A 65-years old male with known liver cirrhosis presented with massive melena, associated with hemodynamic instability, respiratory failure and alteration of the state of consciousness. Relevant analytical findings included anemia (hemoglobin 11.4g/dL), thrombocytopenia (114.000U/L) and hyperlactacidemia (6.2mmol/L).
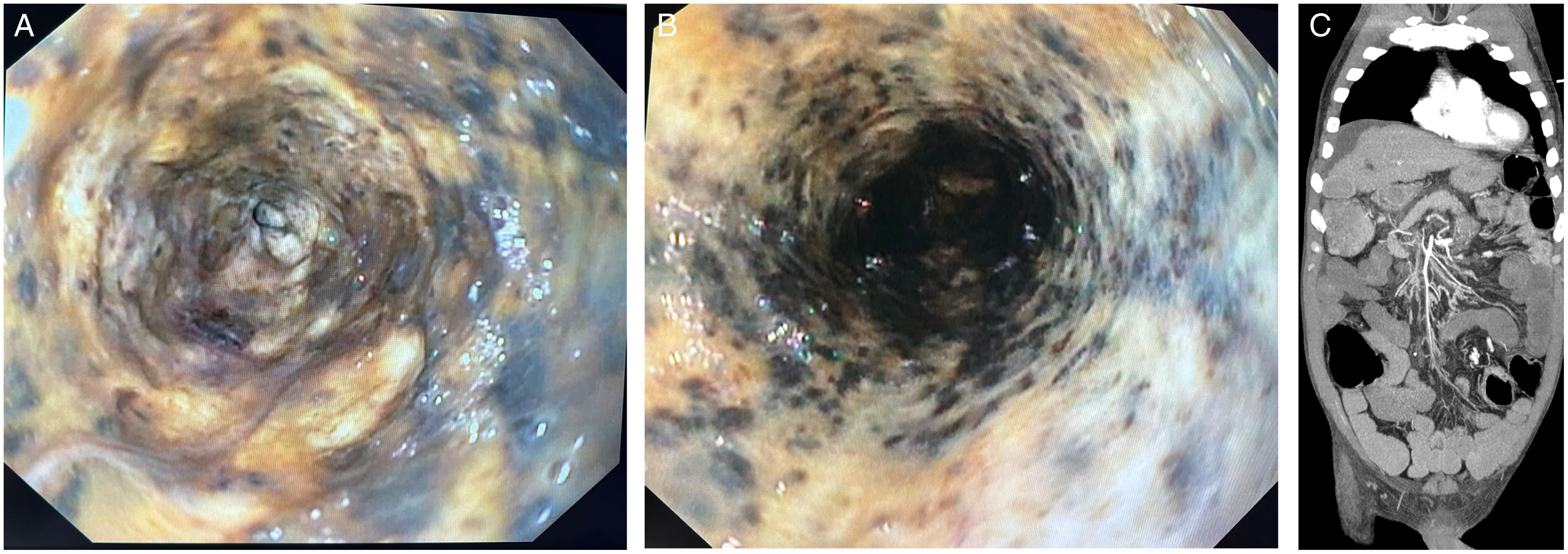
The patient underwent endotracheal intubation, being admitted in ICU, and emergent esophagogastroduodenoscopy was performed, revealing a diffuse circumferential black mucosal discoloration of the whole esophagus, with numerous necrotic areas, and an abrupt transition to normal mucosa at the gastroesophageal junction, compatible with acute esophageal necrosis syndrome (AENS) (black esophagus) (Fig. 1A and B).1 Subsequent CT with angiography showed signs of extensive mesenteric ischemia, with gaseous bubbles in several mesenteric branches (Fig. 1C), interpreted in the context of poorly controlled cardiovascular risk factors. The clinical situation deteriorated significantly, with the patient perishing the following day.
AENS is typically caused by ischemic events, with decreased esophageal blood flow leading to fast development of extensive necrosis. The distal third of the esophagus is usually more susceptible to injury, as it is less vascularized compared with other segments.1
With this case, we aim to share a rare entity, and highlight the wide range of causes of massive upper gastrointestinal bleeding, even in patients with known cirrhosis.
Ethical considerationsInformed consent acquisition was not possible due to patient's death.
FundingNothing to declare.
Conflict of interestNothing to declare.