Extrahepatic disease often develops during progression of hepatocellular carcinoma, but metastatic disease as an initial manifestation is rare. Our case study is a 61-year old male patient who received an orthotopic liver transplantation 10 years ago due to decompensated alcohol-related cirrhosis and hepatitis C virus infection with no virological response to earlier therapies.
Pathology tests on the explanted liver specimen ruled out the presence of hepatocellular carcinoma. Following transplantation, immunosuppressant therapy with ciclosporin 150mg/12h and mycophenolate mofetil 500mg/12h was initiated. During the first few months following transplantation, the patient's laboratory and histology test results were suggestive of rejection, which was resolved with corticosteroid therapy. The patient was then monitored using blood tests, ultrasound and Fibroscan®, with no evidence of significant alterations and maintaining normal liver function. Nine years after the transplantation, the patient was treated with a combination of sofosbuvir, ledipasvir and ribavirin for 12 weeks, achieving sustained virological response. One year later, elevated alpha-fetoprotein levels (111.89IU/ml, increased from 7.6IU/ml) were observed in a routine blood test.
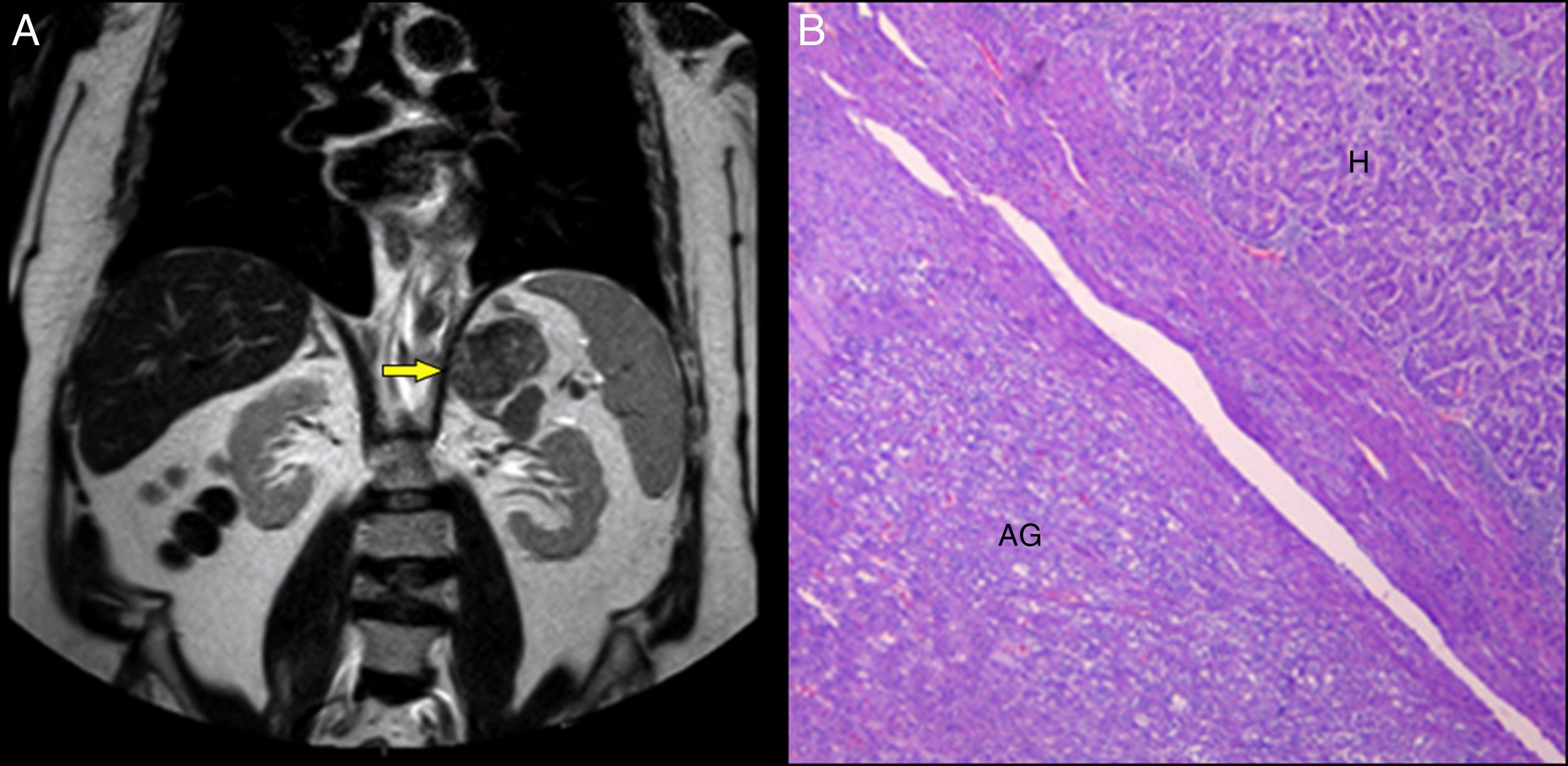
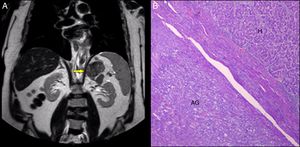
A multiphase computerised axial tomography scan (CT scan) of the abdomen was performed, which showed a liver graft of normal size and morphology, and a nodule measuring 4mm in liver segment VI with contrast uptake in the arterial phase and no evidence of washout in the venous phase, LI-RADS-3. A lobulated, solid, left adrenal mass measuring 77×44mm was also described. Three months later, magnetic resonance imaging (MRI) of the abdomen showed enlargement of the adrenal lesion (88×66mm) (Fig. 1A), which was not characterisable with this imaging method, and stability of the liver lesion. The presence of hormone hypersecretion was ruled out: thyroid function tests, cortisol, ACTH, DHEA, 17-OH progesterone, urine catecholamines and cortisol suppression following dexamethasone injection were all within the normal range. It was decided that it was best to surgically remove the lesion. Histopathology tests (Fig. 1B) revealed a metastatic carcinoma with an immunohistochemical morphology and profile consistent with hepatocellular carcinoma (Hep Par-1, cytoplasmic TTF-1, CAM 5.2 and CD10). There was no infiltration of the resection margins. The size of the liver lesion had remained stable on the control CT scan. A PET/CT scan was performed, which showed no suspicious malignant lesions. Today, five months after surgical resection, the patient is stable and shows no signs of tumour recurrence on imaging scans, with alpha-fetoprotein levels of 6.7IU/ml.
Adrenal incidentalomas are extremely common. Although the best way to manage such tumours has not been completely determined, the first step is to rule out the presence of hormone hypersecretion and the possibility of malignancy.1
Some lesions may be characterisable from imaging scans. In other cases, pathology testing of the lesion may be required to determine whether it is benign or malignant.1
Metastases account for 5% of adrenal incidentalomas.1 The incidence of adrenal metastasis from hepatocellular carcinoma in autopsy series ranges from 4.6% to 12.5%, and it is the fourth most common site of metastasis after the lungs, lymph nodes and bones.2 It has been suggested that the most likely mechanism of onset is arterial spread via the aorta.3
These lesions can be synchronous or metachronous, and may appear years after liver transplantation performed to treat hepatocellular carcinoma.4 However, adrenal metastasis as the first clinical manifestation is extremely rare.5 A literature review revealed a few cases in which metastasis was the initial manifestation of hepatocellular carcinoma. Bone lesions, right atrial metastases, lesions in the parotid gland, a mass in the gluteal region and adrenal metastases have been reported.4,5 However, in all of these cases, a primary lesion was detected during follow-up,4,5 unlike the case study presented herein, in which, 9 months after initial diagnosis, there was no evidence of intrahepatic disease. Therefore, based on existing scientific evidence, this is the first ever described case of adrenal metastatic disease with no evidence of a primary liver tumour.
To conclude, adrenal metastasis can be the first manifestation of the disease and must be considered if an adrenal incidentaloma is detected in patients with an increased risk of hepatocellular carcinoma.
Please cite this article as: Sánchez Rodríguez E, Ríos León R, Flores de Miguel Á, Guerrero García A, Pian H, Gea Rodríguez F, et al. Metástasis adrenal como presentación de un hepatocarcinoma. Gastroenterol Hepatol. 2019;42:171–172.