In this review we summarize the role of liver biopsy, transient elastography and hepatic venous pressure gradient (HVPG) in the diagnosis and monitoring of patients with liver cirrhosis. Transient elastography is useful for the non-invasive diagnosis of cirrhosis, but relevant information is lost if it is used as a dichotomous test. The development of clinically significant portal hypertension (defined as a hepatic venous pressure gradient ≥ 10mmHg) is associated with the development of varices and decompensation and it is something that it is worth testing for. Transient elastography has some value for the prediction of clinically significant portal hypertension, but a large proportion of patients have non-diagnostic values. It has also some value for the diagnosis of varices, but non-invasive markers cannot substitute endoscopic screening in cirrhosis. Better dynamic, easily repeatable non-invasive tools are needed to monitor compensated cirrhosis.
En esta revisión se resume la función de la biopsia hepática, la elastografía transitoria y el gradiente de presión venosa hepática en el diagnóstico y seguimiento de pacientes con cirrosis hepática. La elastografía transitoria es útil para el diagnóstico no invasivo de la cirrosis, pero se pierde información relevante cuando se utiliza como prueba dicotómica. El desarrollo de una hipertensión portal clínicamente significativa (definida como un gradiente de presión venosa hepática de ≥ 10mmHg) se asocia con el desarrollo de várices y descompensación, y merece la pena valorarlo. La elastografía transitoria tiene cierto valor para predecir una hipertensión portal clínicamente significativa, pero una gran proporción de pacientes presentan valores no diagnósticos. También es relativamente valiosa para el diagnóstico de varices, pero los marcadores de detección no invasivos no pueden sustituir al cribado endoscópico en la cirrosis. Son necesarias herramientas no invasivas más dinámicas y fácilmente repetibles para controlar la cirrosis compensada.
Liver cirrhosis is defined by anatomical changes within the liver parenchyma including fibrosis and the development of regenerating nodules. The appearance of cirrhosis is a hallmark in the natural history of chronic liver diseases. It indicates a worse prognosis, and it identifies the point to initiate surveillance for hepatocellular carcinoma and varices. Moreover, in patients with cirrhosis, the onset of clinically significant portal hypertension (CSPH, HVPG≥10mmHg) indicates a further step in the natural history which should be ideally recognized as soon as it appears. In this context, diagnostic methods are of outstanding importance, and their strengths and weaknesses should be recognized.
Brief description of the techniquesLiver biopsy has been used for decades for diagnosing and grading liver diseases, and to address therapeutic decisions.1 The liver is approached either by a percutaneous puncture or during transjugular hepatic vein catheterization; the latter approach is usually limited to patients with contraindication to the percutaneous approach such as major coagulopathy or ascites, since it was considered to be less satisfactory than percutaneous approach, because smaller, more fragmented and thinner samples are obtained. For diagnostic aims, a liver specimen of at least 15mm length, containing at least 6–8 complete portal tracts, should be present, being the ideal specimens of 20–25mm length or 11 complete portal tracts to reliably assess grading and staging, and to reduce sampling errors.2,3 Limitations of liver biopsy include its invasiveness, which can lead, even if rarely, to major complications, and the limited amount of liver tissue; in fact, even if of optimal length, liver biopsy specimens only represent about 1/50,000 of the liver parenchyma.
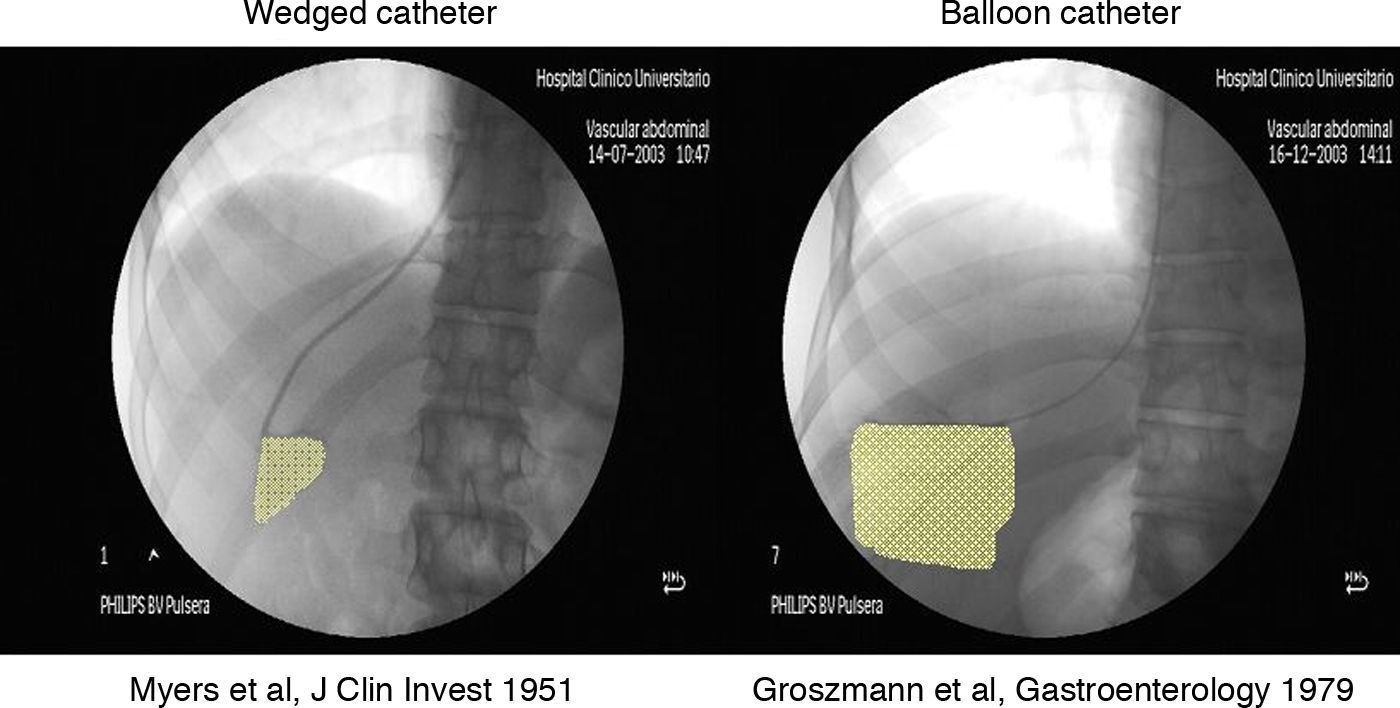
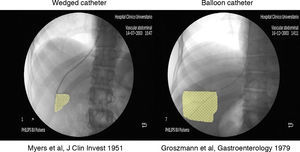
Hepatic vein catheterization with measurement of the hepatic venous pressure gradient (HVPG) is currently the gold standard technique for determining portal pressure. It is calculated as the difference between the wedged hepatic venous pressure (WHVP) and the free hepatic venous pressure (FHVP).4 The WHVP is measured by occluding a main hepatic vein; stopping the blood flow causes the static column of blood to transmit the pressure that is present in the preceding vascular territory – in this case, the hepatic sinusoids, which in the absence of pre-sinusoidal obstruction, reflects portal pressure. The hepatic vein can be occluded either by ‘wedging’ the catheter into a small branch of a hepatic vein or by inflating a balloon at the tip of the catheter (Fig. 1), but the occlusion of the hepatic vein by inflating a balloon is preferred, as the volume of the liver circulation transmitting portal pressure is much larger than that attained by wedging the catheter, which reduces the variability of the measurements.5 It has been shown that the WHVP gives an accurate estimate of portal pressure in alcoholic and viral cirrhosis.4,6 The FHVP, as its name suggests, is a measure of the pressure of unoccluded hepatic vein; our group recently provided evidence to support the use of FHVP and not of right atrial pressure (which was commonly used by interventional radiologists) to calculate the hepatic venous pressure gradient, since the latter shows a worse correlation with clinical outcomes.7 Guidelines for reliable HVPG measurements have been recently published,4,8,9 but HVPG stills lacks widespread standardization. Liver catheterization allows performing in the same procedure a transjugular liver biopsy.
Since HVPG reflects portal pressure, changes in HVPG mirror changes in the factors that determine portal pressure, namely hepatic vascular resistance, collateral resistance and portal blood flow inflow.10 Changes in hepatic resistance can be caused by changes in fibrosis, regenerative nodules or appearance of thrombosis (mechanical factors) or by a change in hepatic vascular tone (dynamic factors).10 Therefore, HVPG estimates, to a certain extent, the degree of liver fibrosis, but integrates in a single measurement the effects of very different pathogenic events occurring in liver diseases.
Given that biopsy and HVPG are invasive methods, in recent years a large amount of investigation has been devoted to the development of non-invasive methods for the evaluation of the liver diseases. Most of them initially mainly focused patients with viral hepatitis, majorly hepatitis C, with the aim of detecting the presence of “significant fibrosis” or cirrhosis, since these have prognostic and therapeutic implications. Among them, transient elastography (Fibroscan®) has been the most extensively evaluated.11
Transient elastography (TE, Fibroscan®, Echosens, Paris, France) equipment consists in a 5MHz ultrasound transducer probe mounted on the axis of a vibrator. Mild amplitude and low frequency vibrations (50Hz) are transmitted to the liver tissue, inducing an elastic shear wave that propagates through the underlying liver tissue. Pulse-echo ultrasonic acquisitions are performed to follow the shear wave and measure its speed. The velocity of propagation of the wave is directly related to the tissue stiffness (the harder the tissue, the faster the shear propagates), which is measured in kilo Pascals (kPa).12 TE is rapid (5min), reproducible and acquires information from a much larger portion of the tissue as compared to liver biopsy (a cylinder of 1cm diameter and a length of 4cm, 100 times larger than the biopsy specimen). Thus, the risk of sampling error is significantly lower. The quality criteria to consider a measurement reliable are at least 10 successful acquisitions and a success rate of at least 60%. In addition, the interquartile range (IQR) of all validated measurements should be less than 30% of the median value. One of the main limitations of the technique is that in about 15–20% of the patients it gives uninterpretable results,13–15 mainly related to the presence of obesity.15 A new type of probe (not yet fully validated) might overcome this problem. Factors different from fibrosis might influence liver stiffness values. Inflammation, cholestasis and liver congestion increase liver stiffness.
Diagnosis of cirrhosisLiver biopsy is considered the gold standard for the diagnosis of cirrhosis, but, as previously mentioned, it has important limitations, such as being invasive, having the potential for complications, false-negative results or underestimation of the disease severity due to sampling error and inter and intra-observer variability. Due to these factors, the interpretation of liver biopsy might be especially difficult in cases of macronodular cirrhosis.
Ultrasound (US) is usually the first imaging method used in patients with suspected cirrhosis,16 as it is non-invasive and widely available. Liver surface nodularity, especially when evaluated by high-frequency, linear array transducers, is the most accurate sign of cirrhosis; the clinical suspicion can be further reinforced by a decreased portal blood velocity, or by the presence of specific signs of portal hypertension. US accuracy, however, depends on the experience of the operator, and it is difficult to apply routinely in the follow-up of all patients with chronic hepatitis. Simpler, faster, and more reproducible non-invasive tests would be desirable.
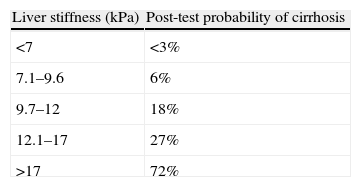
Transient elastography has been extensively evaluated in the diagnosis of cirrhosis in patients with chronic hepatitis C, and less extensively in patients with other etiologies.17–21 It has been shown to be better than other non-invasive markers.22 In practically all studies it was found to be better to diagnose cirrhosis (F4) than to diagnose significant fibrosis (≥F2), although this might be related to the spectrum of patients included in these studies (low prevalence of cirrhosis). Most studies have reported best cut-offs for the diagnosis of cirrhosis between 12 and 15kPa. A meta-analysis including 50 studies found 13kPa to be the best one.23 The methodologies to select these cut-offs seem to favour sensitivity over specificity, which is a sensible strategy in a test used for screening, where the main purpose is to “rule-out” cirrhosis. However, the use of a single cut-off clearly limits the diagnostic potential of Fibroscan, which provides continuous values.24 For example, if the 13kPa cut-off is chosen, patients with a liver stiffness value of 13.5kPa would be classified as having cirrhosis, and would be treated as identical to those with a value of 40kPa, but differently from those with a value of 12.5kPa. The information provided by transient elastography would be improved with appropriate multilevel or continuous likelihood ratios,25 by accounting for the increasing likelihood of cirrhosis with increasing liver stiffness. The use of multi-level likelihood ratios26 (in which liver stiffness values are divided in a number of categories, rather than dichotomized) could offer a more reasonable use of Fibroscan in clinical practice. The likelihood ratio of cirrhosis for a certain stiffness value or category would be the probability that a patient with cirrhosis has that stiffness value or category, compared to the probability that a patient without cirrhosis has that same result. Likelihood ratios permit the calculation of post-test probabilities given a certain pre-test probability (in this case the prevalence of cirrhosis in the studied population). Table 1 shows an example of how multilevel likelihood ratios could be used in this setting, with data taken from the Fibrostic study,13 a multicentre study including 1307 patients with viral hepatitis. Only values below 7kPa reliably ruled-out cirrhosis, and only values above 17kPa were good enough to rule-in cirrhosis. Forty percent of the patients had intermediate values.
Post-test probabilities of cirrhosis (prevalence of cirrhosis: 14%), according to Fibroscan values (from the Fibrostic study, Degos et al.13).
| Liver stiffness (kPa) | Post-test probability of cirrhosis |
| <7 | <3% |
| 7.1–9.6 | 6% |
| 9.7–12 | 18% |
| 12.1–17 | 27% |
| >17 | 72% |
Since Fibroscan provides continuous values the ideal would be to use continuous likelihood ratios, since they convey the most clinical information for assessing the impact of individual test results.25 In this way, any given liver stiffness value would be associated with a likelihood ratio, and a post-test probability of cirrhosis could be calculated for any given liver stiffness value knowing the pre-test probability. This should not be a problem in real-life practice, in which physicians are increasingly used to calculate complex scores. For a robust modelling of continuous likelihood ratios a large number of patients with and without cirrhosis would be required. This large sample could be achieved in an individual-patient meta-analysis of the already published studies.
The combination of different methodologies could increase the diagnostic potential of non-invasive tools. A recent study, performed in 90 patients with clinically doubtful cirrhosis, showed that the combination of liver stiffness with left lobe liver surface (LLS) ultrasound was better for the diagnosis of cirrhosis and substantially decreased the number of indeterminate results of either technique alone.14 Fibroscan was better than LLS ultrasound in ruling out cirrhosis, whilst LLS ultrasound was better to rule it in. Their combination offered the best diagnostic performance, since the two techniques essentially give complementary information on two different anatomical factors of cirrhosis, namely the severity of fibrosis, and the presence of nodularity.
The role of HVPG in the diagnosis of cirrhosis is basically the confirmation of the presence of sinusoidal portal hypertension27; values above 5mmHg should be considered increased, and values above 10mmHg indicate the presence of clinically significant portal hypertension, which holds negative prognostic implications (see below). From a clinical point of view, HVPG should be used to identify the cause of portal hypertension, and to reinforce the diagnosis of cirrhosis whenever another etiology of the liver alteration is suspected (e.g. idiopathic portal hypertension or nodular regenerative hyperplasia).4 It should be underlined that during hepatic vein catheterization a transjugular liver biopsy can be performed, so adding histological information to those obtained by the hemodynamic evaluation.
Monitoring cirrhosisPatients with cirrhosis have a long period of compensated disease, in which symptoms are minimal or completely absent.28 The key events that can occur in a compensated patient, and that should be predicted, are the appearance of varices, the development of clinical decompensation (ascites, variceal bleeding, infections, encephalopathy, jaundice) and hepatocellular carcinoma (HCC). There are few tools to monitor these patients along this compensated stage.
The main driving force for the development of varices and clinical decompensation is the progressive increase in portal pressure. Varices do not appear whilst HVPG remains below 10mmHg.29 The increase in HVPG over 10mmHg a major risk factor for the development of varices30 and decompensation,31 and it is also associated with an increased risk of HCC.32 Thus, this value has been used to define clinically significant portal hypertension (CSPH). Development of CSPH could be used as an intermediate surrogate endpoint of disease progression in patients with early, compensated cirrhosis, and therefore it is something that it is worth testing for. On the other hand recent studies have pointed out that liver stiffness, by itself, can predict clinical endpoints, such as HCC33,34 and cirrhosis decompensation.35
Clinically significant portal hypertensionHVPG measurement is the gold standard to diagnose CSPH. Some findings in liver biopsy could suggest the presence of CSPH. In a study performed in 43 cirrhotic patients small nodule size and increased septal thickness were associated with CSPH.36
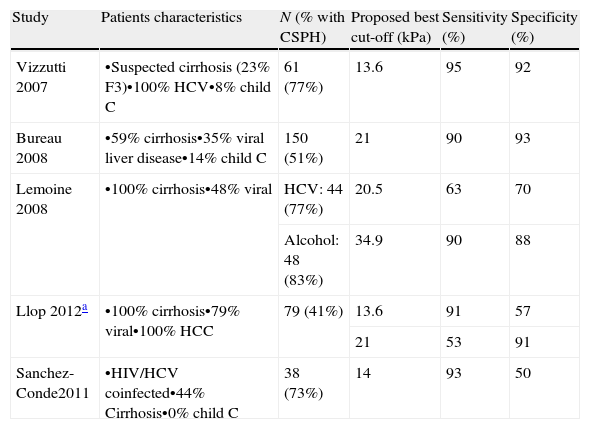
Liver stiffness values have been shown to correlate with HVPG.37–42 This correlation is good in HVPG values up to 10mmHg, but it is much worse above these values,41 reflecting that in advanced portal hypertension the contribution of extrahepatic factors (such as the increase in blood flow due to hyperdynamic circulation) to portal pressure is prominent. Five studies up to now reported the accuracy of transient elastography for the prediction of CSPH.38–42 These studies were performed in patients with different disease severity and with different proportion of viral cirrhosis. One of them40 evaluated the performance of TE in one of the settings in which the presence of CSPH changes the management of the patient, i.e., in patients with well-compensated cirrhosis and a single nodule of HCC (candidates to liver resection). The “best” cut-offs to predict CSPH were rather different (Table 2). In the study by Llop et al. multilevel likelihood ratios were used. This study showed that a cut-off of 13.6kPa was sensitive enough to rule-out CSPH, and a cut-off of 21 was specific enough to rule-in CSPH. Values in between these limits (which were found in 35% of the patients) were not useful. Again, it is clear that the use of a single TE cut-off, though simple, limits the value of TE to predict CSPH. The use of at least two cut-offs reproduces well the clinical thinking in which a diagnostic test commonly gives 3 outputs: the condition is ruled-in, ruled-out or “further tests are needed”.
Studies assessing the diagnostic value of transient elastography to predict clinically significant portal hypertension (CSPH).
| Study | Patients characteristics | N (% with CSPH) | Proposed best cut-off (kPa) | Sensitivity (%) | Specificity (%) |
| Vizzutti 2007 | •Suspected cirrhosis (23% F3)•100% HCV•8% child C | 61 (77%) | 13.6 | 95 | 92 |
| Bureau 2008 | •59% cirrhosis•35% viral liver disease•14% child C | 150 (51%) | 21 | 90 | 93 |
| Lemoine 2008 | •100% cirrhosis•48% viral | HCV: 44 (77%) | 20.5 | 63 | 70 |
| Alcohol: 48 (83%) | 34.9 | 90 | 88 | ||
| Llop 2012a | •100% cirrhosis•79% viral•100% HCC | 79 (41%) | 13.6 | 91 | 57 |
| 21 | 53 | 91 | |||
| Sanchez-Conde2011 | •HIV/HCV coinfected•44% Cirrhosis•0% child C | 38 (73%) | 14 | 93 | 50 |
HCV: hepatitis C virus; HCC: hepatocellular carcinoma.
Very recently, newer methods for estimating stiffness in real time during a normal ultrasound examination have been commercialized. Among them, initial data show that acoustic radiation force imaging (ARFI) holds a similar accuracy as TE in predicting significant fibrosis and cirrhosis.43 These new methods allow measuring stiffness not only within the liver, but also in the spleen. Preliminary evidence suggests that spleen stiffness may reflect more accurately portal hypertension.44
VaricesAll patients with cirrhosis should be screened with upper endoscopy for the presence of varices. This recommendation has not been changed in the latest consensus conference on the management of portal hypertension (Baveno V).45 The presence of varices is indicative, by itself, of the presence of CSPH, and it is a marker of disease progression, since it is associated with increased risk of decompensation31 and impaired prognosis.46 Apart from being a prognostic marker, the diagnosis of varices is relevant since there are effective treatments for the prevention of bleeding (beta-adrenergic blockers and endoscopic banding ligation). Decision on whether the patient needs prophylaxis is based on the size of the varices, the presence of red signs and Child-Pugh class.45 Therefore, for prognostic purposes and for therapeutic decisions, the aim of a non-invasive test should be to detect varices of any size.
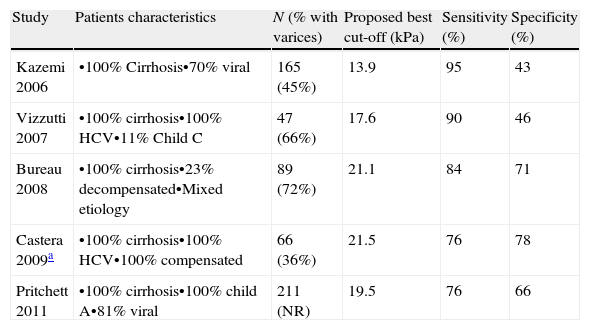
Transient elastography has been assessed as a non-invasive method to predict varices.22,41,47–49 Again, different liver stiffness cut-offs were proposed (Table 3). These differences can be mostly attributed to the methodology for selecting the “best” cut-off (favouring sensitivity or specificity). For screening purposes, in which the aim is to reliably rule-out the presence of varices, a sensitive cut-off should be selected. This would be around 14kPa, which is closely similar to that for the diagnosis of cirrhosis. Therefore, once the diagnosis of cirrhosis is established, transient elastography is unlikely to be useful in the screening of varices. On the other hand, none of these cut-offs were specific enough to reliably rule-in varices.
Performance of transient elastography in the prediction of varices (any size).
| Study | Patients characteristics | N (% with varices) | Proposed best cut-off (kPa) | Sensitivity (%) | Specificity (%) |
| Kazemi 2006 | •100% Cirrhosis•70% viral | 165 (45%) | 13.9 | 95 | 43 |
| Vizzutti 2007 | •100% cirrhosis•100% HCV•11% Child C | 47 (66%) | 17.6 | 90 | 46 |
| Bureau 2008 | •100% cirrhosis•23% decompensated•Mixed etiology | 89 (72%) | 21.1 | 84 | 71 |
| Castera 2009a | •100% cirrhosis•100% HCV•100% compensated | 66 (36%) | 21.5 | 76 | 78 |
| Pritchett 2011 | •100% cirrhosis•100% child A•81% viral | 211 (NR) | 19.5 | 76 | 66 |
HCV: hepatitis C virus.
The combination of non-invasive methods could provide a higher accuracy in the prediction of varices as compared to a single method. A recent study in patients with compensated chronic hepatitis B suggested that the combination of liver stiffness (measured by Fibroscan), spleen size (measured by ultrasound) and platelet count is very accurate in predicting the presence of any varices, high risk varices and variceal bleeding.50,51 Appropiate validation in independent cohorts is needed.
Response to treatmentLiver cirrhosis might improve with etiological treatments (antivirals, alcohol abstinence, flebotomies, cupper chelators, steroids, etc.), but in well-compensated patients this is difficult to measure. It is not easy to define what constitutes an improvement in compensated cirrhosis. In patients with varices, disappearance of varices is a clear sign of improvement.
Liver biopsy can show a decrease in fibrosis, but sampling issues and subjective assessment makes difficult the interpretation of this information. This might be improved by computer-assisted digital image analysis,52 but more data are needed. Some reports suggest true histological regression of cirrhosis. Whilst it is clear that the amount of fibrosis might be decreased, it is much less clear whether the angioarchitectural changes of cirrhosis might truly regress.53 In any case, in the studies showing cirrhosis regression in viral hepatitis this was associated with a marked decrease in the risk of liver-related death.54
There is no information on whether changes in transient elastography might be useful to monitor an improvement in cirrhosis. Preliminary reports suggest that after successful antiviral treatment liver stiffness decreases, but more information is needed. A few studies have evaluated the changes in HVPG after antiviral treatment in cirrhosis showing a decrease in portal pressure,55,56 especially in patients achieving a sustained viral response. A very relevant issue, not yet well defined, is what constitutes a relevant decrease in portal pressure in this setting. In patients with cirrhosis but a baseline HVPG below 10 (i.e., without CSPH), lack of progression to CSPH would clearly be a desirable response. In addition, data from the Timolol trial, which included well compensated patients with cirrhosis and without varices (63% with CSPH at baseline), showed that a 10% decrease in HVPG was associated with a decreased risk of developing varices30 and decompensation.31 Interestingly enough, the risk of developing varices was similarly low (35% at 6 years) if a good response was defined as “>10% decrease in HVPG”, or if a good response was defined as “lack of increase in HVPG by more than 10%”. Therefore, in a mixed population of compensated patients with and without CSPH the definition of response should take into account that lack of progression to CSPH is a good response, and limiting the definition to 10% decrease in HVPG is probably inadequate.
Regarding the risk of variceal bleeding, it is well established that in patients with varices these do not bleed if HVPG does not go over 12mmHg. If HVPG decreases below 12mmHg (spontaneously or with non-selective beta-blockers) the patient is totally protected from variceal bleeding.30 Additionally, a 10%57 or 20%58 HVPG decrease from baseline has been associated with a relevant decrease in the risk of bleeding. However, only half of the patients treated with beta-blockers achieve these goals, and haemodynamic response cannot be predicted non-invasively. With respect to other complications of cirrhosis, it is still unknown whether reversal to a HVPG below 10mmHg totally protects from ascites and decreases the risk of HCC. A large ongoing placebo-controlled trial comparing beta-blockers vs placebo for the prevention of decompensation will further clarify some of these issues (NCT01059396). In addition, the number of patients with HCV cirrhosis treated with antivirals will surely increase after the approval of direct antiviral agents. This will offer a good opportunity to further evaluate HVPG response as a surrogate end-point in this setting.
There are a lot of expectations on the development of antifibrotic drugs. One of the factors that have slowed down their development has been the difficulty in defining good surrogates in a compensated population in which the rate of clinical end-points is very low. A well defined HVPG response could be an excellent surrogate. However, less invasive, easily repeatable methods would be clearly more acceptable by the pharmaceutical companies developing these drugs and by regulatory agencies. The elusive non-invasive portal sphygmomanometer is still badly needed.
FundingSupported in part by a grant from the Instituto de Salud Carlos III (FIS PI11/00883 to JGA), and co-financed by FEDER funds (Fondo Europeo de Desarrollo Regional. Unión Europea. “Una manera de hacer Europa”). Ciberehd is funded by Instituto de Salud Carlos III.
Conflict of interestThe authors declare no conflict of interest.