Casos Clínicos en Gastroenterología y Hepatología
Más datosA 24-year-old man presented to our department, complaining about abdominal pain, nausea, vomiting and weight loss over a period of 2 weeks. He denied any symptoms of fever, headache, diarrhea, or constipation, and any history of special medication. Approximately 3 years earlier he had been diagnosed in another hospital with intestinal obstruction after presentation with similar symptoms. On admission, physical examination revealed tachycardia and an anemic appearance. Body temperature, blood pressure, and respiratory rate were within the normal ranges. The abdomen was soft, non-tender, and non-distended.
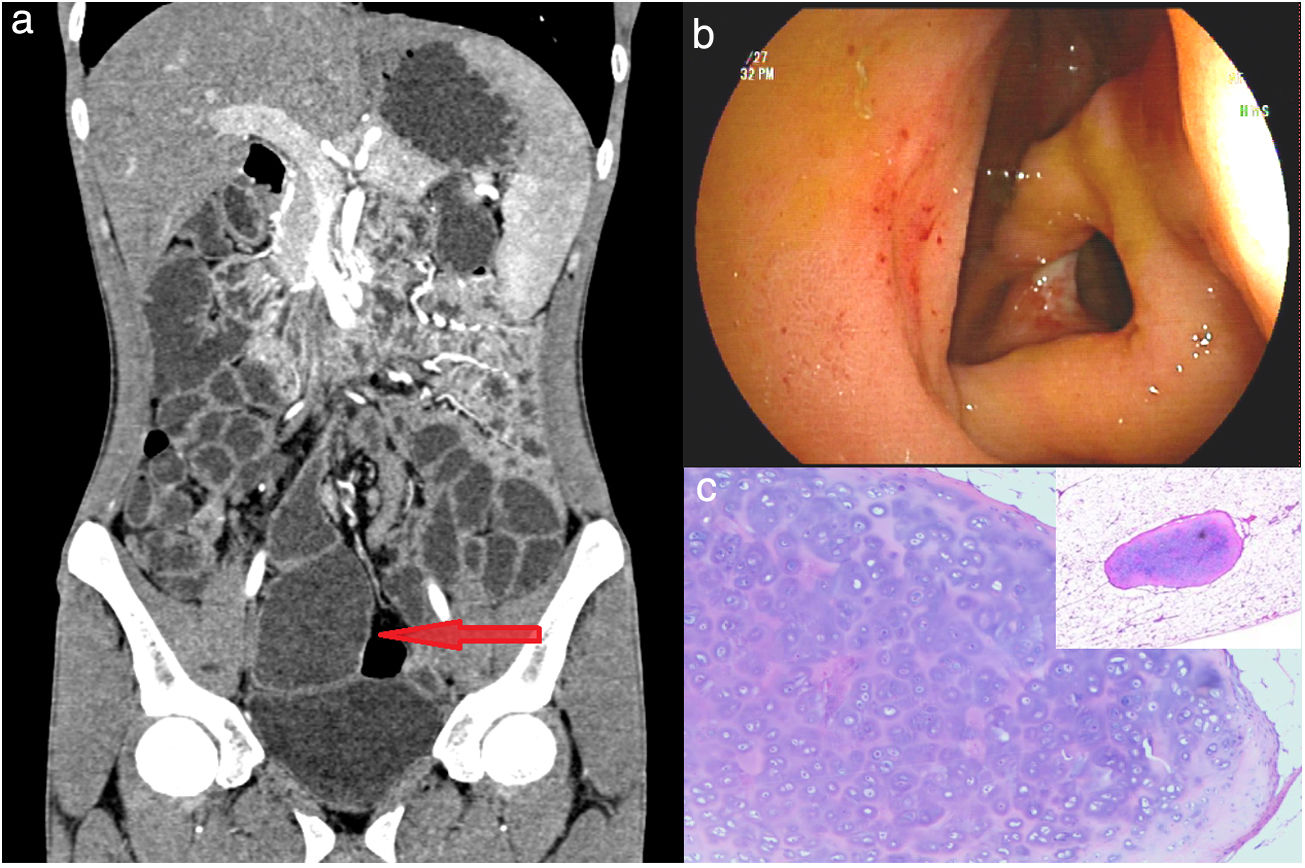
The major laboratory findings were as follows. White blood cell count, 6.21×109/L (normal range, 4–10×109/L); hemoglobin, 59g/L (normal range, 120–160g/L); platelet count, 595×109/L (normal range, 100–300×109/L); C-reactive protein, 3.21mg/L (normal range, <10mg/L); ferritin, 3.18ng/mL (normal range, 15–200ng/mL); erythropoietin, 213.44mIU/mL (normal range, 2.59–18.5mIU/mL); fecal occult blood test, positive (normally negative). Both bowel-wall thickening and luminal dilatation were detected by contrast-enhanced computed tomography (CT) scans of the small intestine (Fig. 1a, arrow). The patient then underwent double-balloon enteroscopy, when a circumferential ulcer was found in the middle part of the ileum where the bowel walls were edematous and accompanied by luminal stenosis, through which the endoscope was unable to pass (Fig. 1b). The patient underwent an exploratory laparotomy during which we noticed that there were cartilage, smooth muscles, fibrous tissue, and adipose tissue in the intestine wall. Based on the postoperative pathology, the possibility of hamartoma was considered (Fig. 1c).
Thickening and luminal dilatation were detected by the contrast-enhanced computed tomography scans of the small intestine (a, arrow). A circumferential ulcer was found in the middle part of the ileum where the bowel walls were edematous and accompanied by luminal stenosis (b). Postoperative pathology showed that there were cartilage, smooth muscles, fibrous tissue, and adipose tissue in the intestine wall (c).
Hamartoma, first reported by Albrecht in 1904, is usually considered to be a benign lesion related to the abnormal arrangement and location of normal tissues. Hamartoma involving the gastrointestinal tract is rare. Previous studies have reported four types of ileal hamartoma, namely neuromuscular and vascular hamartoma (NMVH), neuromesenchymal hamartoma (NMeH), myoepithelial hamartoma, and Cowden hamartomatous syndrome.
NMVH is an extremely rare benign lesion of the intestine. Only a few cases of which have been reported so far in the English literature. NMVH generally presents as localized foci and may cause recurrent obstructive, chronic gastrointestinal bleeding and iron-deficiency anemia. The characteristic histopathologic findings of NMVH include hyperplasia of various tissues such as nerves, vessels, and smooth muscle bundles. In our patient we observed other pathological features, namely fatty submucosal infiltration and generation of cartilage tissue. These alterations were also described by Salas et al.2 and Theodosiou et al.3 Cases with pathological features similar to NMVH but with additional mesenchymal tissues involvement were considered by Salas et al. to constitute a separate entity for which they proposed the alternative term of NMeH,1 whereas Theodosiou et al. tended to regard these two conditions as the same type of lesion.2 Some authors also reported cases of unknown small intestine ulcerations and strictures which they named cryptogenic multifocal ulcerating stenosing enteropathy (CMUSE), but it remains controversial whether CMUSE and NMVH are different terminologies used to explain the same pathology.3 Chronic non-specific multiple ulcers of the small intestine, which is exclusively reported from Japan, has clinical features similar to those of CMUSE and NMVH, although whether they are the same disease with different names is highly contentious.3 In addition, Ayyanar et al. found that ischemia resulting from vasculopathy appeared to be a direct cause of NMVH.4
In our case other pathological features, namely fatty submucosal infiltration and generation of cartilage tissue, were present, although nerve involvement was not found. We considered the possibility that this lesion may be a special type of mesenchymal hamartoma that also needs to be distinguished from non-granulomatous ulcerating jejunoileitis (NGUJI) and diaphragm disease (DD). For NGUJI, the main clinical manifestations are diarrhea and malabsorption3 while DD is considered characteristic of injury resulting from prolonged intake of non-steroidal anti-inflammatory drugs.5 Moreover, via endoscopy we observed transmural inflammation and an annular ulcer, which could readily be diagnosed as Crohn's disease. In fact, some scholars believed that NMVH is a special form of Crohn's disease, although the rarity of NMVH makes the histological diagnosis adebatable issue.
FundingThis work was financially supported by the grants from Suzhou “Science and Education” Youth Science and Technology Project (KJXW2020075), Wujiang science and technology research fund project (WWK201732), and The Scientific Research Project of Suzhou Ninth People's Hospital (YK202023).
Informed consentThe patient provided written informed consent for publication of the data in this study.
Author's contributionJiaqing Shen cared for the patient. Zhenguo Qiao and Wen Zhang wrote the paper. Yi Song was involved doing a literature search. Yi Song reviewed the manuscript. Jiaqing Shen was the guarantor of the overall content of the paper and submitted the paper. All authors read and approved the final version.
Conflict of interestAll authors have no conflicts of interest to disclose.
We thank Hugh McGonigle, from Liwen Bianji (Edanz) (www.liwenbianji.cn/ac), for editing the English text of a draft of the manuscript.