Lanthanum carbonate is a drug frequently used in patients with end-stage renal disease and hyperphosphataemia.1,2 It is an alkaline heavy metal that works by binding dietary phosphorus in the stomach (optimally at pH 3 to 5), forming an insoluble complex that is excreted predominantly in stool, being the kidney and bile excretion almost none.1,3 In a small percentage of patients (0.00127% of cases), lanthanum is absorbed and deposited in the gastrointestinal tract, being the stomach and duodenum the most frequent locations.4
We describe the case of a 51-year-old man with a medical history of hypertension, end-stage renal disease undergoing haemodialysis and severe hyperparathyroidism. The patient was not on any anticoagulant or antiplatelet therapy, but was taking lanthanum (1000mg, 3 times daily) for hyperphosphataemia related to chronic kidney disease for many years.
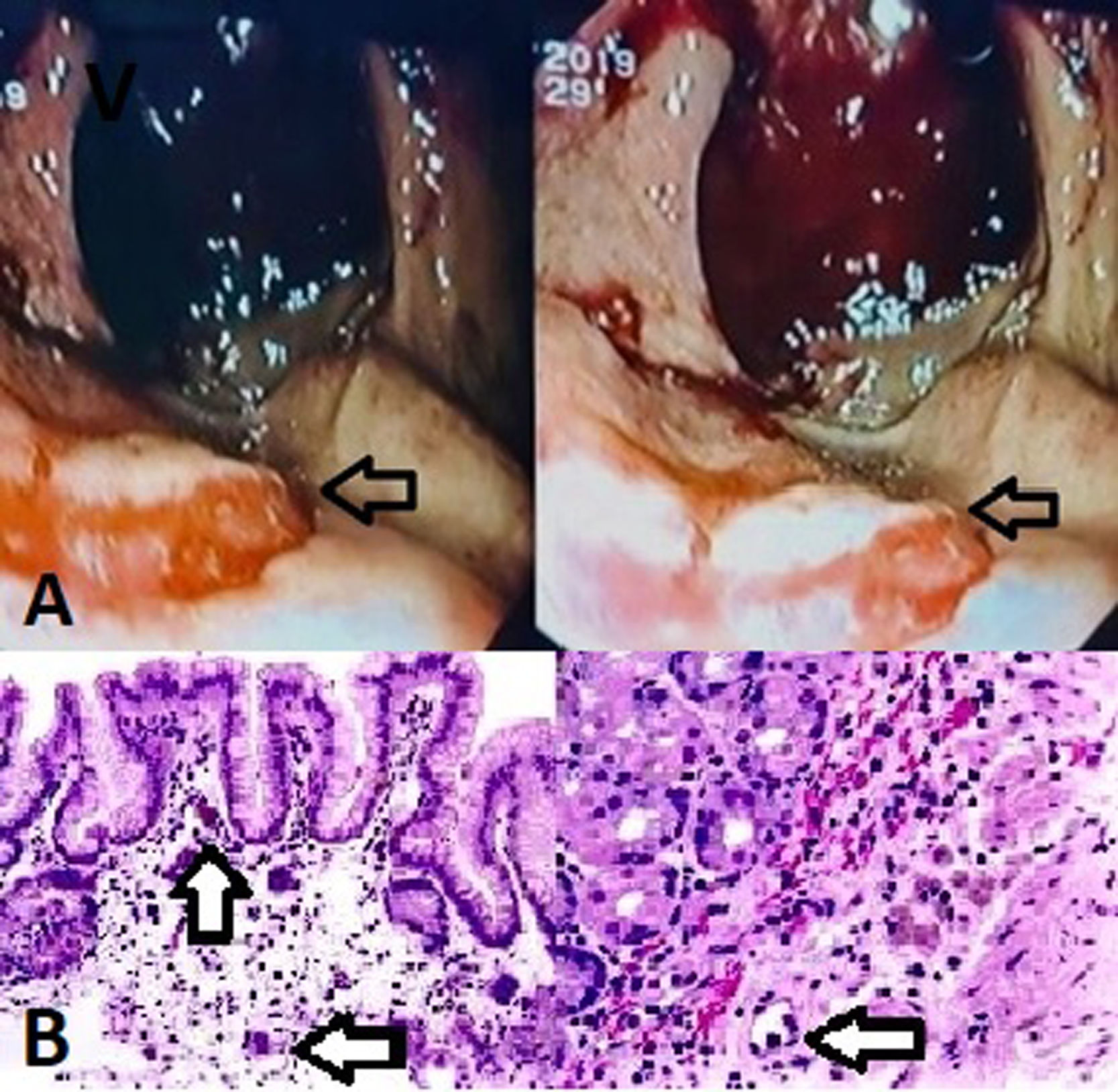
He presented to the emergency department with hematemesis, loss of consciousness and hemodinamic instability. The patient denied having taken nonsteroidal anti-inflammatory drugs or proton pump inhibitors. Laboratory analysis showed severe anemia (hemoglobin 5.3g/dL). Abdominal CT angiography was performed, showing active arterial bleeding from the posterior surface of the stomach. Esophagogastroduodenoscopy (EGD) revealed a non-removable clot on the fundus and greater curvature of the stomach, with underlying active bleeding. After several endoscopic attempts to stop bleeding without success and due to the hemodynamic compromise of the patient, surgical treatment was carried out. Intraoperative EGD was done to identify the bleeding point, observing an erythematous lesion with central whitish mucosa in the posterior gastric surface (Fig. 1A). Atypical gastrectomy was performed by excision of the bleeding lesion.
(A) Gastroscopy image in retroversion, which shows abundant blood content as well as an erythematous lesion with a central whitish area (black arrow). (B) Hematoxylin-Eosin stain. We observed histiocyte aggregates and multinucleated giant cells, with deposition of a dark intracytoplasmic material and expansion of the lamina propia (black arrow).
The histopathological study of the lesion revealed foveolar hyperplasia with prominent histiocytosis and multinucleated giant cells, with deposits of a dark intracytoplasmatic material (Fig. 1B), compatible with gastric lanthanosis. There was no evidence of Helicobacter pylori infection.
Lanthanum carbonate deposits in the gastrointestinal tract can be asymptomatic (most frequent) or produce vomiting, abdominal pain, resistant iron deficiency anemia or, less frequently, gastrointestinal bleeding.1
The available scientific evidence in the medical literature about gastrointestinal bleeding due to lanthanum deposit is limited,4 being the first case report to the best of our knowledge of massive upper gastrointestinal bleeding due to deposit of this medication.
Endoscopic findings of patients on phosphate binders include diffuse or patchy deposits of a whitish material in the gastric mucosa, erosions, ulcerations or gastric polypoid nodular lesions.1 It is recommended to discontinue lanthanum treatment and follow-up with serial endoscopies to ensure the improvement or disappearance of the lesions.1,3,4
There are no acknowledgements to perform.