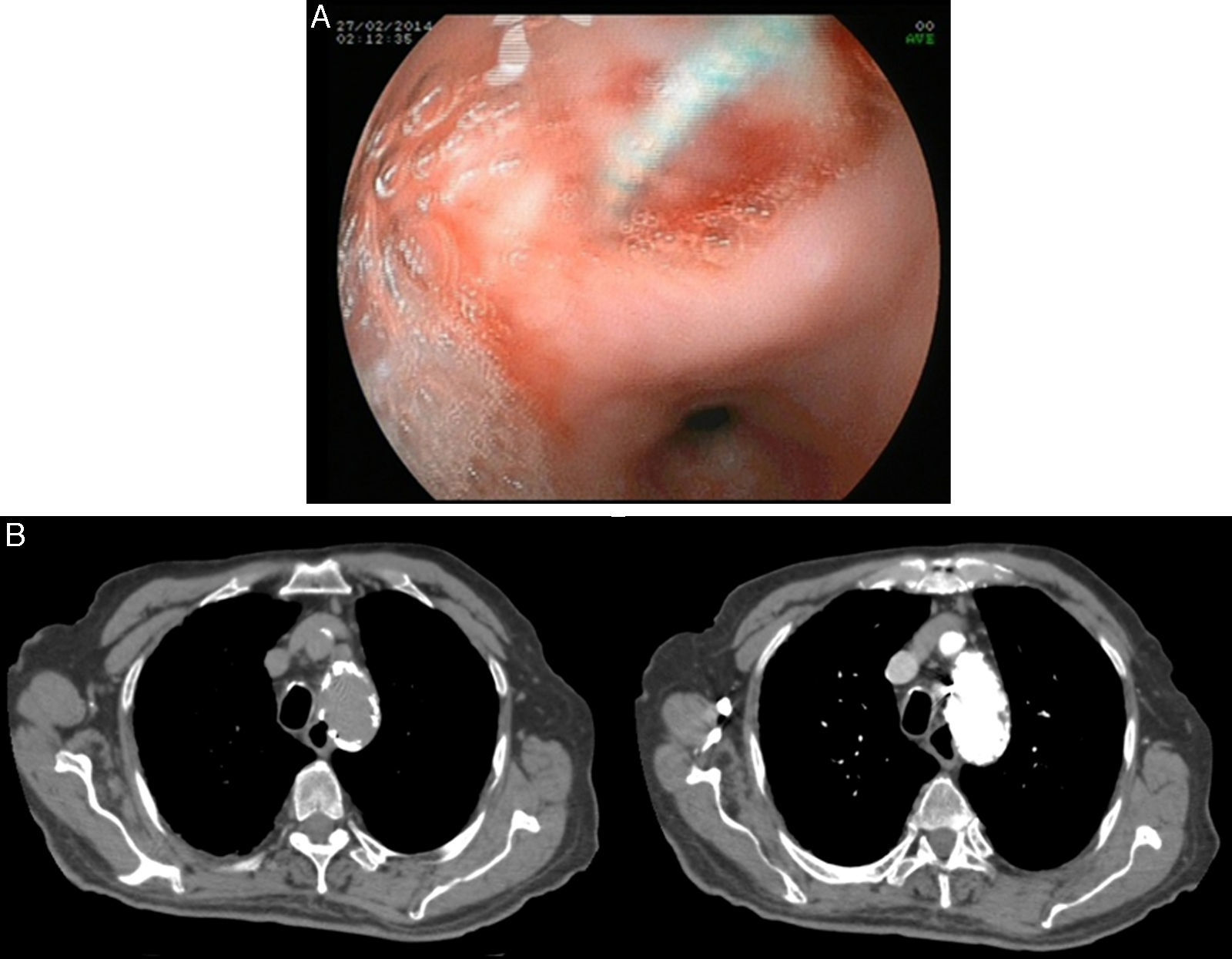
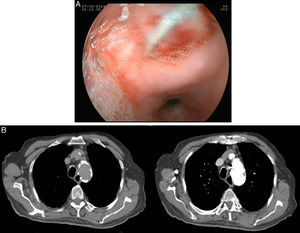
An 81-year-old man presented with progressive dysphagia to solid foods, odynophagia, and signs of upper gastrointestinal bleeding. Past medical history includes: (a) chronic ischemic cardiomyopathy treated with angioplasty and stent, (b) Leriche syndrome diagnosed 3 years before, (c) thoracic aortic aneurysm treated 12 months before with an endoprosthesis (Valiant®) placed through abdominal aorta. Vital signs were normal range on presentation, as well as physical examination. Initial chest X-ray showed a mediastinal widening. Laboratory data were significant only for hemoglobin (10.3g/dl). Urgent upper digestive endoscopy was performed within 12h (Fig. 1A). It showed a pseudodiverticula in the upper third esophagus with a silver, wire shaped foreign body emerging from inside. Initially he was treated conservatively without any endoscopic treatment. To confirm the suspect of a metallic foreign body and to discard any other mediastinal complications, a thoracic computer tomography (CT) was performed (Fig. 1B). An aortic stent was in intimate contact and penetrating into the esophagus lumen, without any evidence of pneumomediastinum or other complications. Taking into account the comorbidities and the high surgical risk, conservative approach was decided and accepted by the patient. He was suggested to eat soft, well-chewed food with frequent liquid gulps during meals. Esophageal symptoms have had mild improvement and weight keeps stable in the 9 months of follow-up.
Endovascular treatment of thoracic aneurysm with endoprosthesis has become the first therapeutic choice.1 Complications with endoprosthesis include: (a) ischemia (depending on the occluded artery by the extreme of the stent); (b) endoleak (persistence of blood flow outside the lumen of the endoluminal graft but within the aneurysm sac); (c) access complications (pseudoaneurysm, bleeding, pain); (d) post-implantation syndrome; (e) device migration; (f) aorto-esophageal fistula (AOF).1,2 In our case, an AOF was first suspected with the upper endoscopy and then confirmed with CT, which also discarded any other mediastinal complications. AOF is a rare and early (median of 90 days) complication of thoracic endovascular aortic repair (TEVAR).1,2 The European Registry of Endovascular Aortic Repair Complications has reported an incidence of 1.5%.1 AOF usually presents with fever (81%), hematemesis (53%), shock (6%) or dyspnea (6%).1 Conservative approach, offered to patients who refuse surgery or as a palliative option, is lethal with 100% of mortality within two years of follow-up, mainly due to bleeding. Moreover AOF frequently results in prosthesis related infections, which worsen the prognosis. The only durable and successful approach to cure the disease is radical esophagectomy and extensive aortic reconstruction. However, surgical repair is usually not possible because of patients being elderly and comorbidities.
Differential diagnosis of dysphagia and hematemesis includes: (a) foreign bodies with mucosal erosions’ ulcers, (b) hiatus hernia complications (Cameron's lesions), (c) diverticula bleeding, (d) large esophageal varices, (e) acute esophageal necrosis (black esophagus), (f) aorto-esophageal fistula. This case illustrates that a deep anamnesis may allow physicians to consider all diagnosis before additional tests are performed.
Conflict of interestThe authors who have taken part in this study declared that they do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.