A 31-year-old man with past medical history of anal fistula 6 years before and bone marrow failure of unknown etiology diagnosed two months before presentation, was admitted at the Hematology Department due to fever, abdominal pain and nausea. He was under ciclosporine 400mg/day and aciclovir 400mg 3 times a day. The results of his examination were significant for moderate epigastric and umbilical abdominal pain and laboratory data showed pancytopenia (similar to previous results) and C reactive protein of 266mg/dL. Ultrasound imaging was unremarkable.
He was then treated with piperacilin/tazobactam 4.5g/3 times a day. The CT scan showed two segments in the jejunum with wall thickening and mesenteric edema and vascular mesenteric prominence.
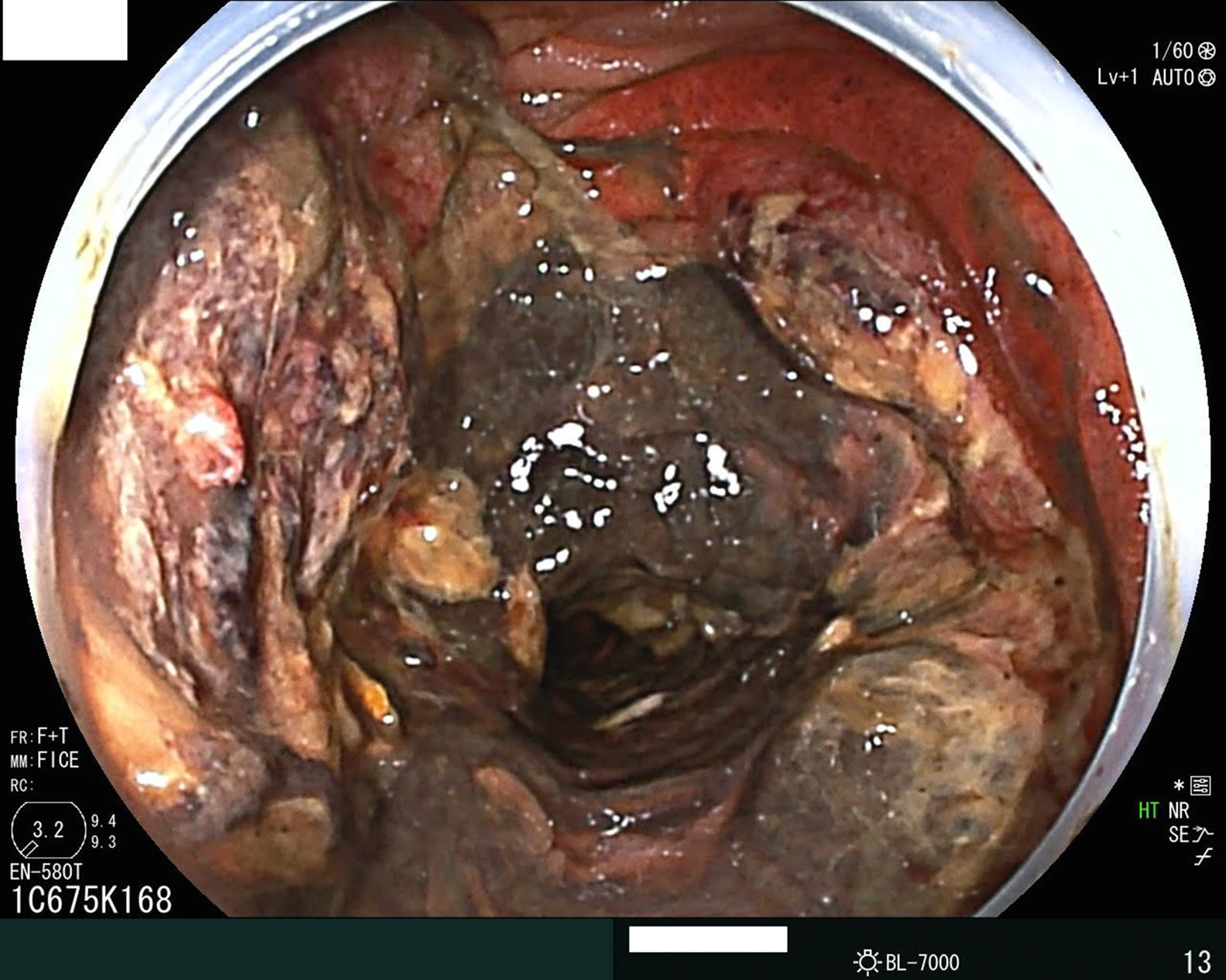
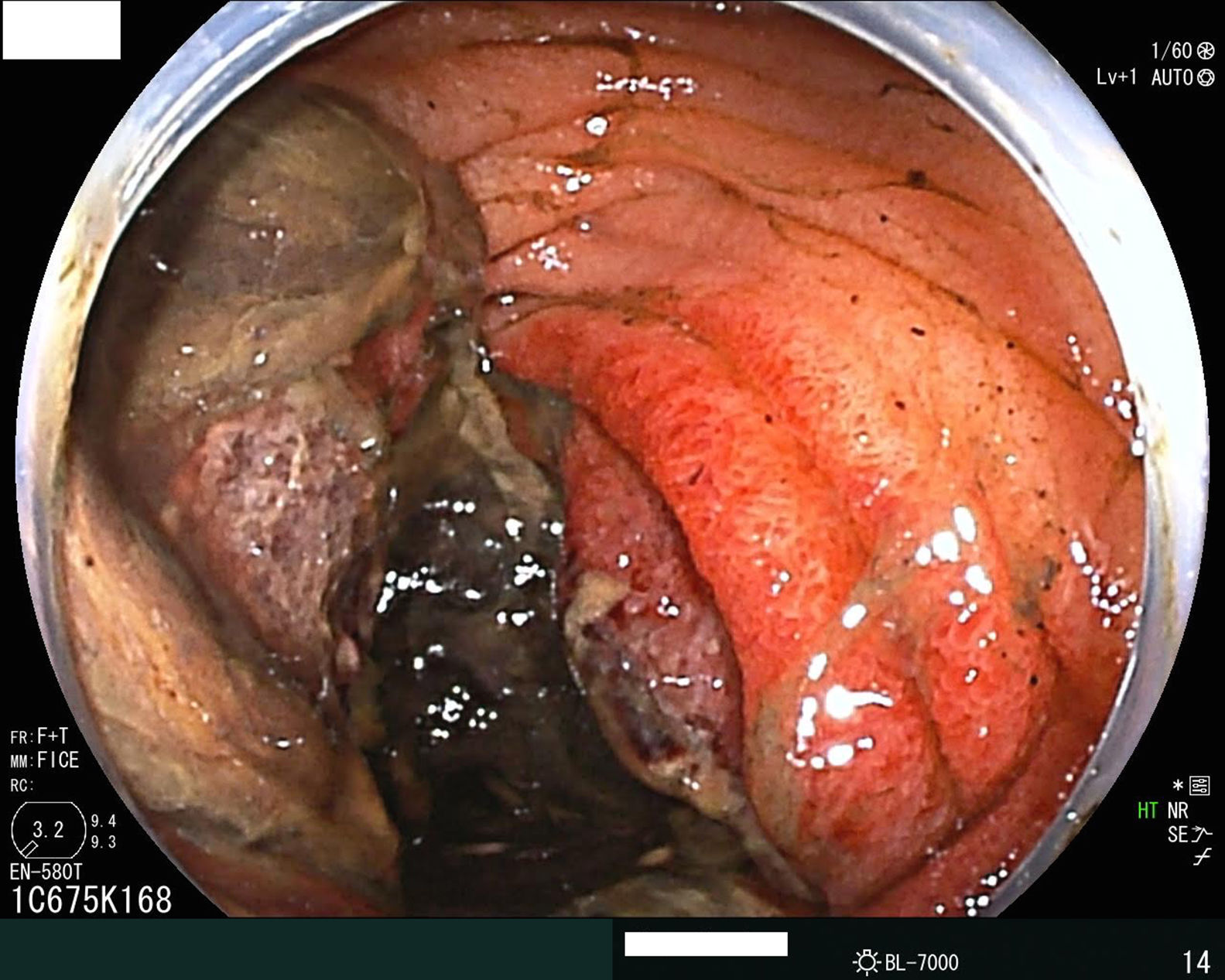
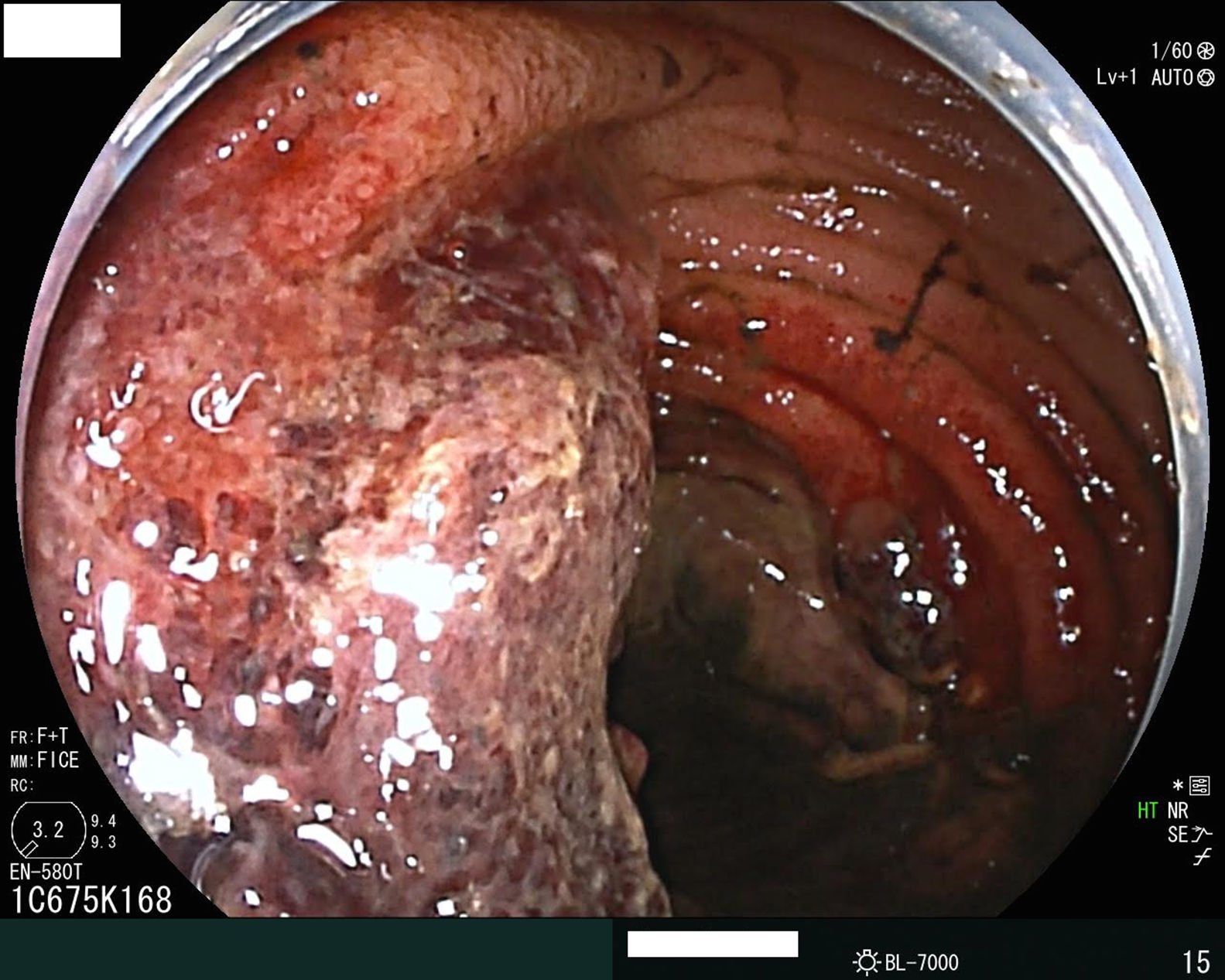
In the clinical discussion we proposed to perform an enteroscopy which showed a 10cm segment in the proximal jejunum with edematous and fragile mucosa, with ulceration and extensive necrosis (Figs. 1–3).
Histopathological specimen was compatible with ischemic enteritis.
Ischemic enteritis is a rare entity but with high mortality. Therefore, early recognition is very important in the management of these patients.