Aetiological diagnosis of acute hepatitis is sometimes difficult. We present the case of a patient with a rare cause of this condition.
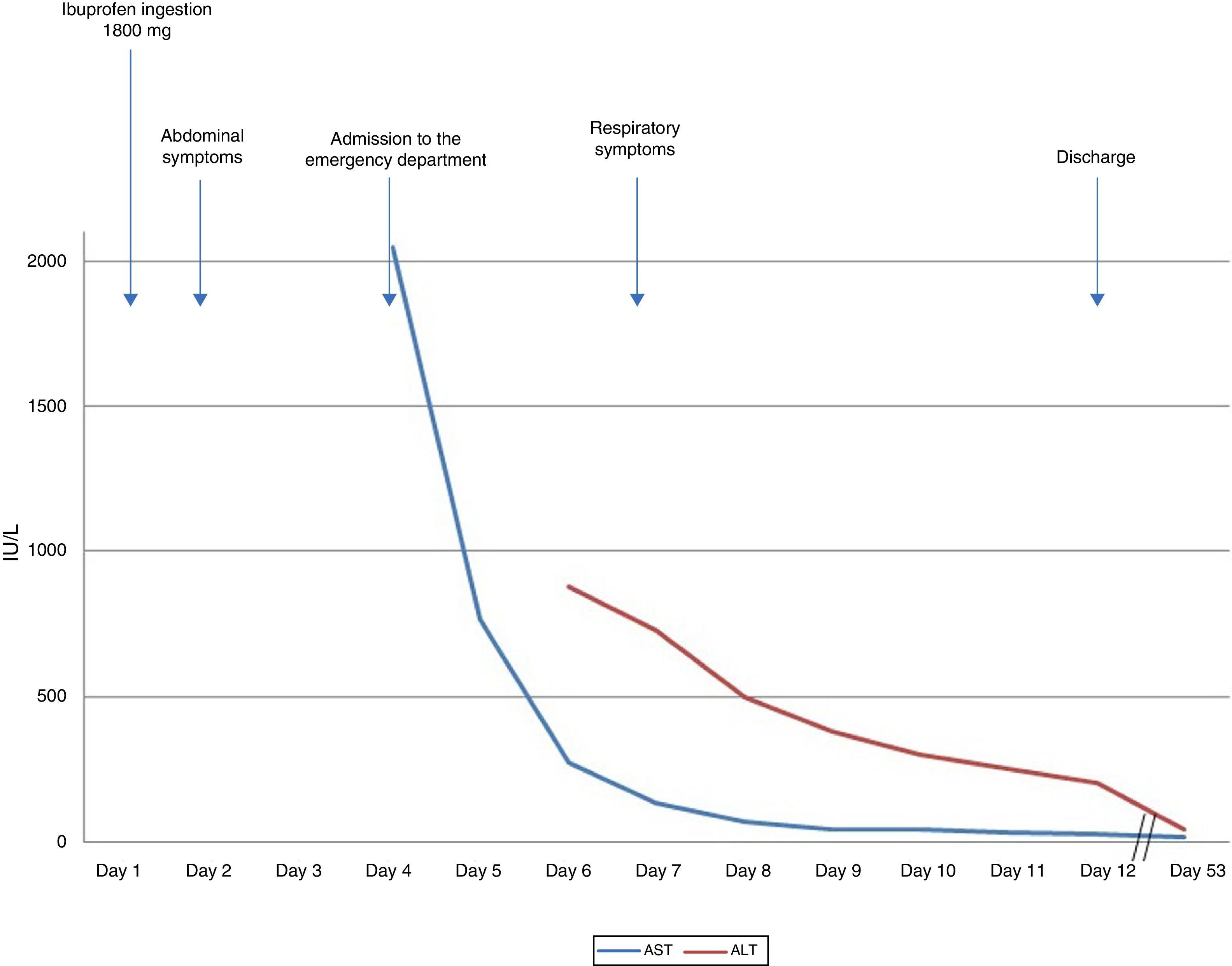
A 32-year-old woman, with no family or personal history of note and receiving no regular treatment, presented in the emergency department with a 48-h history of diffuse abdominal discomfort associated with nausea and vomiting, unaccompanied by fever or respiratory symptoms. She had taken 1800mg of ibuprofen for dysmenorrhoea 24h before onset of symptoms. Physical examination was unremarkable, but blood tests taken in the emergency department showed pancytopenia, international normalised ratio (INR) 1.6 and aspartate aminotransferase (AST) 2045IU/L. The evolution of the liver profile is shown in Fig. 1. Total bilirubin, gamma-glutamyl transferase (GGT) and alkaline phosphatase (ALP) were all within reference ranges. Abdominal ultrasound revealed a normal-sized liver with hyperechogenicity of the portal system, splenomegaly and a small amount of free fluid but no other abnormal findings. The initial aetiological study – including autoimmune study, alpha-1 antitrypsin, iron profile, complete viral serology (anti-HVA IgM, HBsAg, anti-HCV, HCV PCR assay, anti-HVE, anti-EBV IgM and anti-CMV IgM) and bacterial serology–was negative. The only remarkable finding was low ceruloplasmin levels; however, 24-h urinary copper concentrations were normal. On the third day after admission, the patient presented a dry cough, odynophagia and enlarged laterocervical lymph nodes. Polymerase chain reaction (PCR) testing for H1N1 virus in nasopharyngeal exudate showed positive and a chest X-ray was normal. The patient was diagnosed with influenza A (H1N1) infection. Treatment with oseltamivir for 5 days resulted in a gradual clinical and analytical improvement (AST 28IU/L, alanine aminotransferase (ALT) 205IU/L). At a check-up 53 days after symptom onset, the patient's liver function test results had completely reverted to normal values.
Influenza A (H1N1) infection is characterised by pulmonary involvement, with cough, fever, general malaise and headache that remit spontaneously after 6–8 days. Severe infection is characterised by pneumonia, septic shock and multi-organ failure.1,2 Liver involvement in influenza virus infections has been demonstrated in experimental animal models. Cases of liver failure have been described in children; in adults, however, there have only been reports of moderately elevated liver function tests or episodes of hepatic decompensation in patients with underlying chronic liver disease.3,4
Prior ibuprofen ingestion as a cause of hepatic impairment is a plausible alternative, as it occupies third place among hepatotoxic drugs in the Spanish DILI Registry.5 Since a score of 7 points (probable) was obtained on the Council for International Organization of Medical Scientists (CIOMS) causality assessment scale, the patient was advised to avoid ibuprofen use. The time of symptom onset, presence of pancytopenia and splenomegaly and absence of immunoallergic symptoms6 on admission all suggest influenza A as the cause; however, the appearance of respiratory symptoms 5 days later raises the question of whether the initial liver symptoms were of toxic origin. The gradual resolution after ceasing ibuprofen intake and initiating antiviral treatment is not helpful in discriminating between the two possible causes. Establishing the aetiology of the symptoms with certainty is difficult. Since the presentation of influenza A as acute hepatitis without respiratory symptoms is unusual, the only way to determine whether the symptoms were caused by an episode of hepatotoxicity secondary to ibuprofen would be to run a rechallenge test–which obviously was not possible for ethical reasons.7 Finally, a liver biopsy was ruled out, given that symptoms rapidly improved to the point where liver function results reverted to normal.
This is a clear example of toxic liver injury as a “great mimic” of liver disease. Because the disorder can resemble any acute or chronic liver disease, diagnosis is difficult and requires all alternative causes of liver damage to be ruled out, including less common ones, such as influenza A in our case.
Please cite this article as: Ortega-Alonso A, García-Cortés M, Fernández-Castañer A, Ruiz J, González-Amores Y, Andrade RJ. Hepatitis aguda en una paciente con gripe A: ¿casualidad o causalidad? Gastroenterol Hepatol (Engl Ed). 2016;39:20–21.