–88%) with regard to incidence of complications in postsurgical patients.2,9,11 In intubated patients, 12 episodes of pneumonia per 1000 days of mechanical ventilation have been recorded.22 These complications have high rates of morbidity and mortality, increased hospitalisation rates and longer hospital stays.2,3,5,9,13–15,20,21,23–25
Respiratory physiotherapy plays an essential role3,5,9,26 in preventing or minimising all of these lung complications in ICU.8,23,27 RP is part of respiratory rehabilitation,28,29 a multidisciplinary intervention that also encompasses assessment of the patient, muscle exercise, education, dietary intervention and psychosocial support.28–31 Because it requires prolonged application, and the patient's stay in ICU is sometimes shorter than the duration of the complete programme, it can be impossible to complete. Therefore, this study focuses exclusively on RP. RP includes a series of techniques with the general aim of improving regional ventilation, mucociliary clearance, gas exchange, respiratory muscle function, dyspnoea, tolerance to exercise and health-related quality of life.28–30,32
Although routine practice in ICU, there is controversy as to the efficacy of the various techniques.26,33 We conducted this literature review to describe the most effective RP methods for the prevention and treatment of pulmonary complications in patients admitted to ICU, differentiating spontaneously breathing patients from intubated patients, undergoing invasive mechanical ventilation (IMV). In this paper we considered spontaneously breathing patients to be those able to breathe by themselves and not through an artificial airway.
MethodologyTo meet our objective, we performed a narrative literature review from January to August 2016, in the Pubmed, Cinahl y Cochrane Library databases. We also reviewed the websites of the leading scientific societies (Spanish Society of Pneumology and Thoracic Surgery, American Association for Respiratory Care, European Respiratory Society Statement on Pulmonary Rehabilitation) and performed manual searches of various relevant journals in the area of respiratory therapy: Respiratory Care, Critical Care Nurse, Enfermería Intensiva. We also reviewed the reference lists of the selected articles, to check for studies of interest (snowball technique). These searches were limited by language (English and Spanish, year of publication (last 15 years) and age (people >18 years of age).
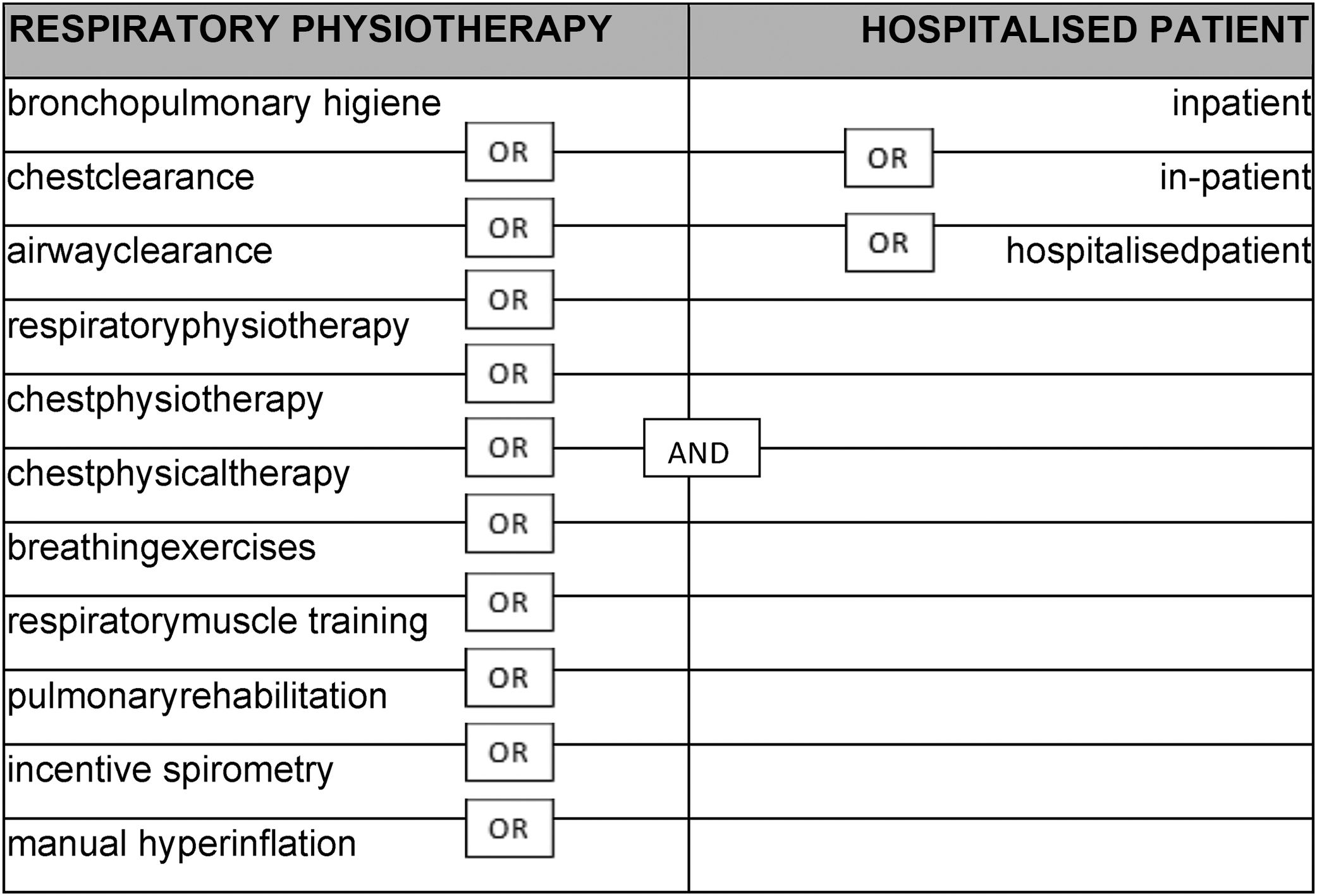
The terms used and their combination with the Boolean operators are shown in Table 1. Initially the term ICU was included in the search, but because of the few articles we found, most of which concerned intubated patients, we decided to exclude it and conduct a wider search.
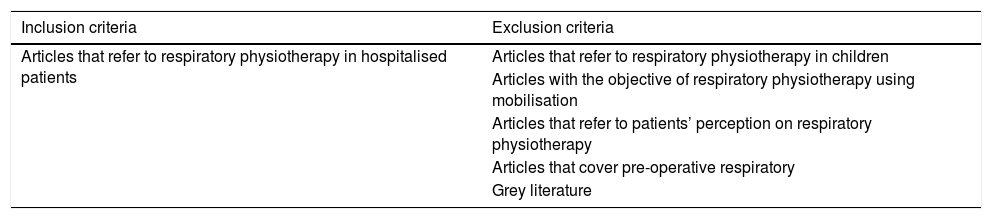
The articles were selected according to the inclusion and exclusion criteria defined in Table 2.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Articles that refer to respiratory physiotherapy in hospitalised patients | Articles that refer to respiratory physiotherapy in children |
| Articles with the objective of respiratory physiotherapy using mobilisation | |
| Articles that refer to patients’ perception on respiratory physiotherapy | |
| Articles that cover pre-operative respiratory | |
| Grey literature |
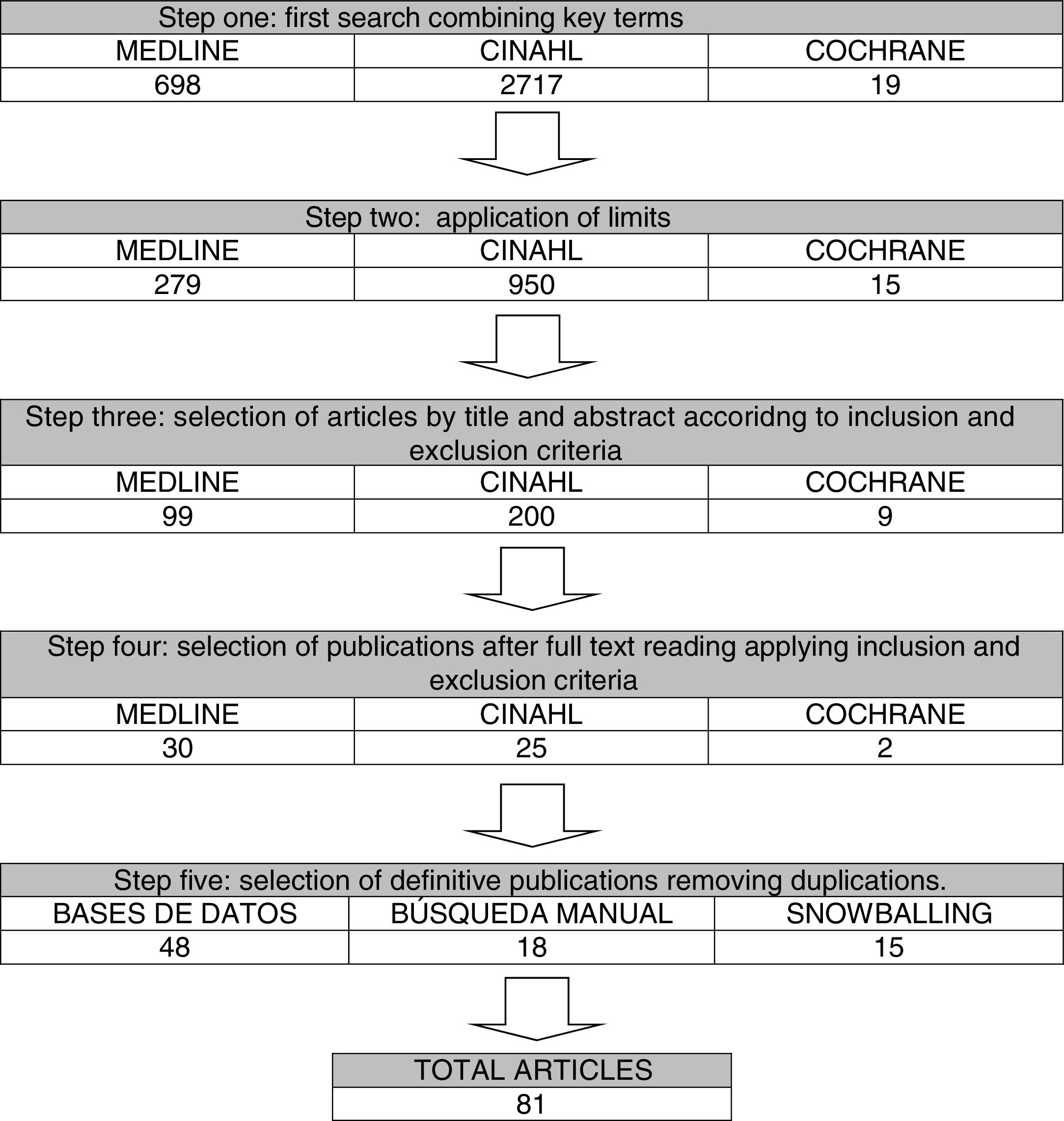
The flow of articles is described in Fig. 1.
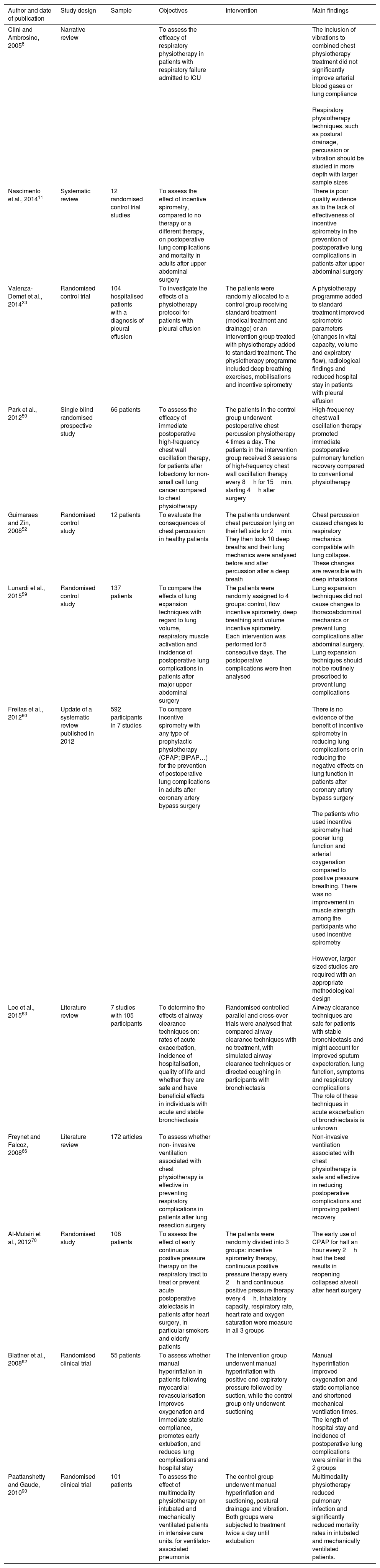
ResultsThe results were classified into 2 groups: (a) RP exercises for spontaneously breathing patients and (b) RP exercises for patients undergoing IMV. We first described each of the techniques, and then outlined the advantages and disadvantages found in the articles we reviewed. Table 3 shows the most relevant articles on the different exercises described.
The most relevant articles in the study.
| Author and date of publication | Study design | Sample | Objectives | Intervention | Main findings |
|---|---|---|---|---|---|
| Clini and Ambrosino, 20058 | Narrative review | To assess the efficacy of respiratory physiotherapy in patients with respiratory failure admitted to ICU | The inclusion of vibrations to combined chest physiotherapy treatment did not significantly improve arterial blood gases or lung compliance Respiratory physiotherapy techniques, such as postural drainage, percussion or vibration should be studied in more depth with larger sample sizes | ||
| Nascimento et al., 201411 | Systematic review | 12 randomised control trial studies | To assess the effect of incentive spirometry, compared to no therapy or a different therapy, on postoperative lung complications and mortality in adults after upper abdominal surgery | There is poor quality evidence as to the lack of effectiveness of incentive spirometry in the prevention of postoperative lung complications in patients after upper abdominal surgery | |
| Valenza-Demet et al., 201423 | Randomised control trial | 104 hospitalised patients with a diagnosis of pleural effusion | To investigate the effects of a physiotherapy protocol for patients with pleural effusion | The patients were randomly allocated to a control group receiving standard treatment (medical treatment and drainage) or an intervention group treated with physiotherapy added to standard treatment. The physiotherapy programme included deep breathing exercises, mobilisations and incentive spirometry | A physiotherapy programme added to standard treatment improved spirometric parameters (changes in vital capacity, volume and expiratory flow), radiological findings and reduced hospital stay in patients with pleural effusion |
| Park et al., 201250 | Single blind randomised prospective study | 66 patients | To assess the efficacy of immediate postoperative high-frequency chest wall oscillation therapy, for patients after lobectomy for non-small cell lung cancer compared to chest physiotherapy | The patients in the control group underwent postoperative chest percussion physiotherapy 4 times a day. The patients in the intervention group received 3 sessions of high-frequency chest wall oscillation therapy every 8h for 15min, starting 4h after surgery | High-frequency chest wall oscillation therapy promoted immediate postoperative pulmonary function recovery compared to conventional physiotherapy |
| Guimaraes and Zin, 200852 | Randomised control study | 12 patients | To evaluate the consequences of chest percussion in healthy patients | The patients underwent chest percussion lying on their left side for 2min. They then took 10 deep breaths and their lung mechanics were analysed before and after percussion after a deep breath | Chest percussion caused changes to respiratory mechanics compatible with lung collapse. These changes are reversible with deep inhalations |
| Lunardi et al., 201559 | Randomised control study | 137 patients | To compare the effects of lung expansion techniques with regard to lung volume, respiratory muscle activation and incidence of postoperative lung complications in patients after major upper abdominal surgery | The patients were randomly assigned to 4 groups: control, flow incentive spirometry, deep breathing and volume incentive spirometry. Each intervention was performed for 5 consecutive days. The postoperative complications were then analysed | Lung expansion techniques did not cause changes to thoracoabdominal mechanics or prevent lung complications after abdominal surgery. Lung expansion techniques should not be routinely prescribed to prevent lung complications |
| Freitas et al., 201260 | Update of a systematic review published in 2012 | 592 participants in 7 studies | To compare incentive spirometry with any type of prophylactic physiotherapy (CPAP; BIPAP…) for the prevention of postoperative lung complications in adults after coronary artery bypass surgery | There is no evidence of the benefit of incentive spirometry in reducing lung complications or in reducing the negative effects on lung function in patients after coronary artery bypass surgery The patients who used incentive spirometry had poorer lung function and arterial oxygenation compared to positive pressure breathing. There was no improvement in muscle strength among the participants who used incentive spirometry However, larger sized studies are required with an appropriate methodological design | |
| Lee et al., 201563 | Literature review | 7 studies with 105 participants | To determine the effects of airway clearance techniques on: rates of acute exacerbation, incidence of hospitalisation, quality of life and whether they are safe and have beneficial effects in individuals with acute and stable bronchiectasis | Randomised controlled parallel and cross-over trials were analysed that compared airway clearance techniques with no treatment, with simulated airway clearance techniques or directed coughing in participants with bronchiectasis | Airway clearance techniques are safe for patients with stable bronchiectasis and might account for improved sputum expectoration, lung function, symptoms and respiratory complications The role of these techniques in acute exacerbation of bronchiectasis is unknown |
| Freynet and Falcoz, 200866 | Literature review | 172 articles | To assess whether non- invasive ventilation associated with chest physiotherapy is effective in preventing respiratory complications in patients after lung resection surgery | Non-invasive ventilation associated with chest physiotherapy is safe and effective in reducing postoperative complications and improving patient recovery | |
| Al-Mutairi et al., 201270 | Randomised study | 108 patients | To assess the effect of early continuous positive pressure therapy on the respiratory tract to treat or prevent acute postoperative atelectasis in patients after heart surgery, in particular smokers and elderly patients | The patients were randomly divided into 3 groups: incentive spirometry therapy, continuous positive pressure therapy every 2h and continuous positive pressure therapy every 4h. Inhalatory capacity, respiratory rate, heart rate and oxygen saturation were measure in all 3 groups | The early use of CPAP for half an hour every 2h had the best results in reopening collapsed alveoli after heart surgery |
| Blattner et al., 200882 | Randomised clinical trial | 55 patients | To assess whether manual hyperinflation in patients following myocardial revascularisation improves oxygenation and immediate static compliance, promotes early extubation, and reduces lung complications and hospital stay | The intervention group underwent manual hyperinflation with positive end-expiratory pressure followed by suction, while the control group only underwent suctioning | Manual hyperinflation improved oxygenation and static compliance and shortened mechanical ventilation times. The length of hospital stay and incidence of postoperative lung complications were similar in the 2 groups |
| Paattanshetty and Gaude, 201090 | Randomised clinical trial | 101 patients | To assess the effect of multimodality physiotherapy on intubated and mechanically ventilated patients in intensive care units, for ventilator-associated pneumonia | The control group underwent manual hyperinflation and suctioning, postural drainage and vibration. Both groups were subjected to treatment twice a day until extubation | Multimodality physiotherapy reduced pulmonary infection and significantly reduced mortality rates in intubated and mechanically ventilated patients. |
We found different RP methods in the literature such as lung expansion techniques, coughing, vibration, percussion, postural drainage, incentive inspirometry (IS), oscillatory and non-oscillatory devices and non-invasive mechanical ventilation (NIMV). We shall go on to describe each technique.
Lung expansion techniquesLung expansion techniques are used to promote breathing that enables active deep inhalation, with apnoea before passive exhaling. They include maximal inhalation, fractional inhalations with apnoea, diaphragmatic and pursed lip breathing.34 They are used to reexpand the lung tissue and encourage movement of secretions.23,35,36
Some authors also argue that they can be useful in increasing exercise capacity,37,38 vital capacity,39,40 inhalatory muscle strength,39–41 reducing dyspnoea37,38,40 and improving the quality of life39,41of individuals with weakened musculature. Other authors claim that pursed lip exercises42,43 and diaphragmatic breathing42 alleviate dyspnoea for patients with COPD. Similarly, Sutbeyaz et al.44 and Kyo Chul et al.45 describe benefits in patients with brain damage. In all cases, the results obtained were a consequence of a lengthy programme.
However, in the literature we reviewed these techniques were not found to provide benefits,8 although they might be useful in addition to exercising the body.34,37
CoughingDefined as a natural defence mechanism to remove foreign bodies and excess secretions as a result of disease processes from the airway. Coughing can be voluntary and involuntary.46,47 In situations where coughing is ineffective, there are various techniques to improve results such as manually assisted cough or the mechanical insufflator-exsufflator.7,47
Gosselink et al., 33 in 2008, stated that coughing is effective in increasing expiratory flow velocity, adequate inhalatory volume being necessary for it to be effective in eliminating secretions. In contrast, De Chamoy and Eales48 found that coughing, along with other activities, has no benefits in patients who have undergone heart valve surgery.
VibrationThis is the application of an oscillatory effect on the thoracopulmonary apparatus that can be transmitted to the airways to encourage the transport and elimination of bronchial secretions.8 Vibration can be performed externally manually during the expiratory phase,8 or mechanically using a vibration device.46,49
In the literature review we found only one article justifying mechanical vibration. Park et al.50 showed that applying vibration using a device on lobectomised patients improved lung function and arterial oxygenation.
We found no articles that justified or rejected the use of this manual technique in isolation.
PercussionPercussion aims to provoke oscillation in the thoracic wall, which is transmitted to the lungs and the airways, and generates loosening and movement of secretions.8 Percussion can be performed manually by striking the thoracic wall over the affected area of the lung or using mechanical devices.49 Martí et al.46 highlight that performing the manoeuvre manually does not achieve the necessary frequency (15–25Hz) to achieve the desired effect.
The available evidence is controversial and limited. Some studies have shown some increase in mucociliary transport during the percussion exercise,49 but without demonstrating a better effect than that of other techniques. A systematic review claims that use of this technique is insufficient.51 Furthermore, adverse effects have been described, such as pulmonary collapse and/or pneumoconstriction.52
Postural drainagePostural drainage encourages the transport of secretions inside the bronchial tree due to the action generated by the force of gravity. To achieve this, the bronchial segment to be drained must be angled as vertically as possible, putting the patient into different positions.46,49
Bellone et al.53 state that postural drainage is safe and effective in eliminating secretions without causing undesirable effects on oxygen saturation. Other studies,8,49 claim that its use in ICU optimises oxygen transport, improves ventilation/perfusion, increases lung volume, reducing effort of breathing, minimising the effort of the heart, and encouraging mucociliary clearance. However, bearing in mind the features of patients in ICU, often the complications of postural drainage limit its application.36,46,49 Moreover, Button and Boucher54 have demonstrated that to facilitate mucociliary transport mechanically flow and pressure variations must be created inside the bronchial tree, and the effect of the force of gravity should not be sought.
Incentive spirometryThis is a device that encourages maximum sustained inhalation to increase lung expansion,23 globally used as prophylaxis and to treat respiratory complications.3,5,6,11,20,35
In terms of positive effects, some authors claim that it is useful in reexpanding alveoli and reversing postoperative hypoxaemia.11 It increases inhalatory volume, enabling uniform ventilation during the start of inhalation,18 and transpulmonary pressure and inhalatory muscle function.55 In addition, it improves dyspnoea, arterial gasometry and the perception of health-related quality in patients with COPD, without producing changes in the parameters of lung function.55 Various authors vouch for its use in patients who have undergone abdominal surgery,6,20,56 heart surgery3,18,57 and tracheotomised patients.1 It reduces lung collapse and prevents infections,20,56 improves exercise tolerance,3 and improves the respiratory muscles compared to intermittent positive pressure.18
We should take into account that the efficacy of IS will depend on whether the patient has received correct instructions and has been adequately supervised by the nurse when performing the technique.3
Despite its widespread use and the benefits described, the evidence to support its efficacy remains controversial.2,5,6,58,59 The review by Carvalho et al.2 finds no statistically significant differences between applying IS treatment and not giving any RP treatment for respiratory complications in patients after heart, thoracic or abdominal surgery. This claim is reinforced by Do Nascimento et al.,11 Guimarães et al.,4 Gosselink et al.58 and Lunardi et al.59 who show the same results in patients after abdominal and thoracic surgery respectively. Various authors conclude that IS offers no advantages compared to coughing,60 breathing exercises11,19,35,60 or NIMV.2,60 However, Agostini et al.35 report that for patients at risk (>75 years, ASA>3, COPD,smokers, BMI>30), after thoracic surgery, this technique has more benefits in preventing lung complications than conventional RP.
Non-oscillatory and oscillatory devicesNon-oscillatory devices, such as intermittent positive expiratory pressure systems improve postoperative lung function through deep, wide and maintained breathing with a view to improving airway clearance.10,30,46
Roth et al.61 indicate that breathing exercises with exhalation resistance have positive effects on total lung capacity in people with tetraplegia, thus reducing respiratory morbidity and improving outcomes. Darbee et al.62 in 2004 obtained the same results in patients with cystic fibrosis.
However, the literature review by Rodriguez et al.9 in 2014 showed no statistically significant differences between patients who performed positive expiratory pressure exercises and those who performed deep breathing exercises. The results show that neither lung complications nor days of hospital stay reduced. Along the same lines, Orman and Westerdahl10 obtained no benefits in patients after abdominal and thoracic surgery.
The oscillatory devices have similar features to the above, but encourage bronchial drainage thanks to the generation of an oscillating flow that acts on the properties of secretions.30,46
Lee et al.,63 in a systematic review of patients with bronchiectasis, do not advocate the use of these devices long term despite the positive effects they describe (increased expectoration, avoidance of lung collapse, improved expiratory flow in patients with bronchiectasis and reduced pulmonary hyperinflation). In contrast, Figueiredo et al.64 found that the use of a specific oscillatory device used in patients with bronchiectasis and with a daily mucus production of 25ml improved airway permeability and reduced lung resistance.
Non-invasive mechanical ventilationThis involves applying mechanical ventilation to the lungs using techniques that do not require an endotracheal airway.65
A reduction in lung complications, morbidity and mortality, costs and hospital stay has been described after using continuous positive pressure post vascular,5 thoracic,5,21,66,67 abdominal,2,5,10 or heart surgery.18 The same results were achieved in the treatment of hypercapnic respiratory failure in elderly patients with acute exacerbation of COPD,68 and in patients with cystic fibrosis, it has been described to reduce the work of the inhalatory muscles.69 It is also beneficial in the treatment of acute postoperative respiratory failure,66 prevents postoperative muscle fatigue,18 and reduces endotracheal intubation risk.5,68 It also increases oxygenation,5,47,66,67 improves the benefits of pulmonary rehabilitation,47,66 reexpands collapsed alveoli,70 reduces dyspnoea and increases tolerance to exercise,30,32,67,71 it significantly increases respiratory muscle strength,71 and causes no significant changes in the patient's haemodynamics.47,66
In the review by Rodriguez et al.,9 significant improvement was evidenced in lung function parameters, arterial gasometry and shorter hospital stay in patients who underwent RP with NIMV compared to those with standard RP (IS and coughing),after lung resection surgery. Freitas et al.60 obtained the same result in heart surgery patients.
In terms of negative effects, NIMV can cause discomfort and skin abrasions from the interface, and irritation from device noise.67
Respiratory physiotherapy exercises for patients undergoing invasive mechanical ventilationIn the literature review, we found different RP methods for intubated patients. Hyperinflation, suctioning, postural drainage, percussion, vibration and compression are highlighted. We detail each of the exercises below.
HyperinflationPatients undergoing mechanical ventilation, often sedated and physically restricted, have reduced mucociliary transport with the consequent secretion retention. Hyperinflation aims to imitate the movements of coughing and move secretions towards the upper airway.72,73 It is therefore widely used in intubated patients as a method of RP.7,73–76 It can be carried out with the ventilator or manually.75,77–79
Manual hyperinflation (MH) prevents atelectasis and reexpands collapsed alveoli,8,49,73,74,76,78,80–82 improves oxygenation,8,49,73,78,81–83 increases lung compliance8,16,49,73,78,81,83 and distensibility,8,82 encourages movement of airway secretions,16,49,76,78,81,82 and facilitates weaning.8,73,74,82 Several authors have obtained similar benefits performing hyperinflation with the ventilator.75,77,78 However, hyperinflation is indicated for patients with high PEEP requirements because loss of PEEP has negative effects for the patient.77–79,84
There are discrepancies in terms of the adverse effects caused by MH. Some authors claim that there are none.78,80,84 In contrast, others describe reduced heart rate or increased intracranial pressure.49,73,74,85,86 In all cases, MH is advocated if performed correctly. Several authors highlight that if not performed appropriately the number of complications increase.87,88
Suctioning of secretionsThe aim of this is to eliminate secretions from the central airway and stimulate coughing.49,74
It is considered a measure for which there is a high level of evidence in preventing mechanical ventilation-associated pneumonia.17,22 Choi et al.16 found that suctioning alone had no adverse effects for these patients, therefore it can be used safely. In contrast, other authors describe negative effects such as hypoxaemia, haemodynamic instability, tracheobronchial erosion, haemorrhage, and increased intracranial pressure.49,89 However, these complications reduce with sedation49,89 and preoxygenation.36,49 In patients with high PEEP and FiO2 requirements, suctioning is performed using in-line or closed systems, to avoid disconnection of the ventilator.33,79 In all cases, suctioning is recommended.
Postural drainageThere are no differences in terms of technique, aim, benefits and disadvantages in performing postural drainage between patients with NIMV and spontaneously breathing patients.
Percussion, vibration and compressionWe found no evidence that percussion alone produces changes in the lung function of intubated patients.76 Similarly, neither has an improvement in secretion elimination been described.8,23 In contrast, negative effects have been found such as pain, anxiety, atelectasis and increased oxygen consumption.88
In relation to vibration and manual compression, we found no articles that study these techniques in isolation, but combined they can be useful in moving and eliminating secretions.8,90
DiscussionWe found clear evidence of the efficacy for NIMV as a method of RP for spontaneously breathing post-surgery patients and those with respiratory disease.2,5,9,10,21,66,67 However, the evidence is more limited for other methods of RP in isolation (coughing, vibration, percussion, postural drainage, lung expansion techniques and oscillatory and non-oscillatory systems).
IS is a widely-used method about which there is a great deal of controversy. This might be because of the difficulty in conducting controlled studies and confirming its benefits in preventing complications or reducing days of hospital stay.
We found that hyperinflation is clearly effective in improving lung capacity and reducing respiratory consequences. Similarly, suctioning has proved effective in preventing ventilation-associated pneumonia. This is not the case for the rest of the RP methods used in isolation.
It is worth noting that the efficacy of the different RP methods increases when they are used in combination. Nici et al.32 describe that coughing together with NIMV is more effective than coughing alone. Likewise, IS combined with positive pressure at the end of exhalation is more effective.5,13 Furthermore the combination of postural drainage with percussion and forced exhalation improve mucus clearance in patients with COPD and bronchiectasis,32 and the association of postural drainage with vibration and percussion improves forced vital capacity, arterial oxygenation, exercise tolerance and other aspects.91 Syed et al.38 showed that a combination of percussion, postural drainage, coughing and diaphragmatic breathing are effective in eliminating secretions in patients with bronchiectasis. Along the same lines, vibration techniques associated with multimodality therapy improve functional capacity.92 The association of various techniques have shown beneficial effects for intubated patients. MH together with suctioning promotes better alveolar recruitment, reduces resistance in the airway and improves lung compliance.16,27,36 Likewise, the combination of both with postural drainage and lying on one side reduces the incidence of ventilation-associated pneumonia in patients who have been intubated for more than 7 days.16,27,73 This same result was obtained by Ntoumenopoulos et al.,17 combining postural drainage with vibration and suctioning. Similarly, Berti et al.76 claim that a combination of techniques, such as percussion, MH accompanied with chest compression on exhalation and suctioning, significantly improves weaning from IMV, reduces the stay in ICU, and the extent of lung damage. Pattanshetty et al.90 combined MH, vibration, suctioning and Semi Fowler's position and improved the weaning the process reducing mortality. Cork et al.93 describe how Semi Fowler's position, hyperinflation with the ventilator, vibration and in-line suctioning improved chest radiography and lung compliance in patients with extracorporeal oxygenation membrane. Although adverse effects have been described, such as increased oxygen consumption and CO2 production, a combination of techniques for patients subjected to IMV is still recommended.78
Furthermore, most of the articles we reviewed showed the importance of combining RP with an early mobilisation programme.9,16,17,19,21,24,35,37,94 The beneficial effects they describe include increased oxygen saturation and reduced hospital stay.12 In addition, Morano et al.34 found improvements in maximum inhalation capacity, reduced incidence of postoperative complications and days of hospital stay, and a systematic review by Stiller27 showed an increase in successful weaning rates from the respirator. Similarly, Wong95 obtained benefits in arterial oxygenation and radiography and was able to avoid endotracheal intubation and mechanical ventilation.
As with all nursing care, the choice of exercises for both intubated and non-intubated patients should respect their individual features and not lose sight of the objectives set.3,7,33,36 The success of RP also depends on other factors such as pain, nutrition and functional capacity. It has been described that deep breathing and effective coughing might be limited by pain, affecting lung expansion and increasing the risk of atelectasis.1,5
The role of the nurse is essential in this regard. Appropriate training is required to ensure patient adherence to the treatment and prevent complications.94,96 For example, Hassanzadeh et al.97 highlight that one of the reasons that no benefits associated with the use of IS have been found might be due to a failure to adhere to the treatment. A failure to perform MH correctly on intubated patients triggers haemodynamic alterations.73,98–100 Along the same lines Paulus et al.72 observe the low rate of complications associated with MH when performed by experienced nurses.
All of the above make action guidelines and protocols necessary, with a view to combining criteria and preventing complications.33,101
A limitation of the review was the few articles that describe RP in spontaneously breathing patients admitted to ICU. Similarly, many of the articles we found refer to chronic patients in lung rehabilitation programmes. Furthermore, there is little evidence on how therapies should be combined, and not all the types of exercises are included.
ConclusionsThe literature shows that NIMV is effective in preventing complications and improving lung function for patients with spontaneous breathing. However, the evidence for the other techniques is controversial. Further research studies on these exercises should be undertaken.
The MH technique shows clear benefits as the best method of RP for intubated patients.
Combined therapy shows the best results for both groups of patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Goñi-Viguria R, Yoldi-Arzoz E, Casajús-Sola L, Aquerreta-Larraya T, Fernández-Sangil P, Guzmán-Unamuno E, et al. Fisioterapia respiratoria en la unidad de cuidados intensivos: Revisión bibliográfica. Enferm Intensiva. 2018;29:168–181.