No studies have specifically searched for predictors of a favourable outcome that would allow a conservative therapeutic approach in adult Crohn's disease (CD).
AimsTo identify predictors of a favourable disease course over time at CD diagnosis.
MethodsWe identified and included all patients diagnosed with CD between January 1994 and December 2003, who had CD with an inflammatory pattern and no perianal disease at diagnosis, and who were followed up for at least 5 years. Clinical and therapeutic features until December 2008 and losses to follow-up were identified. We defined a favourable outcome as the absence of stricturing and penetrating complications of the disease (including perianal disease), together with the absence of need for anti-TNF therapy or resectional surgery during follow up.
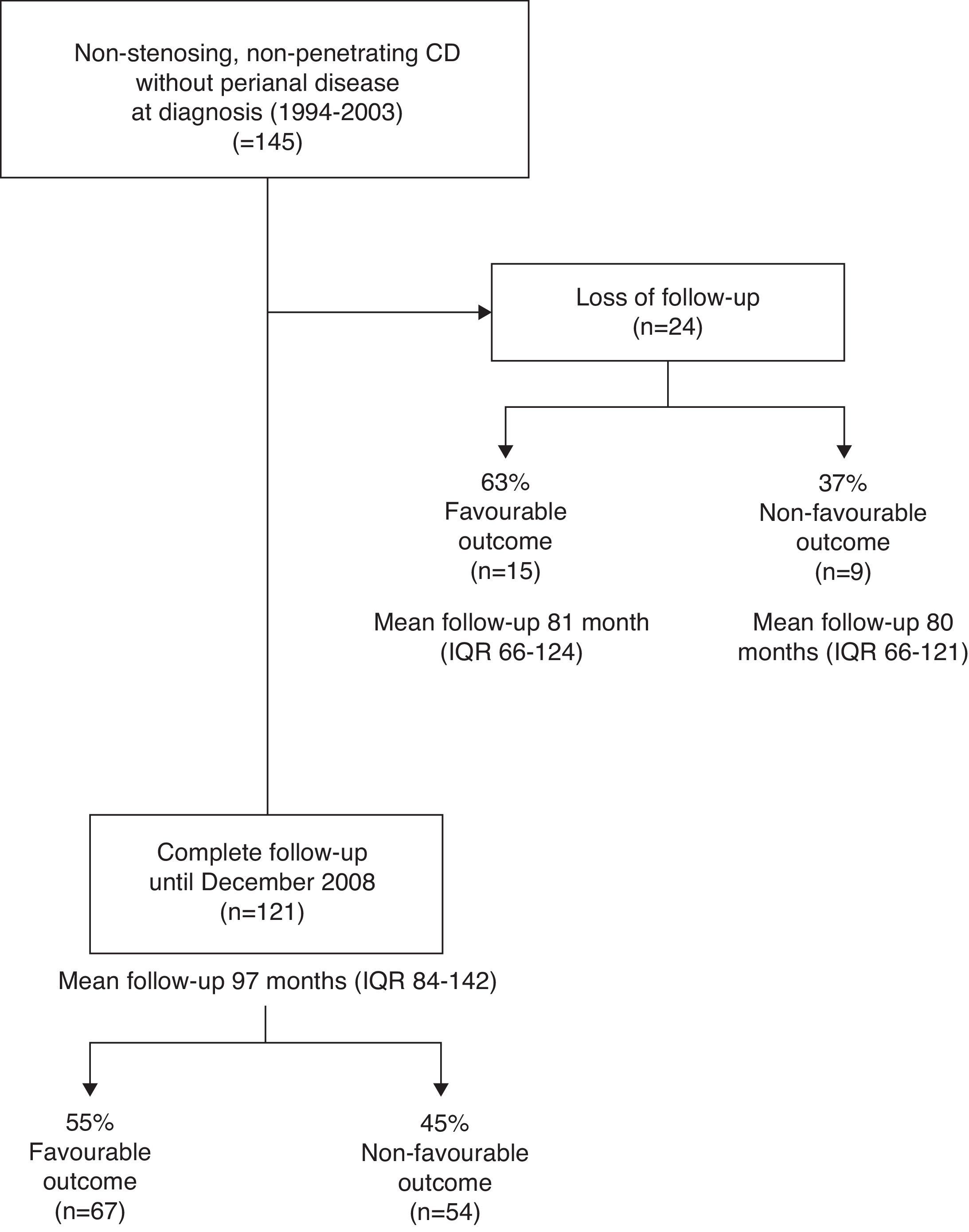
ResultsOne hundred and forty-five patients were included and followed up for a median of 96 months (IQR, 79–140). At diagnosis, location was ileal in 39%, colonic in 28%, and ileocolonic in 32%; 50% of the patients were active smokers, and 41% used immunomodulators. Eighty-two patients (57%) met the criteria for a favourable outcome at the end of follow-up. The only factor associated with a favourable outcome was isolated colonic involvement (P=0.022), with 73% of these patients meeting the criteria for a favourable outcome.
ConclusionsA favourable outcome of initially uncomplicated CD is not easily predicted at disease diagnosis by means of clinical or epidemiologic factors. Nevertheless, patients with isolated colonic disease are less likely to have an aggressive course.
Ningún estudio ha demostrado de forma específica la presencia de predictores de un curso favorable en la enfermedad de Crohn (EC), hecho que permitiría un enfoque más conservador.
ObjetivosIdentificar en el momento del diagnóstico de la EC los factores predictivos de un curso favorable en la evolución de la enfermedad.
MétodosSe identificaron e incluyeron todos los pacientes diagnosticados entre enero 1994 y diciembre de 2003, con una EC de patrón inflamatorio, sin afectación perianal en el momento del diagnóstico y con un mínimo de 5 años de seguimiento. Se recogieron las características clínicas y de tratamiento hasta diciembre de 2008 o pérdida de seguimiento. Definimos como curso favorable la ausencia de complicaciones estenosantes o penetrantes (incluida la enfermedad perianal), así como la no necesidad de terapia anti-TNF o cirugía resectiva en el seguimiento.
ResultadosCiento cuarenta y cinco pacientes fueron incluidos y seguidos por una media de 96 meses (IIQ, 79-140). Al diagnóstico, la afectación fue ileal en 39%, cólica en el 28% e ileocólica en el 32%. Así mismo, el 50% de los pacientes era fumador activo y el 41% usó inmunomoduladores desde el momento del inicio. Ochenta y dos pacientes (57%) presentaron criterios de curso favorable al final del seguimiento. Solo la afectación exclusivamente cólica se asoció a un curso favorable (p=0,022) cumpliendo en este subgrupo en un 73% los criterios de curso favorable.
ConclusionesEl curso favorable de una EC no complicada al inicio no es fácilmente predecible mediante el análisis de factores clínicos y epidemiológicos. De todas formas, parece ser que los pacientes con afectación cólica exclusiva presentan con menor frecuencia un curso agresivo.
Crohn's disease (CD) is a chronic idiopathic condition with recurrent symptoms but sustained intestinal inflammatory activity that usually leads to irreversible bowel damage and impairment of certain gastrointestinal functions. Although treatment options have been used for years in order to control symptoms, the current approach is to achieve sustained clinical, biological and even endoscopic remission,1 from early phases of the disease.2 To accomplish this goal, some therapeutic strategies have already been evaluated in the setting of RCTs.3,4
Categorisation of patients at diagnosis into high or low risk seems essential to tailor a personalised treatment according to disease prognosis. Most efforts have been focused on identifying clinical, serological and even genetic factors associated with a more aggressive course or poorer outcomes in CD to advocate a more intensive therapeutic approach right from disease diagnosis.1,5–16 However, results are highly heterogeneous mainly because of different definitions for “aggressive” disease or “poorer” outcome. Another limitation of these studies is the fact that most patients will present many of the risk factors found at disease diagnosis, making these criteria of limited usefulness in clinical practice.
To our knowledge, no studies have specifically searched for predictors of a favourable disease outcome that would allow a conservative therapeutic approach. Whereas prediction of complicated disease would provide an important tool for earlier and more intensive therapeutic intervention, a long-term, uncomplicated disease course could avoid patient overtreatment. Therefore, the aim of our study was to identify factors at CD diagnosis associated with a favourable disease course over time.
Patients and methodsPatients diagnosed with CD between January 1994 and December 2003 were identified from the Inflammatory Bowel Disease (IBD) databases of three Spanish tertiary centres. Diagnosis of CD was based on conventional Lennard–Jones criteria17 and patients were phenotypically characterised following the Montreal classification.18 Patients were only included if they had an inflammatory pattern without perianal disease at CD diagnosis, in whom biological agents were not started or resective surgery was not performed within the first 3 months, and who were followed up at the same centre for at least 5 years from diagnosis or until death. Demographic, epidemiological, and clinical features (including treatment with immunomodulators or biological agents, surgery, changes in the Montreal classification during the follow-up period) were collected from diagnosis until December 2008, loss of follow-up, or death.
For the study purposes, we arbitrarily defined favourable outcome of CD as the absence of stricturing and penetrating complications of the disease (including perianal disease), together with no need for biological therapy with anti-tumour necrosis factor agents or resectional surgery, during follow-up. We decided that the use of immunomodulators (azathioprine, 6-mercaptopurine or methotrexate) did not preclude the favourable outcome definition because thiopurines are widely used even at disease diagnosis in many clinical settings (paediatric onset of CD, extensive intestinal involvement, corticosteroid use)19 and they are – together with biological agents – the only effective drugs for maintenance of remission. Consequently, their use is widespread and should not be seen as an intensive treatment strategy. Consequently, for analysis purposes, patients were only considered immunomodulator users if they started these medications before losing favourable outcome status or if they maintained their favourable outcome status until the end of follow-up. Conversely, the use of biological agents still depends on the development of certain unfavourable outcomes such as chronically active disease, steroid-dependence o refractoriness, failure of conventional immunomodulators or disease-related penetrating complications. From this perspective, we decided to consider the use of biological agents as surrogate marker of disease severity.
In relation to smoking, non-smokers were defined as those patients who had never smoked or had smoked less than 7 cigarettes/week,20former smokers as those who had given up smoking at least 12 months before CD diagnosis and, in the remaining situations, patients were considered to be active smokers.
This was an observational study according to the Declaration of Helsinki and approved by the Institutional Review Board of the steering centre (Hospital Universitari Germans Trias i Pujol).
Statistical analysisDescriptive statistics are expressed as percentages for categorical variables and median with interquartile range (IQR) for continuous variables. Student's t-test was used to compare continuous variables between study groups (patients with and without favourable outcome). The log rank test was performed to compare Kaplan–Meier curves for categorical variables. Those variables reaching a P-value of less than 0.1 were included in the multivariate analyses (Cox proportional-hazards regression). Insofar as background centre might influence medical practice it was also included in the multivariate analysis, together with the use of immunomodulators, as potential confounding variables. All statistical tests were two-tailed and performed using the SPSS statistical tests with the PASW Statistics/SPSS 18.0 package for Windows Inc., Chicago, IL, USA.
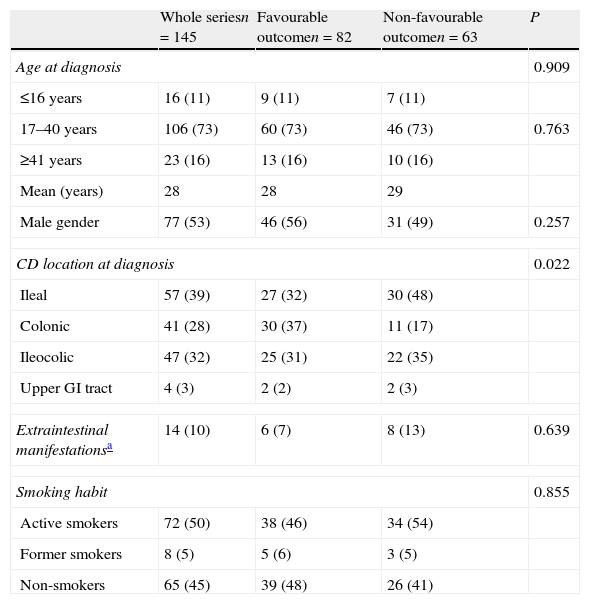
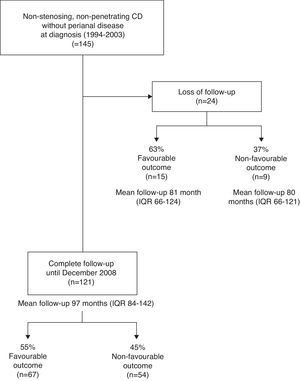
ResultsA total of 145 patients were included and followed up for a median of 96 months (IQR, 79–140), 83% of them until the end of the study period in December 2008 (Fig. 1). No patients died during the study period. A total of 82 patients (57%) met favourable outcome criteria at the end of follow-up. Table 1 shows the clinical characteristics at disease diagnosis of the whole study population as well as the comparison between patients with or without favourable outcome.
Clinical and demographic characteristics at CD diagnosis.
| Whole seriesn=145 | Favourable outcomen=82 | Non-favourable outcomen=63 | P | |
| Age at diagnosis | 0.909 | |||
| ≤16 years | 16 (11) | 9 (11) | 7 (11) | |
| 17–40 years | 106 (73) | 60 (73) | 46 (73) | 0.763 |
| ≥41 years | 23 (16) | 13 (16) | 10 (16) | |
| Mean (years) | 28 | 28 | 29 | |
| Male gender | 77 (53) | 46 (56) | 31 (49) | 0.257 |
| CD location at diagnosis | 0.022 | |||
| Ileal | 57 (39) | 27 (32) | 30 (48) | |
| Colonic | 41 (28) | 30 (37) | 11 (17) | |
| Ileocolic | 47 (32) | 25 (31) | 22 (35) | |
| Upper GI tract | 4 (3) | 2 (2) | 2 (3) | |
| Extraintestinal manifestationsa | 14 (10) | 6 (7) | 8 (13) | 0.639 |
| Smoking habit | 0.855 | |||
| Active smokers | 72 (50) | 38 (46) | 34 (54) | |
| Former smokers | 8 (5) | 5 (6) | 3 (5) | |
| Non-smokers | 65 (45) | 39 (48) | 26 (41) | |
Expressed as absolute numbers (frequencies). CD: Crohn's disease; GI: gastrointestinal tract.
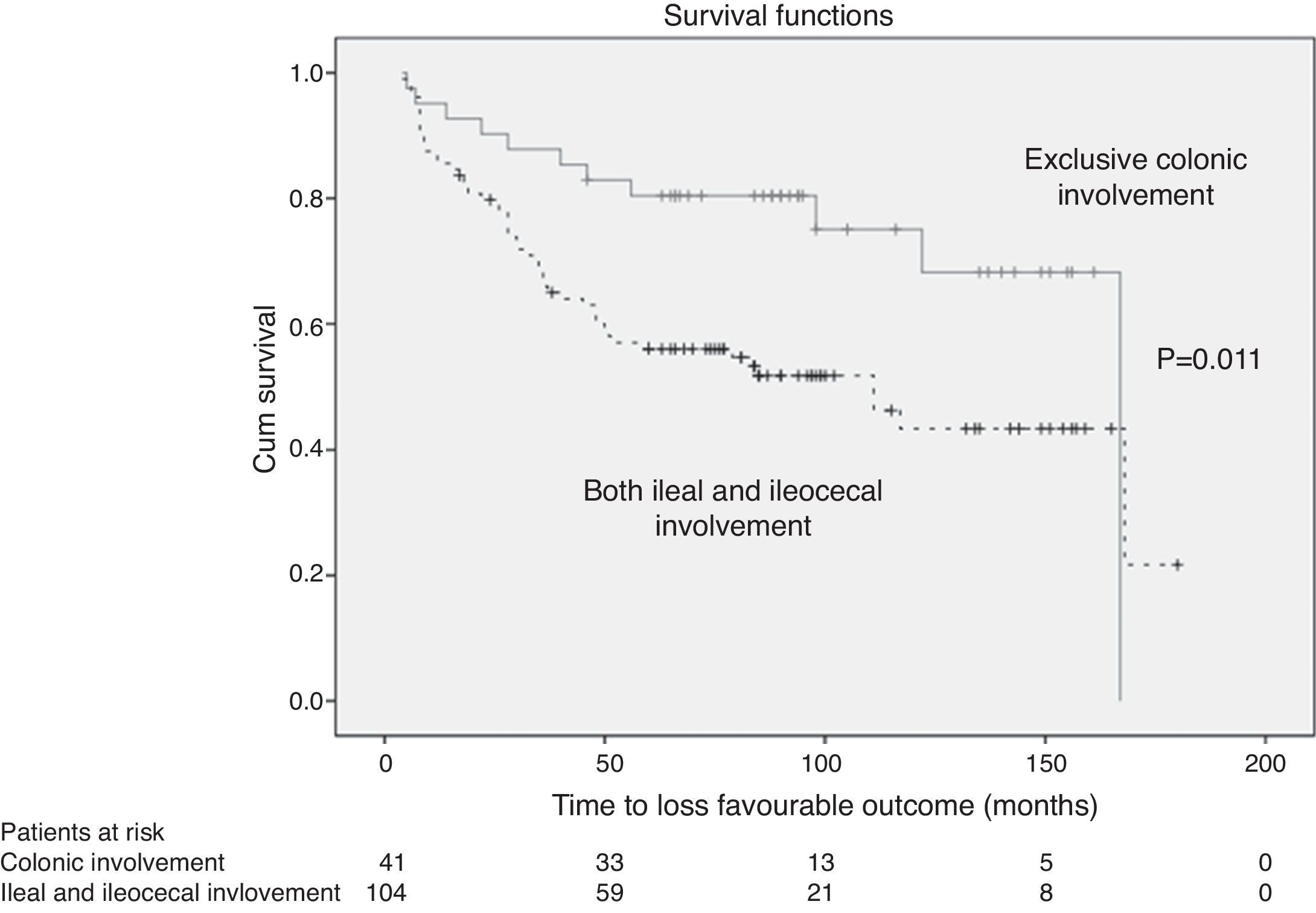
Disease location at diagnosis was the only significant difference between the two groups of patients in the log rank test, with isolated colonic involvement being more frequent compared to other locations (37% vs. 17%, P=0.022) among patients with favourable outcome. Although the use of immunomodulators was different regarding clinical outcome (49% [44/90] in favourable outcome and 29% [16/55] in non-favourable outcome), this difference did not reach statistical significance (P=0.078).
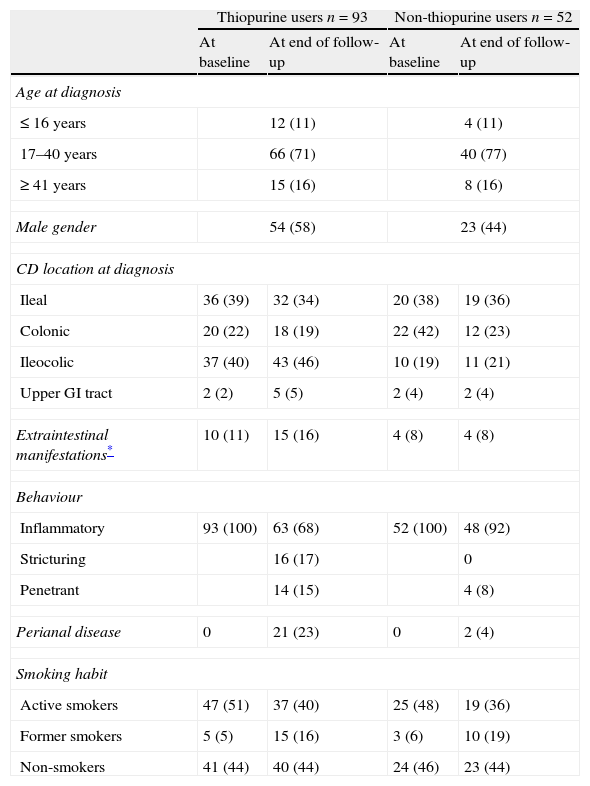
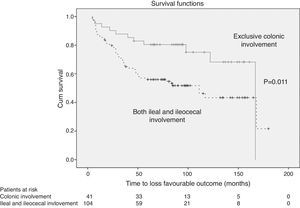
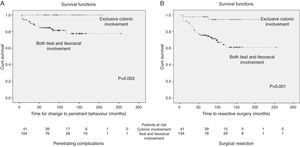
Despite this and, as stated before, immunodulator use was included together with background centre as potential confounding factors into the Cox proportional-hazards regression model for favourable outcome. The regression analysis showed that isolated colonic involvement was the only independent predictor of a favourable outcome (RR 2.192 [CI 95%]: 1.021–4.704, P=0.044) Fig. 2). Clinical characteristics of the group of patients that required immunomodulators from diagnosis or later on in the disease evolution are presented in Table 2.
Clinical and demographic baseline characteristics between users of thiopurines or not users.
| Thiopurine users n=93 | Non-thiopurine users n=52 | |||
| At baseline | At end of follow-up | At baseline | At end of follow-up | |
| Age at diagnosis | ||||
| ≤ 16 years | 12 (11) | 4 (11) | ||
| 17–40 years | 66 (71) | 40 (77) | ||
| ≥ 41 years | 15 (16) | 8 (16) | ||
| Male gender | 54 (58) | 23 (44) | ||
| CD location at diagnosis | ||||
| Ileal | 36 (39) | 32 (34) | 20 (38) | 19 (36) |
| Colonic | 20 (22) | 18 (19) | 22 (42) | 12 (23) |
| Ileocolic | 37 (40) | 43 (46) | 10 (19) | 11 (21) |
| Upper GI tract | 2 (2) | 5 (5) | 2 (4) | 2 (4) |
| Extraintestinal manifestations* | 10 (11) | 15 (16) | 4 (8) | 4 (8) |
| Behaviour | ||||
| Inflammatory | 93 (100) | 63 (68) | 52 (100) | 48 (92) |
| Stricturing | 16 (17) | 0 | ||
| Penetrant | 14 (15) | 4 (8) | ||
| Perianal disease | 0 | 21 (23) | 0 | 2 (4) |
| Smoking habit | ||||
| Active smokers | 47 (51) | 37 (40) | 25 (48) | 19 (36) |
| Former smokers | 5 (5) | 15 (16) | 3 (6) | 10 (19) |
| Non-smokers | 41 (44) | 40 (44) | 24 (46) | 23 (44) |
Expressed as absolute numbers (frequencies). CD: Crohn's disease; GI: gastrointestinal tract.
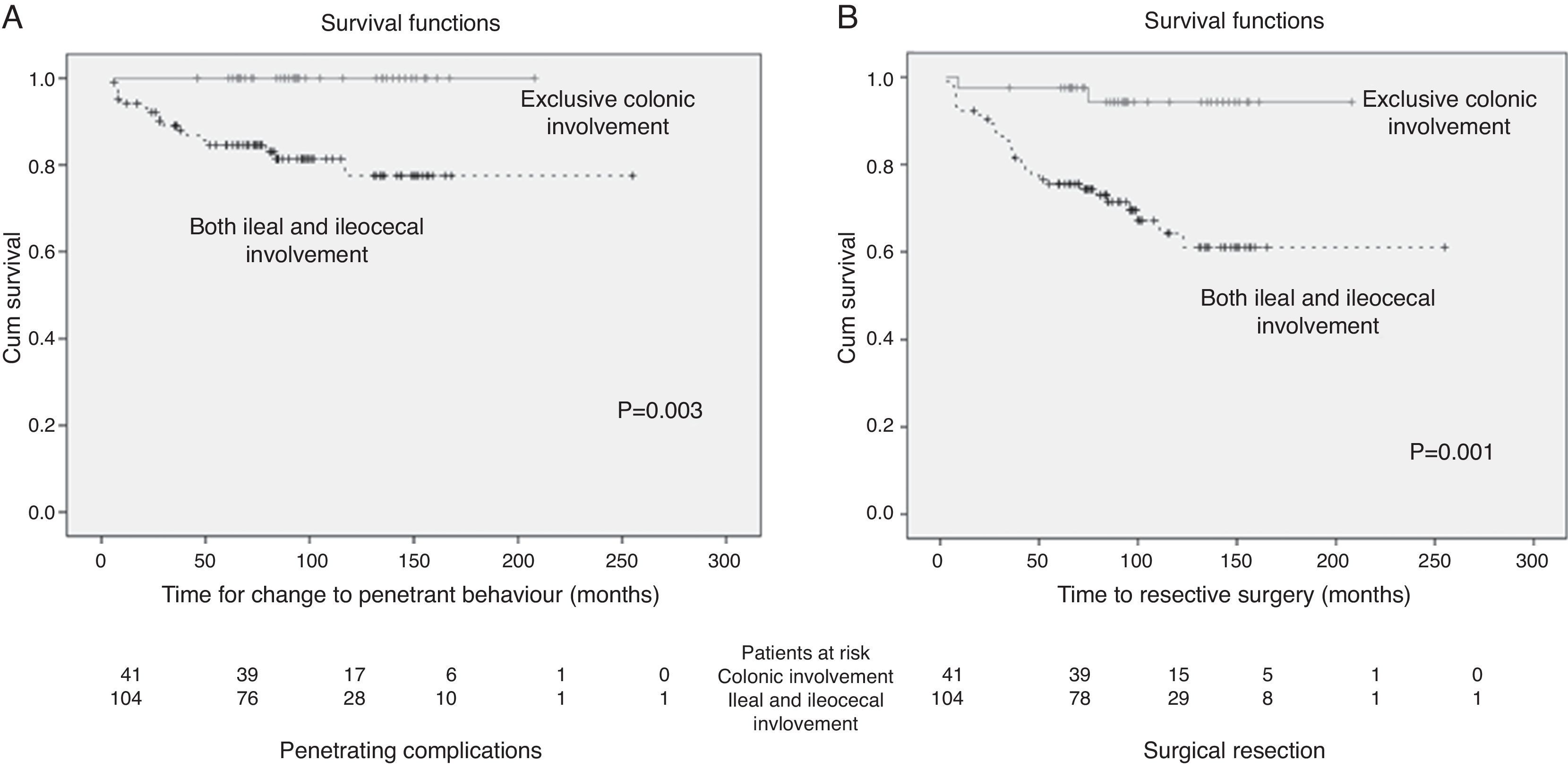
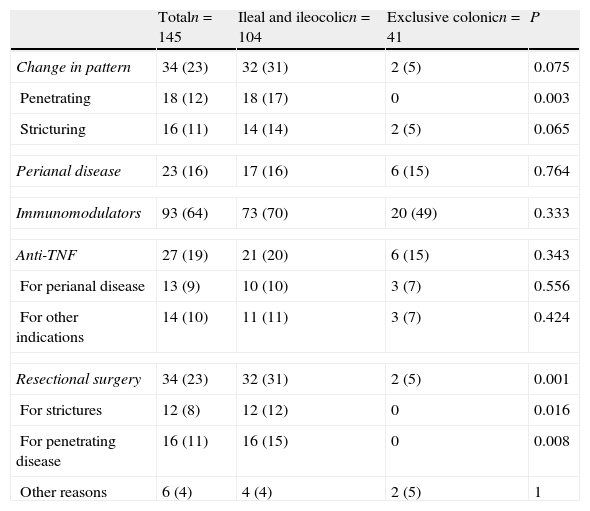
Table 3 shows the development of disease-related complications as well as therapeutic requirements of the whole series. A more favourable outcome among patients with isolated colonic involvement was due to a lower risk of developing intra-abdominal penetrating complications (P=0.003), and for requiring resectional surgery (P=0.001) when compared to exclusive ileal and ileocolonic location (Fig. 3).
Clinical and therapeutic outcomes according to initial disease involvement.
| Totaln=145 | Ileal and ileocolicn=104 | Exclusive colonicn=41 | P | |
| Change in pattern | 34 (23) | 32 (31) | 2 (5) | 0.075 |
| Penetrating | 18 (12) | 18 (17) | 0 | 0.003 |
| Stricturing | 16 (11) | 14 (14) | 2 (5) | 0.065 |
| Perianal disease | 23 (16) | 17 (16) | 6 (15) | 0.764 |
| Immunomodulators | 93 (64) | 73 (70) | 20 (49) | 0.333 |
| Anti-TNF | 27 (19) | 21 (20) | 6 (15) | 0.343 |
| For perianal disease | 13 (9) | 10 (10) | 3 (7) | 0.556 |
| For other indications | 14 (10) | 11 (11) | 3 (7) | 0.424 |
| Resectional surgery | 34 (23) | 32 (31) | 2 (5) | 0.001 |
| For strictures | 12 (8) | 12 (12) | 0 | 0.016 |
| For penetrating disease | 16 (11) | 16 (15) | 0 | 0.008 |
| Other reasons | 6 (4) | 4 (4) | 2 (5) | 1 |
Expressed as absolute numbers (frequencies).
In order to search for more accurate outcome prediction among patients with isolated colonic disease we evaluated endoscopic lesions at disease diagnosis. Complete and detailed colonoscopy reports at diagnosis were available in 38 out of 41 patients with colonic CD. A further analysis was performed regarding the presence of deep ulcers at colonoscopy in this subset of patients. No differences were found with respect to the presence of deep ulcers in at least one colonic segment (57% favourable outcome group vs. 70% non favourable outcome group, P=0.475) or within more than one colonic segment (25% favourable outcome group vs. 20% non favourable outcome group, P=1). No correlation was noticed between rectal involvement and the risk of perianal disease on follow-up (12% rectal involvement without perianal disease vs. 20% rectal involvement with perianal disease, P=1).
DiscussionCD is a chronic condition that often leads to irreversible intestinal damage that may cause nutritional deficiencies, a decrease in patients’ quality of life and even loss of intestinal functions. Despite the widespread use of immunomodulators and the availability of biological agents, up to 50% of CD patients still need to be operated on because of the development of stricturing or penetrating disease complications.14 For this reason, some authors maintain that an early introduction of such therapies might change the natural history of the disease.2 However, we all agree that the systematic implementation of more intensive treatment strategies would overtreat a proportion of patients not at risk of CD-related complications. The use of immunomodulators and/or biological agents may be associated with the occurrence of severe side effects, specifically serious infections and malignancies.21,22 Under this perspective, the accurate prediction of the disease course is urgently required. To date, most efforts have been focused on identifying risk factors for aggressive disease. Unfortunately, criteria to define aggressive or invalidating disease course have been widely heterogeneous and include phenotypic patterns,10 disabling chronic symptoms,11 use of corticosteroids,10,11 immunomodulators,11,14,15 biological agents,11,15 surgery,1,8,11,13,14 hospitalisations,11 or the development of stricturing or penetrating complications6,9,16 including perianal disease.7,11,13,15 Nevertheless, those risk factors found in different studies are present in most patients at diagnosis, and some authors state that they may not even be predictors but already manifestations of the condition it is attempting to predict.23 Our study differs from the above-mentioned studies in that we intentionally did not consider the use of immunomodulators as a criterion to exclude a favourable outcome in an attempt to reflect real-life clinical practice. Thiopurines are widely prescribed and are the drug of choice for evidence-based maintenance therapy in CD. Our results showed a clear trend to a better outcome in patients on thiopurines, and that is the reason why we decided to include thiopurine therapy as a variable in the multivariate analysis; however, no statistically significant association was obtained.
Factors for “favourable course” of the disease have not been specifically addressed. It can be assumed that not having an aggressive disease equals having a favourable course, but this last assumption is not appropriate given the heterogeneity of definitions.
Despite this divergence of predictors in CD evolution, it seems clear that a complicated disease behaviour (with its structuring and penetrating patterns) as well as the use of biological agents and/or intestinal resection may gather the most used clinical factors for outcome prediction. Therefore, we decided to use them in order to set the “favourable course” definition employed in this study. Our results show that exclusive colonic involvement is the only clinical baseline characteristic associated to a higher likelihood of favourable outcome. Similar findings have already been reported albeit in a different way. Ileal or ileocolic involvement has been found to be a risk factor for poorer outcome in one study,7 as patients with colonic disease tend to need less surgery1,12,24,25 or corticosteroid courses,24 have slower progression to complicated disease15 and are protected from the development of strictures and obstruction.10 Only one study reported colonic involvement to be a predictor of aggressive disease, but the authors did not consider isolated colonic involvement and the study included a small number of patients in the ileal group.5
Despite being the only predictor of a favourable disease course, 27% of patients with exclusive colonic involvement (11/41 of isolated colonic) still did not meet our criteria for favourable outcome. We performed additional analyses to better identify these patients exploring their baseline endoscopic findings; we failed to find additional prognostic factors. Allez et al., in a landmark study, reported the predictive value of severe endoscopic lesions among patients with ileocolonic CD.8 However, it should be considered that the French study only included patients with colonic involvement and with available endoscopic data. Thus, this cohort could be biased by the inclusion of patients with a more active disease. Conversely our study dealt with the hospital inception cohort.
Our study has important limitations. First, its retrospective nature hinders the adequate assessment of many potential relevant data such as the duration of symptoms up to disease diagnosis, degree of weight loss or accurate information related to endoscopic or cross-sectional imaging findings. Second, this was a cohort coming from three referral centres whereas population-based cohorts are recommended for describing true phenotype disease outcome correlations.12,26 Third, it has to be considered that our cohort includes patients who were diagnosed before the full availability of antiTNF therapy; as far as antiTNF use was included in the definition of favourable outcome, this should interfere with the results. However, antiTNF drugs are still introduced in patients refractory to conventional therapy including immunosuppressants, reducing the risk of bias. Fourth, our study did not include serologic or genetic factors that have been proposed to be of potential usefulness for an accurate CD clinical course prediction.23 Serological markers seem to correlate to CD phenotypic subsets27–30 or different time progression courses.16,29,31
On the other hand, however, our series has a follow-up time that is long enough to study the phenotypic natural history of CD, as proposed by Silverberg.18
In short, in the setting of the current use of immunomodulators, CD patients with uncomplicated, isolated colonic involvement are less likely to present disease-related complications or require biological agents. Although population-based cohort studies adding genetic and serologic data are warranted, a conservative approach in this subset of patients seems to be appropriate.
Conflict of interestThe authors declare no conflict of interest.
This study was partly supported by CIBERehd (Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas) of Fondo de Investigación Sanitaria of the Instituto de Salud Carlos III, from the Spanish Ministry of Health.