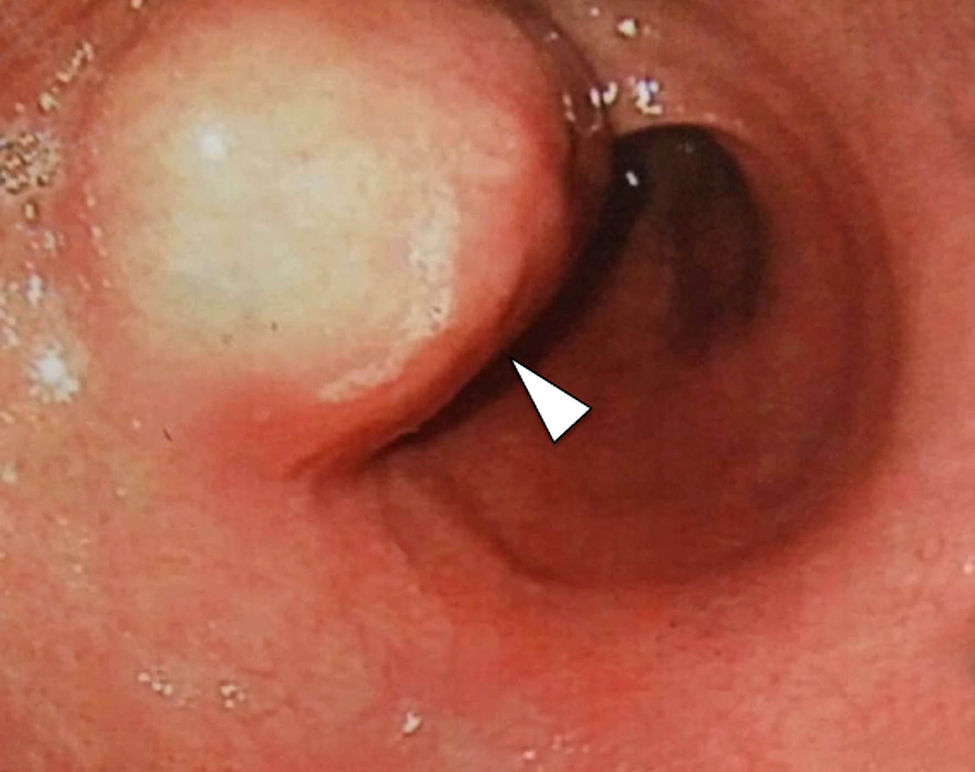
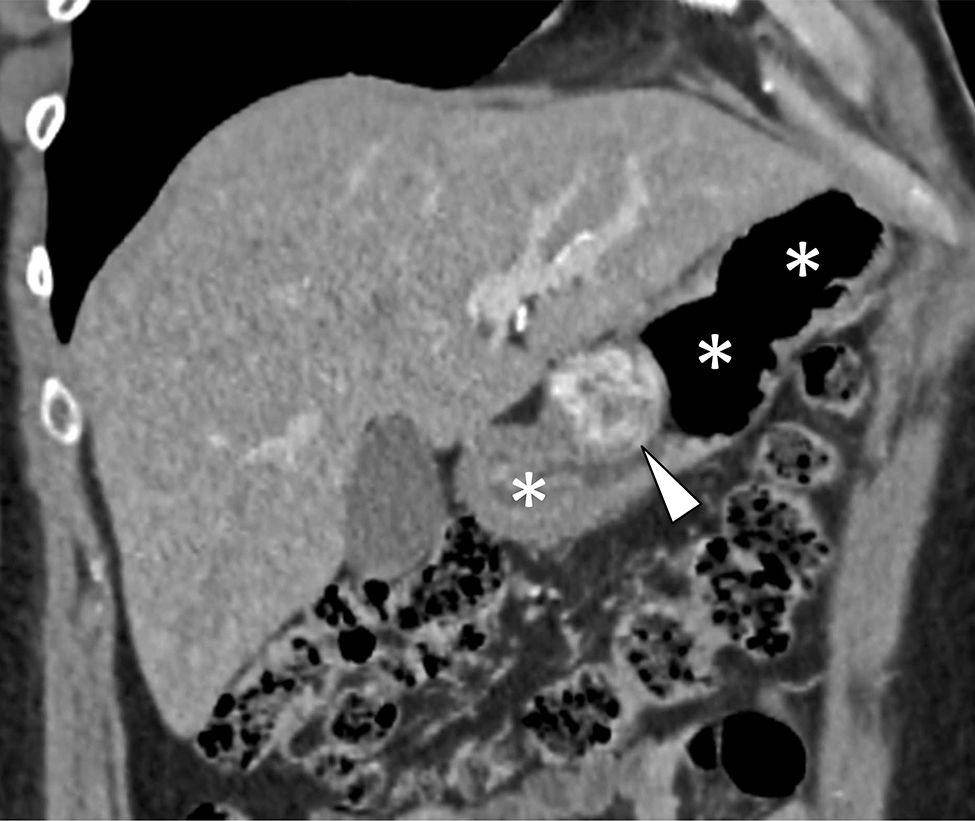
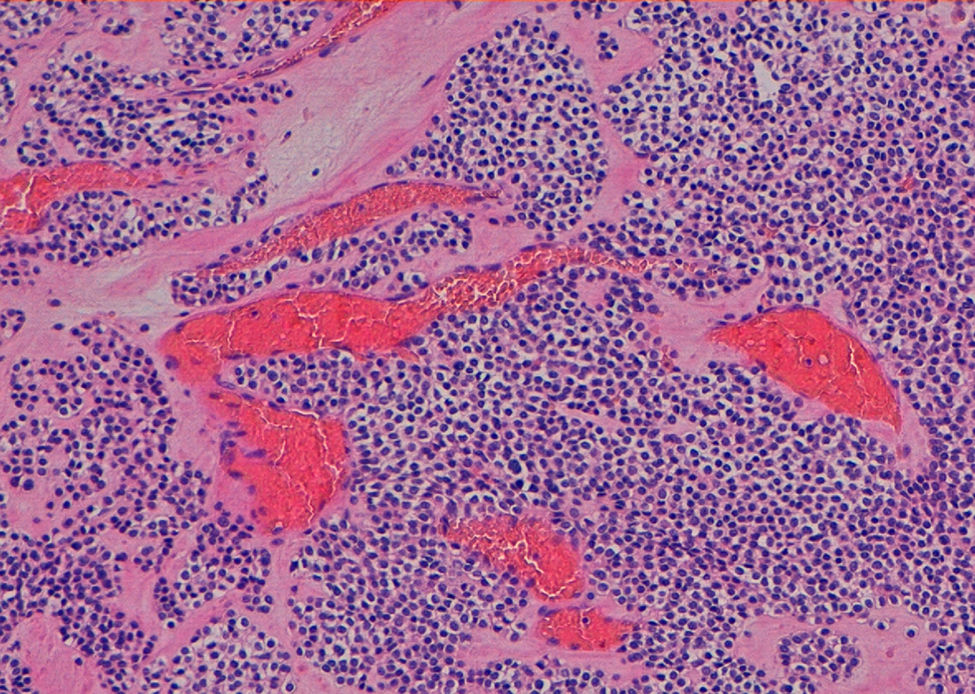
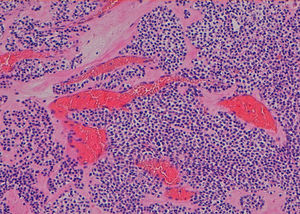
A 49-year-old man has been evaluated in our hospital for intermittent increasing epigastric discomfort over a 6-month period. No nausea or vomiting was noted. At the time of his presentation hematological examinations were within the normal limits. Gastro-duodenal endoscopy showed a round protruding lesion at the level of the gastric antrum (Fig. 1). Abdominal multi-detector computed tomography (MD-CT) revealed at the level of the gastric antrum an intraluminal subepithelial mass, with high vascular enhancement and 4-cm in diameter (Figs. 2 and 3). No other abdominal nodules or lymph nodes were noted. Patient underwent wedge resection. Histopathological evaluation demonstrated negative margin of the resection, and the mass was characterized by smooth muscle fibers, a jalinic stroma, a conspicuous vascular network and negative for cytokeratin and CD56 determining the diagnosis of a glomus tumor (Fig. 4). Given the benign diagnosis, the patient has been enrolled in clinical, laboratory and imaging follow-up program.
Gastric glomus tumor is a rare benign mesenchymal high vascular tumors arising from the glomus bodies.1,2 It constitutes about 1% of all benign gastric tumor.1–3 Typically, they are located in gastric antrum, as solitary, intraluminal subepithelial mass that are generally smaller than 3-cm in diameter.1–3 Gastrointestinal bleeding (hematemesis/melena) and epigastric discomfort are the most two common initial symptoms/signs.1–3 Gastro-duodenal endoscopy, endoscopic ultrasond, MD-CT and biopsy are generally the diagnostic procedure before surgery therapeutic treatment.2
Authors’ contributionsUmberto G. Rossi, MD, EBIR: write paper, diagnosis, images.
Mariangela Rutigliani, MD: review paper, diagnosis, image.
Francesco Paparo, MD: review paper, diagnosis.
Marco Filauro, MD: contribution to write paper, treatment.
FundingThe authors declare that there is no financing plan.
Conflict of interestThe authors declare that there is no conflict of interest.