To identify the resources that could improve the care of patients with advanced disease, the present study describes the sociodemographic characteristics of advanced cancer patients dying in a palliative care unit.
MethodWe performed a retrospective study of oncology patients who died in a palliative care unit from January 2006 to December 2009. A descriptive analysis was conducted to compare the clinical and sociodemographic characteristics of advanced cancer patients, using measures of central tendency and frequencies.
ResultsOf the total number of oncology patients, 443 died in the palliative care unit. The most frequent primary cancer site was the lung (20.5%), followed by the liver–pancreas (17.2%), and genitourinary apparatus (16.5%). The primary cancer diagnosis was significantly related to gender (χ2=55.97, p<0.00). The primary cancer diagnosis in younger patients was respiratory tumor. When gender was considered, men with a cancer diagnosis were significantly younger than women (Z=−2.19, p=0.028). No significant differences in the length of admission were identified on comparing means according to the primary cancer diagnosis (χ2=9.77, p=0.36), gender (Z=−0.3, p=0.76) or age groups (χ2=5.29, p=0.15).
ConclusionsAmong patients with advanced cancer who died in the palliative care unit, significant demographic variables were gender and age.
El presente estudio describe las características socio-demográficas de pacientes con cáncer avanzado fallecidos en una unidad de cuidados paliativos, su consideración puede ayudar a la adecuación de recursos que mejoren el cuidado de pacientes con enfermedad avanzada.
SarreraAzterketa honetan, zainketa aringarrietako unitate batean minbizi aurreratuz hildako pazienteen ezaugarri sozio-demografikoak aztertzen dira. Emaitzak lagungarri izan daitezke baliabideak era eraginkorragoan erabili eta paziente hauen zainketa hobetzeko.
MétodoSe trata de un estudio retrospectivo con pacientes oncológicos fallecidos en una unidad de cuidados paliativos entre Enero 2006 y Diciembre del 2009. Se realizó un análisis descriptivo para compara características clínicas y socio-demográficas de pacientes con cáncer avanzado, utilizando medidas de tendencia central.
MetodoaAtzera begirako azterketa, zainketa aringarrietako unitate batean 2006ko urtarriletik 2009ko abendura bitartean minbiziz hildako pazienteekin egina. Analisi deskriptibo baten bidez, minbizi aurreratua duten pazienteen ezaugarri klinikoak eta sozio-demografikoak konparatzen ditu, joera zentraleko neurrien bitartez.
EmaitzakPaziente onkologiko guztien artetik, 443 zainketa aringarrietako unitatean hil ziren. Tumore primario nagusiak: biriketako minbizia (% 20.5), hepatopankreatikoa (% 17.2) eta tumore genitourinarioa (% 16.5). Korrelazio handia dago tumore primarioaren diagnostikoaren eta generoaren artean (χ2=55.97, p<0.00). Paziente gazteenen artean, arnas bideetako tumoreak dira tumore primario nagusiak. Generoari erreparatuta, minbiziz hildako gizonak emakumeak baino gazteagoak dira (Z=−2.19, p=0.028). Ez dago alde nabarmenik ospitaleratzearen iraupenean, batez bestekoak konparatzen baditugu tumore primarioaren diagnostikoaren (χ2=9.77, p=0.36), generoaren (Z=−0.3, p=0.76) eta adin-taldeen (χ2=5.29, p=0.15) arabera.
ResultadosDel total de pacientes oncológicos atendidos, 443 fallecieron en la unidad de cuidados paliativos. La distribución más prevalente del tumor primario fue cáncer de pulmón (20.5%), hepatopancreático (17.2%), y tumor genitourinario (16.5%). Había una alta correlación entre diagnóstico de tumor primario según el género (χ2=55.97, p<0.00). El diagnóstico del tumor primario en pacientes más jóvenes fue de tumores respiratorios. Si se considera el género, los hombres fallecidos por cáncer tienen menor edad que las mujeres (Z=−2.19, p=0.028). No hay diferencias significativas en la duración del ingreso al compara medias según diagnóstico del tumor primario (χ2=9.77, p=0.36), género (Z=−0.3, p=0.76) y grupos de edad (χ2=5.29, p=0.15).
OndorioakGenero eta adinaren araberako emaitza adierazgarriak daude zainketa aringarrietako unitatean minbizi aurreratuz hildako pazienteen aldagai demografikoetan.
ConclusionesEn las variables demográficas de pacientes con cáncer avanzado que fallecen en la unidad de cuidados paliativos aparecen resultados significativos por género y edad.
The national cancer registries in Spain indicated that the proportions of death by cancer in 2006 were decreasing an average 1% for men and 1.3% for women. However, the death rate caused by malignant tumors was estimated to be 26.6% of total mortality, three out of one thousand men and two out of one thousand women died due to cancer. Advanced cancer was the first cause of death in men and was the second cause of death in women. The three types of cancer mortality in Spain were lung, colorectum and prostate for men, and breast, colorectum and lung carcinoma for women.1
In the last few years, palliative care services have been rapidly expanded in Spain for cancer, long-term chronic illnesses or geriatric terminally ill patients. In Catalonia (northeast region of Spain), during 2005, nearly 66% of patients dying of cancer and 44% of patients dying of non-cancer illness needed palliative care services.2 Moreover around 70% of patients admitted for palliative care died in the palliative care unit.2 The implementation of palliative care by multidisciplinary team can prevent and relieve issues that cause suffering families and patients at the end of their life.3 We have some evidence that the specialized palliative care resources may contribute to reduce the cost of the health system to take care of patients with advanced illness.4 It is interesting to consider that, the current implementation of palliative care is focused on the needs of the patient and their families to improve the quality of the care of the advanced diseases.5
The issues related to differences of socio-demographic characteristics of patients admitted at palliative care unit have been only partly considered. In previous studies, a representative population of patients with advanced cancer, age and gender were considered with performance status, symptom control variable and primary site, as predictor of morbidity in advanced cancer.6 In other studies, the male gender was found to be a factor associated with in-hospital mortality, independent of primary cancer diagnosis.7 Considering more prevalent leading sites of cancer, a number of studies have described clinical and socio-demographic factors related to advanced cancer incidence and mortality. Initially, the findings about the gender-associated differences in presentation and survival from lung cancer showed that the proportion of advanced disease was equally high in every gender. However, women were diagnosed at a younger age and early stage but survival in women appeared to be longer than in men.8 Similar differences between genders were also found in patients with advanced melanoma disease. There was superior female survival after the diagnosis and progression of melanoma, but among male all included tumor characteristics were less favorably distributed.9, 10 In upper tract urothelial carcinoma, an unfavorable gender distribution for female was found on cancer specific mortality. However, in this study, gender did not achieve an independent predictor status after the prognosis adjustment for tumor characteristics such as stage, tumor grade, year of surgery, or other demographic characteristics such as patient's age.11
In some studies based on the national registries of cancer estimated the annual prevalence and incidence of cancer. However, little is known about the distribution of primary cancer diagnosis of inpatient palliative care unit, and the related demographic characteristics. Therefore, the purpose of this study is to use a retrospective design, to describe demographic characteristics of oncology patients who died at palliative care unit. Moreover, this study determines whether factors such gender, age or admission's length were associated with specific primary cancer diagnosis.
Materials and methodsThis study was conducted at Antic Hospital Sant Jaume i Santa Magdalena, which is a socio-health center in Barcelona (Spain). In this center, the palliative care unit had 12 beds, and the unit is staffed by a multidisciplinary healthcare team including geriatric physicians, trained nurses in gerontology, physical therapists, nutritionist, social workers and clinical psychologist. The unit admitted patients whose illnesses were non-surgical and did not require intensive care. The patients with advanced disease were transferred to palliative care unit when the disease complexity required symptom control or psychosocial care by the multidisciplinary team. The patients are also admitted from another hospital services such as the home care service, after evaluation by the consultation team.
In this retrospective study, data were collected from all the patients admitted to palliative care unit from January 1, 2006 up to discharged patients in December 31, 2009. The analysis included patients who died from cancer at palliative care unit. From an institutional database, the following factors were evaluated: gender, age, primary cancer diagnosis, duration of the entire hospitalization from date of admission to date of discharge, and information about the patient's admission outcome. Permission to conduct this study was received from the Institutional Review Board at the Antic Hospital St. Jaume i Sta. Magdalena and waived the requirement to the informed consent.
Statistical analysisDescriptive statistics were calculated to demographic data using measures of central tendency and frequencies. Admission length at palliative care unit measured by days, and patient's age were treated as a continuous variable. In addition, analysis for age was performed separately for patients up to 64 years of age, from 65 to 74 years, from 75 to 84 years and patients aged 85 years or over. The primary cancer diagnosis was categorized according to ICD-9 codes. Moreover the types of gastrointestinal cancer were separated into the more frequent categories, such as colorectum, higher gastrointestinal (esophagus, stomach, small intestine) and hepatopancreatic.
Pearson Chi-square test was used for categorical variable. Non-parametric tests were used to compare quantitative variable analysis, when one-way analysis of variance was not applicable. A p value <0.05 was considered statistically significant. Post hoc multiple comparisons with Bonferroni adjustment were used to identify differing subgroups. The Statistical Package for the Social Sciences (SPSS version 11) was used for statistical analysis.
ResultsThere were a total of 694 admissions during the study period. From the total number of admissions, 632 (91.1%) patients had only one admission, 53 (7.6%) patients had a second admission, and 9 (1.2%) patients had three or more admissions. From the total sample admitted over these four years study period, 533 (76.8%) died at palliative care unit. From the patients discharged alive, 73 (10.5%) were sent home, 55 (7.9%) were transferred to long-term care unit, and 33 (4.8%) were sent to other institutions.
Considering eligible only all first-time palliative care unit admissions, the patients with an admitting diagnosis of cancer were 522 (82.6%), which is higher than the patients with other diagnosis. The first-time admissions of non-cancer diagnosis 34 (5.4%) patients had pulmonary disease, 30 patients had dementia (4.7%), 24 patients (3.8%) had cardiac disease, 13 patients (2.1%) had renal failure or disease, and 9 (1.4%) patients had other neurological disease or not specified disease. The cancer was the most prevalent illness treated at palliative care unit and the primary cause of death. In this study a total of 443 (83.11%) inpatients died due to cancer. The retrospective analysis was therefore based on these oncology patients. Table 1 showed demographics characteristics of oncology patients who died at palliative care unit. Compared with women (n=144, 32.5%), a higher proportion of men (n=299, 67.5%) with cancer diagnosis died at palliative care unit. The mean age of all patients was 76.5 years (range 39–100 years). The majority of the patients have an age between 75 and 84 years old, or higher. Median length of stay at palliative care unit was 12 days (range less than 24h to 175 days). Regarding the cause of death by the localization of primary cancer, the three most frequent tumors at palliative care unit were lung (20.5%), hepatopancreatic (17.2%), and genitourinary (16.5%).
Table 1. Demographic characteristics of cancer patients at palliative care unit (n=443).
| Characteristics | |
| Admission length (days) | |
| Mean | 20.76 |
| Median | 12 |
| Std. deviation | 25.67 |
| Range | Hours to 175 |
| Age | |
| Mean | 76.5 |
| Median | 78 |
| Std. deviation | 11.69 |
| Range | 39–100 |
| N | % | |
| Gender | ||
| Female | 144 | 32.5 |
| Male | 299 | 67.5 |
| Age | ||
| Lowest to 64 | 76 | 17.2 |
| 65–74 age | 76 | 17.1 |
| 75–84 age | 170 | 38.4 |
| 85 to highest | 121 | 27.3 |
| Primary cancer | ||
| Head and neck | 12 | 2.7 |
| Hematologic | 23 | 5.2 |
| Genitourinary | 73 | 16.5 |
| Central nervous system | 22 | 5 |
| Unknown primary | 21 | 4.7 |
| Dermatologic, breast | 22 | 5 |
| Colorectum | 58 | 13.1 |
| Respiratory | 91 | 20.5 |
| Higher gastrointestinal | 45 | 10.1 |
| Hepatopancreatic | 76 | 17.2 |
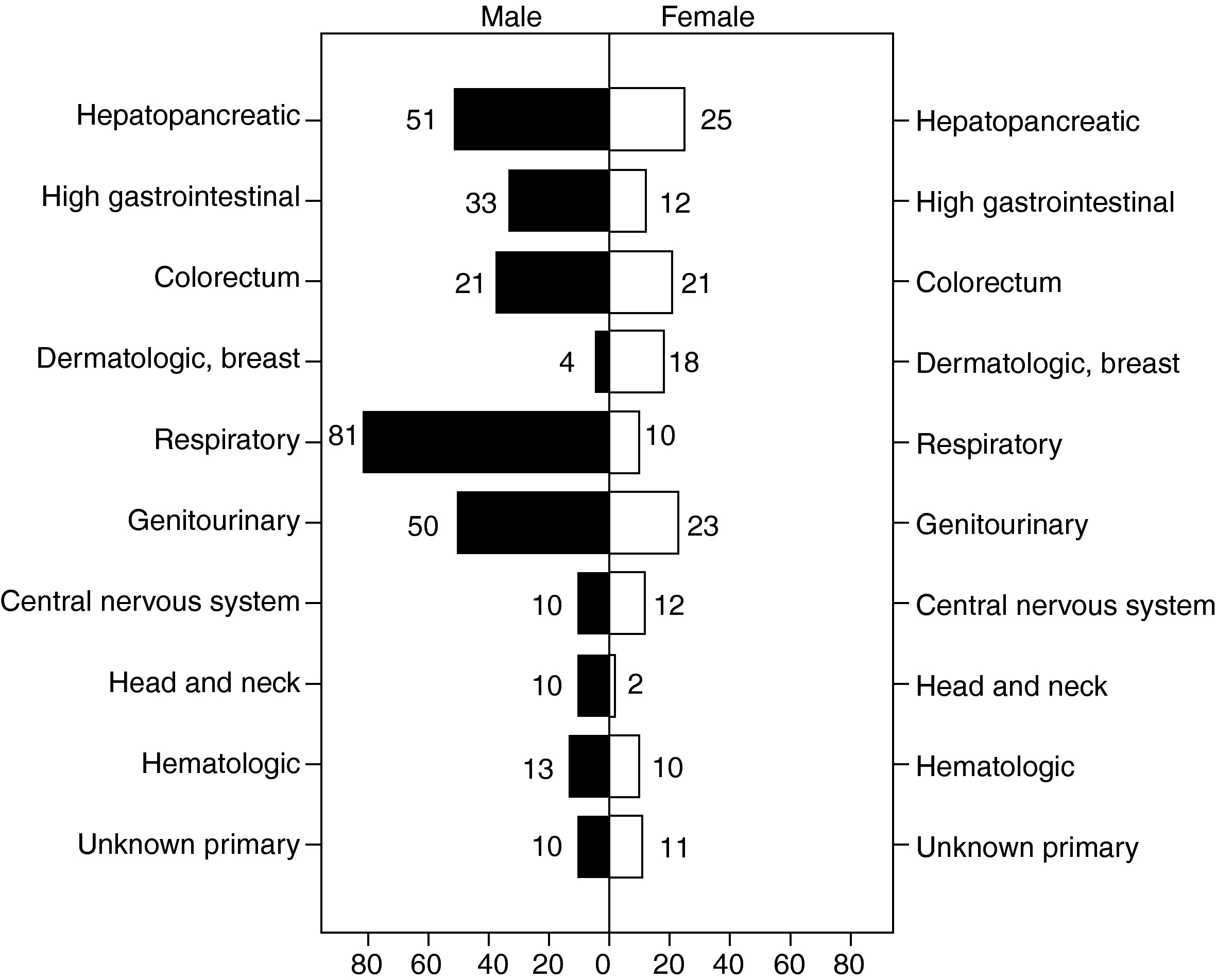
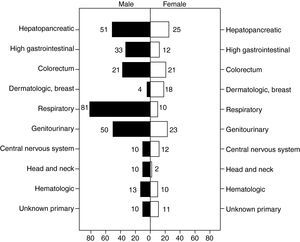
Primary cancer diagnosis among men and women are presented in Figure 1. The most frequent tumor at palliative care unit in men was respiratory (n=81) followed by hepatopancreatic (n=51) and genitourinary (n=50). In women, the most common cancer was hepatopancreatic (n=25) followed by genitourinary (n=23) and colorectum (n=21). The statistical analysis using Chi-squared test, patient's primary cancer diagnosis showed a significant relationship to gender (χ2=55.97, p<0.00).
Figure 1. Distribution of primary cancer diagnosis by gender at palliative care unit.
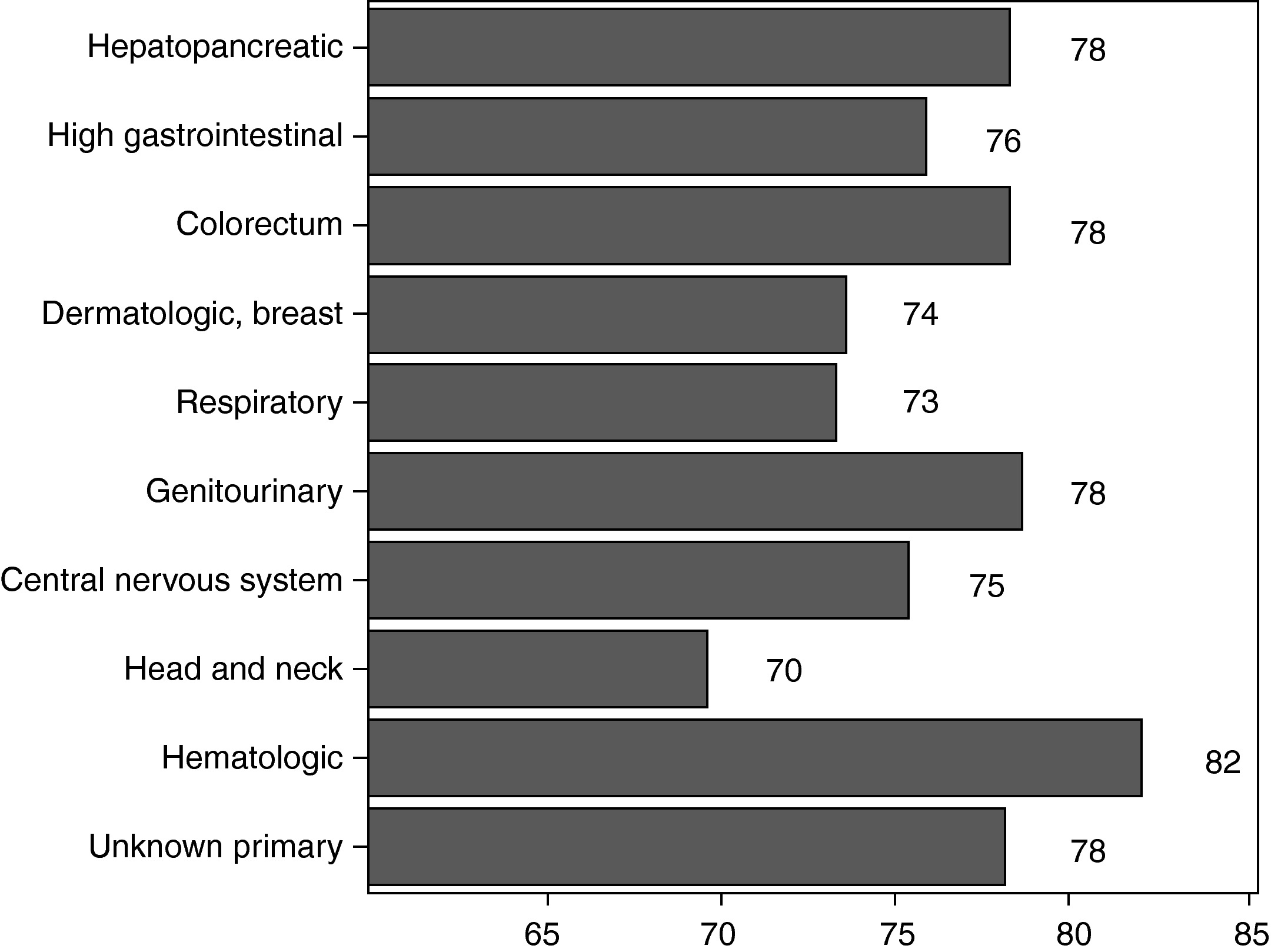
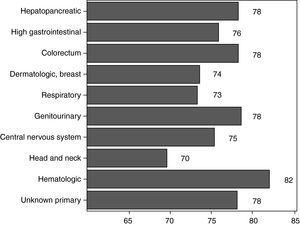
AgeConsidering the age variable, normality of test distribution was not assumed (Z=2.33, p<0.00), and the non-parametric test was applied to compare means. Significant differences in the type of tumor were determined by using Kruskal–Wallis H statistics on age (χ2=28.47, p<0.00). Due to the fact that the variable primary tumor had ten groups, it was realized forty-five comparisons two to two using Mann–Whitney U test. In this study the correction of Bonferroni was used to a level of signification of 0.001. Depending of age it was found a significant statistically differences between Hematologic and Respiratory tumors (Z=−4.15, p<0.000). Moreover, differences were found between Genitourinay and Respiratory tumors (Z=−3.74, p<0.000) and between Respiratory and Hepatopancreatic tumor (Z=−3.78, p<0.000). There was a trend towards statistical significance between Respiratory and Colorectum tumor (Z=−2.97, p=0.003) by age. A high difference between primary cancer diagnosis in younger patient was found for respiratory tumor. The mean age of patients for primary cancer diagnosis was shown in Figure 2.
Figure 2. Means age of patients at palliative care unit by primary cancer.
In order to examine the differences in age by gender, a Mann–Whitney U test was used. In the patients admitted at palliative care unit compared by gender the difference was statistically significant (Z=−2.19, p=0.028). The men were aged significantly lower (median: 78 age, range: 39–100 years old) compared to women patients (median: 81 age, range: 42–99 years old).
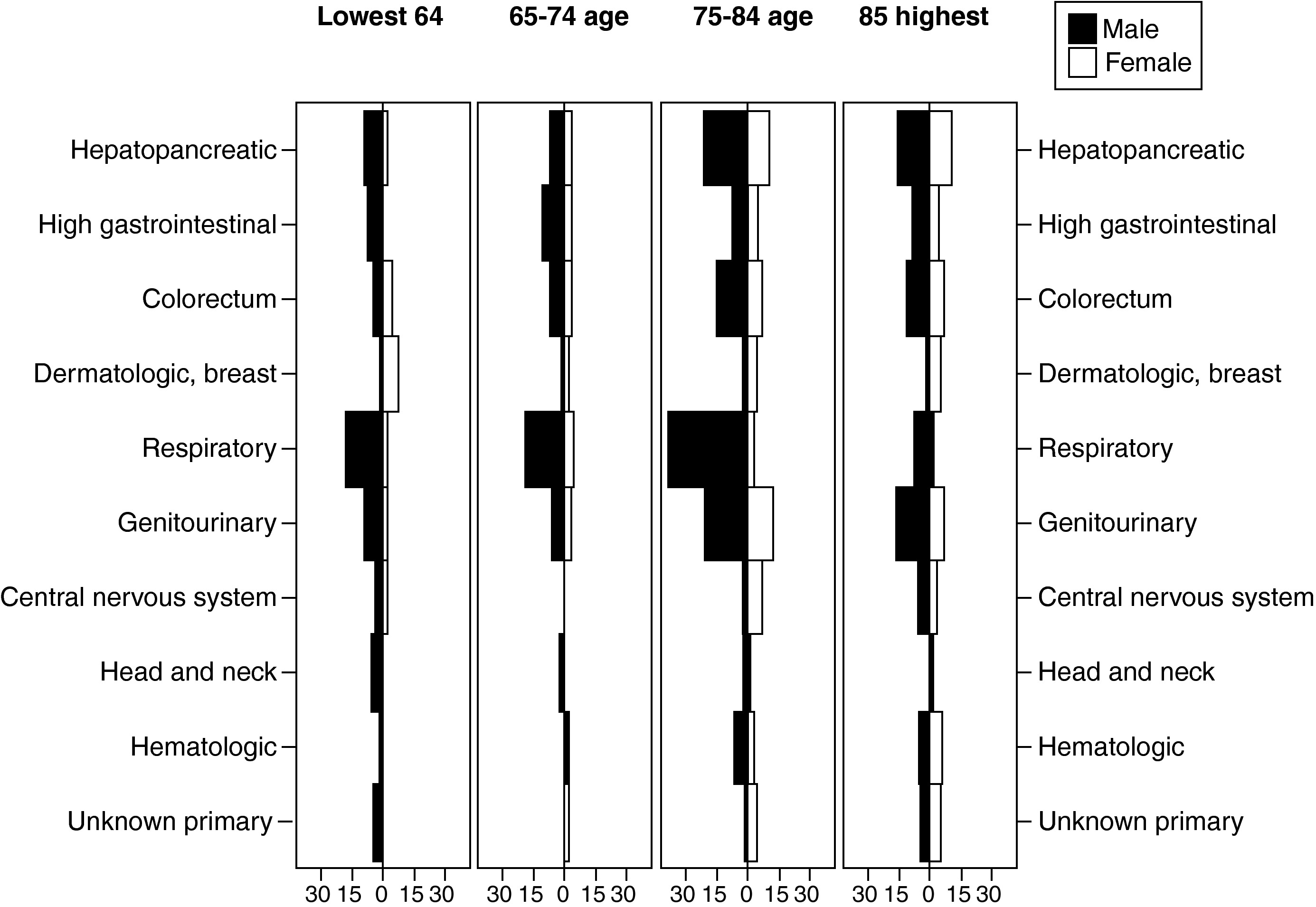
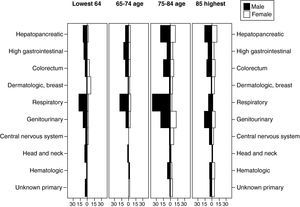
To highlight the different effects of age on primary cancer diagnosis of patients who died at palliative care unit, four age groups were made in patients more than 60 years old. When deepening in the descriptive analysis of the primary cancer diagnosis by age groups and gender, statistical analysis was not calculated because of the reduced count of data on the categories list. Nevertheless, the frequencies of primary cancer tumor by age groups and gender are shown in Figure 3.
Figure 3. Distribution of primary cancer diagnosis by age groups and gender.
Length of admissionsThe Kolmogorov–Smirnov test did not indicate a normal distribution of length of admissions variable measured by days (Z=4.45, p<0.00). Non-parametric Kruskall–Wallis H test was applied to compare means of primary cancer diagnosis, and age groups. No significant differences in the type of tumor were determined using Kruskal–Wallis H statistics on length of admissions (χ2=9.77, p=0.36). The comparison of age groups on length admissions at palliative care unit showed significant differences (χ2=5.29, p=0.15).
The mean duration of hospital admission by gender for oncology patients who died in hospital were similar. In the female patients 21.98 days (Std. deviation: 26.14, range: hours to 134 days) and in male patients were 20.17 days (Std. deviation: 25.46, range: hours to 175 days). Using Mann–Whitney U test appeared that the difference by gender was not significant on length of admissions (Z=−0.3, p=0.76).
DiscussionThe number of palliative care programs increasing recently in Spain (specifically in Catalonia), permits to study in depth the patient's care with advanced disease. Palliative care is an essential part of the continuum treatment of cancer patients. Moreover, in this study we consider that 82.7% of the total first-admissions at palliative care unit were oncology patients. This is higher than the palliative care coverage for cancer patients that occurred in other countries.12
Similarly to others studies,12, 13 palliative care unit are more likely to attend patients diagnosed with primary lung cancer, which was also the leading primary cause of death in Spain.1 In this study, hepatopancreatic and genitourinary tumors were diagnosed more commonly among patients admitted and who died at palliative care unit. Therefore, they are more prone to the need of palliative care unit services. But in terms of cancer diagnosis, present studies highlight that besides lung cancer, gastrointestinal and hematologic malignancy cancers were found to be associated with higher hospital death rate.7, 13
As expected, there was higher proportion of advanced tumors in men than in women who were treated at palliative care unit. A recent study also revealed male gender to be a factor associated with in-hospital mortality.7 However, more than gender and age, the primary site of cancer appears to be an important predictor of morbidity in advanced cancer.6 Besides the different factors attributed to gender that influence the death in the hospital, the death in men was more related to medical condition whereas in women it was related to functional dependency.14 Adding the effect of age, it should be noted that in the result of the current study the men were aged significantly lower compared to women patients. Moreover, younger patient's age was found for respiratory tumor. Differences by gender, age and primary cancer diagnosis could be factors to reflect the characteristic of patient's disease complexity. This determines the needs for symptom control and psychosocial care that have to be managed at palliative care unit.
National data have reported discrepancies in the incidence and prevalence of cancer according to gender1 and similar discrepancies are held at palliative care unit. The most frequent tumor in men was respiratory cancer followed by hepatopancreatic and genitourinary cancers (specifically, prostate), while in women it was hepatopancreatic followed by genitourinary and colorectum cancers, respectively.
A key finding in the current study was that age, gender and primary cancer tumor were not a significant variable related to length of admission at palliative care unit but instead other variables did yield significant findings. It is important to note that many of the patients diagnosed with cancer may have metastases at admission, which could explain comorbidities or complications of symptoms and length of patients’ survival at palliative care unit. The analysis in a gynecological cancer sample shows that the effect of age did not only have an independent prognostic effect on survival but it was strongly influenced by stage of disease and type of treatment.15 Similar results were reported in colon carcinoma. Those results show that there was not a significant relationship between higher stage and older age, but there was an increasing risk of death with increasing diseases’ stage.16 Regarding the length of admission, medical comorbidities could be more significant than age, gender or symptoms to primary sites when cancer is advanced.
There are several limitations in this study that should be considered for future clinical trials. Firstly, the retrospective design of this study is limited to the nature of the data that was collected. Important clinical variables, such as performance status, psychological distress, medical comorbidities, responsiveness of symptoms or other parameters that might also carry a prognostic value, were not included in this study. Secondly, our study does not provide any useful data on effects of symptom control that plays a critical role in attending to patients’ comfort measures for terminally ill patients. In addition, the current study included mortality data of oncology patient for a single unit of palliative care. This may limit the degree to which these results could be generalized. The patterns of palliative care delivery may vary across the same country. Finally, in future studies should be considered further efforts to document socio-demographic factors on patients with long-term chronic illnesses. The studies should consider older persons affected with cancer or geriatric terminally ill patients, in the same way as the potential determinants for predicting in-hospital mortality.
Conflicts of interestNo conflicts of interest to declare.
Acknowledgements
The invaluable work of Leonor Domínguez and Silvia Martínez for their assistance with data register is highly appreciated.
Received 21 June 2011
Accepted 30 August 2011
Corresponding author. gcosta@csdm.cat