Bezoars are collections of indigestible foreign material that accumulate and coalesce in the gastrointestinal tract (usually the stomach). Phytobezoars, composed of vegetable matter, are the most common type of bezoar and they are rarely encountered in adults with a normal intestinal tract. Their formation may occur in patients with previous history of abdominal surgery or any other anatomical or physiological disorder altering gastric motility.
Superior mesenteric artery syndrome (SMAS) is an uncommon clinical entity characterised by compression of the third segment of the duodenum against the aorta by the superior mesenteric artery, which can cause a complete or partial duodenal obstruction. SMAS might often be overlooked in clinical practice. However, establishing the diagnosis is important because effective treatment may significantly improve the patient clinical condition and it can be a predisposing factor for other abnormalities and complications.
A 50-year-old vegetarian Armenian man presented with a long-term history of recurrent abdominal postprandial discomfort, early satiety, fullness and weight loss. Three days before admission, abdominal pain suddenly increased along with episodes of nausea and vomiting, leading to feeding intolerance. He had no history of eating disorders, drug abuse or previous abdominal surgery.
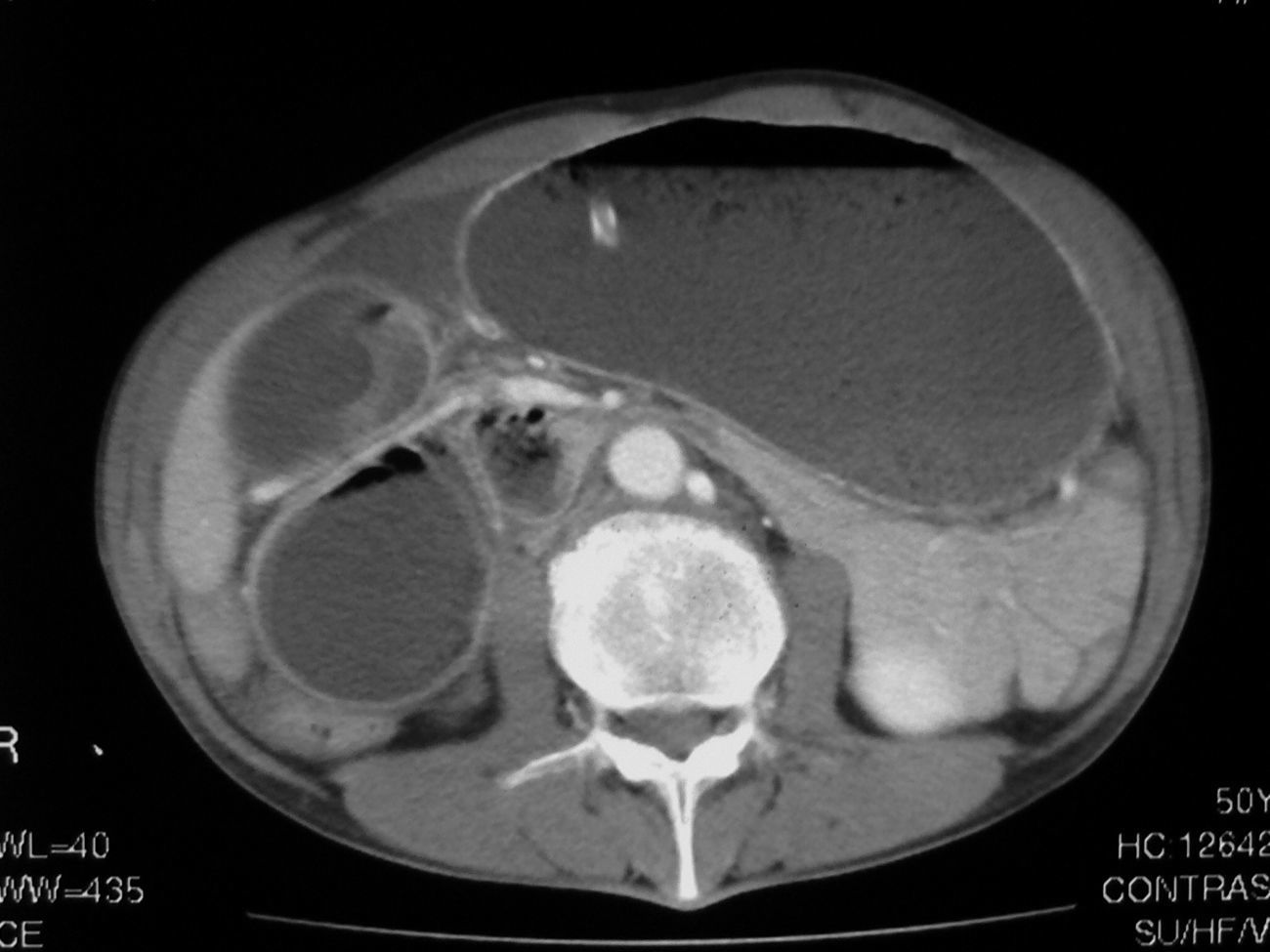
Clinical examination showed moderate dehydration and abdominal distension with diffuse tenderness. Laboratory-test results showed hemoconcentration and leukocytosis. Chest and abdominal plain radiography disclosed marked gastric dilatation with mild left pleural effusion. CT examination (Figs. 1 and 2) revealed fluid filled dilatation of the stomach and first and second parts of the duodenum. The third duodenal part showed abrupt vascular compression caused by the superior mesenteric artery (SMA), and it contained a well-defined non-homogeneus circular intraluminal mass of 3cm diameter with a mottled gas pattern. Collapsed loops of small bowel were seen immediately distal to the obstruction. Esophago-gastroduodenal endoscopy showed a semi-solid dark-greenish duodenal mass consisting of food particles and vegetable fibres. Mechanical disruption was attempted during endoscopy. Scattered ulceration and friability of the gastric and duodenal mucosa probably secondary to pressure necrosis were also found.
A nasogastric tube was inserted. Parenteral nutrition and intravenous treatment with proton-pump inhibitors were initiated. Gastric content was progressively removed and abdominal distension disappeared. An endoscopic study undertaken on the fifth day of hospitalization showed a reduction in gastro-duodenal dilatation and phytobezoar was not visible. Extrinsic compression continued to reduce the duodenal lumen but there were no signs of obstruction. Oral feeding was reintroduced and well tolerated. The patient was discharged with dietary counseling in order to avoid recurrences.
The angle of 45° formed by abdominal aorta and SMA is preserved due to the presence of fatty tissue around the duodenum and pancreas. Any factor that reduces this fatty tissue will narrow the angle and may potentially produce the entrapment and compression of the third part of duodenum, developing the so-called SMA syndrome. Its clinical presentation ranges between a casual radiological finding in asymptomatic subjects and a symptomatic intestinal obstruction1.
Conventional CT of the abdomen clearly depicts the abrupt extrinsic compression on the third portion of the duodenum by the SMA. Small bowel loops distal to the crossing point of the third portion of the duodenum and the SMA are collapsed. CT also rules out other pathologic processes that may mimic SMA syndrome. CT angiography with maximum intensity projection and 3D reconstruction is an useful non-invasive diagnostic technique that allows SMA visualization and its relationship with the abdominal aorta and duodenum2.
There is no standardized method to treat gastric phytobezoars but non-surgical measures such as endoscopic fragmentation and removal should be the initial approach3,4. Duodenal collections may often require surgery if the obstruction does not resolve promptly. On the other hand, the first line treatment of SMA syndrome is usually conservative although efficacy reported with this approach is limited5. Surgery should be considered for both entities when conservative measures are ineffective. Several surgical techniques have been described to treat SMA syndrome but the most successful procedure is duodenojejunostomy, using a laparoscopic approach when possible6.
In our case, both the SMA syndrome and the high fibre content in the patient's diet could have been predisposing factors contributing to phytobezoar formation. A decrease of alimentary intake as the result of obstructive symptoms may have contributed to weight loss and mesenteric fatty tissue reduction, accentuating the angle between the SMA and abdominal aorta. Conservative measures together with parenteral hyperalimentation successfully relieved intestinal obstruction in our patient. Endoscopic disruption of the phytobezoar was also attempted to promote spontaneous passage.