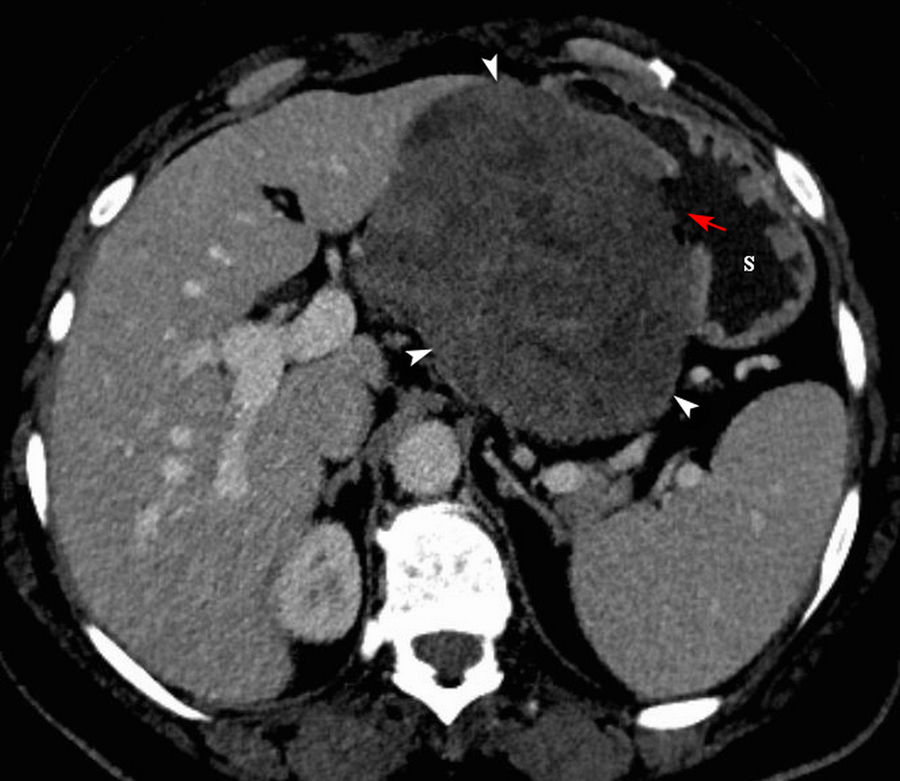
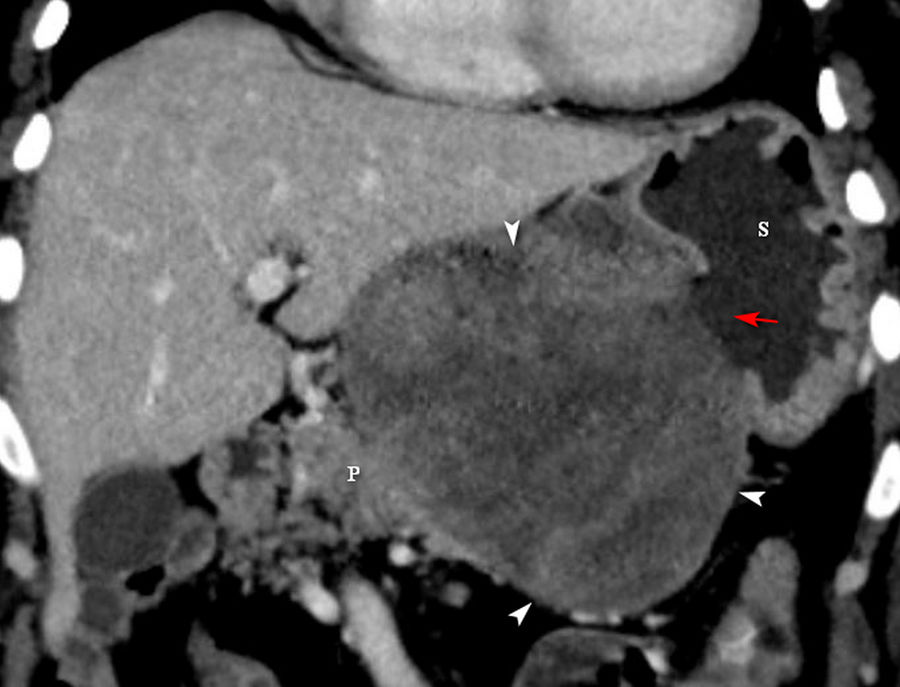
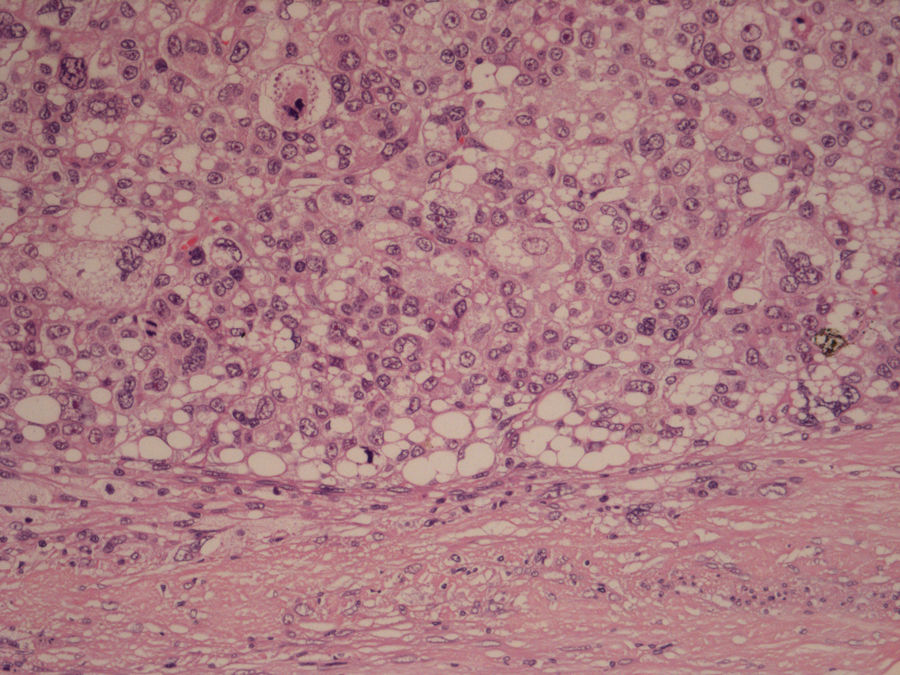
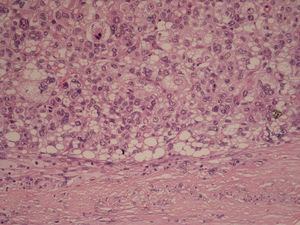
A 50-year-old female was referred to our clinic for further investigations and treatment due to an abdominal mass detected on ultrasound during a routine check-up in another department. The medical history was irrelevant. At our institution, she was tachycardic, normotensive, but anemic with a hemoglobin level of 5.5mg/dL. A CT scan of the abdomen was performed, which revealed a large ulcerated, well-defined, heterogeneously enhancing mass lesion of size 13×8×7cm on the lesser curvature of the stomach, occupying the lesser sac, associated with loss of fat planes with the pancreas body (Fig. 1, Fig. 2). There was no infiltration of the mass into the surrounding structures, nor any evidence of metastases or lymphadenopathy. According to imaging features, it has been suggested that the most likely etiology is a gastrointestinal stromal tumor (GIST). An attempt was made to perform a gastroscopy, but due to the patient's poor cooperation this was unfortunately not possible, thus no pre-operatively biopsy was performed. The mass was completely resected with a total gastrectomy and distal pancreatectomy. Histopathology of the tumor showed a tumor with sheets of large pleomorphic cells with vesicular hyperchromatic nuclei showing plenty of mitosis, occasional lipoblasts (Fig. 3), associated with focal areas of spindle-shaped cells. Immunostaining showed that the cells were positive for vimentin and some were also positive for S-100. The final pathological diagnosis was a pleomorphic liposarcoma grade 3 FNCLCC arose in the lesser omentum with gastric and pancreatic infiltration. The post-operative period was uneventful till her discharge from the hospital. Following the surgery, a 24-day period of chemotherapy treatment was initiated, with ifosfamide (2g, days 1–3), and epirubicin (60mg day 1; 50mg day 2). She only underwent 2 cycles of chemotherapy treatment and then refused the subsequent treatment. In follow up, of 3 months after the surgery, the patient remained asymptomatic and disease free.
According to World Health Organization (WHO),1 pleomorphic liposarcoma is the rarest type of liposarcomas (5–10%), with a very high chance of local recurrence and metastasis compared to other histological variants. The most common sites are proximal extremities, followed by the retroperitoneum. Primary lesser sac pathological processes are very rare, and it is characterized as the growth of a progressively mass, and it is easily ignored until it has large sizes or there are some compressive manifestations.2 It is very difficult to distinguish pleomorphic liposarcoma from other liposarcoma or sarcoma based on imaging features, and the definite diagnosis depends on the pathological examination. The main treatment is surgery, especially radical resection, and for patients with distant metastasis and local invasion is recommended palliative intervention with relieve the compression symptoms.2,3