INTRODUCTION
Primary gastrointestinal melanoma is rare. Most gastrointestinal melanomas are metastatic from primary cutaneous lesions. Only eight cases of primary malignant melanoma of the common bile duct (CBD) have been described in the literature. The diagnosis is based on failure to find another primary site, histological examination with electron microscopy, and immunohistochemical tests.
CASE REPORT
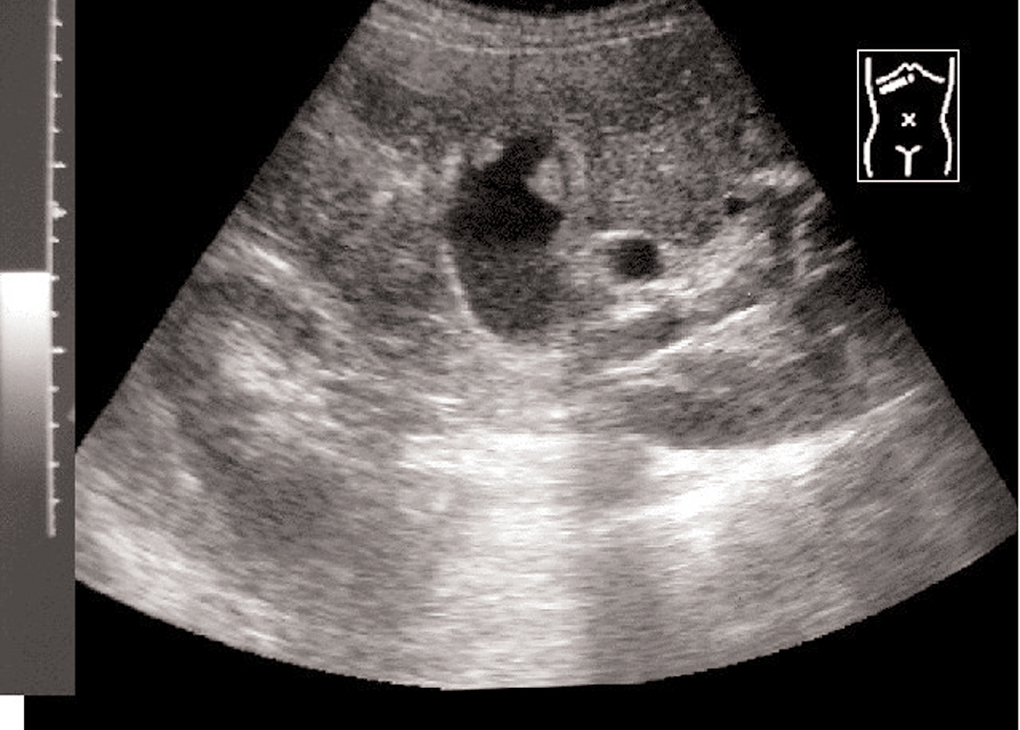
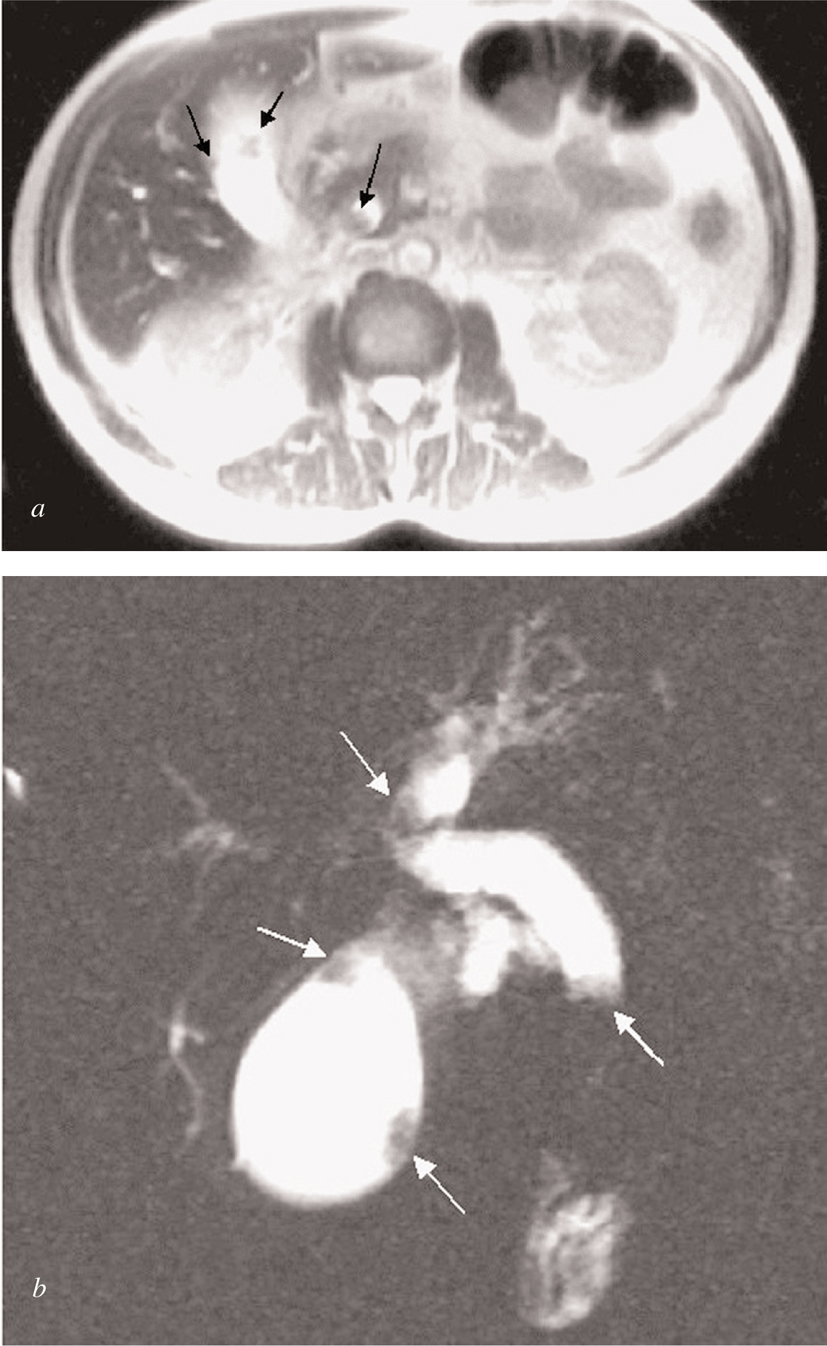
A 47-year-old man presented in July 2000 with progressive jaundice for 3-4 weeks, weakness, and anorexia leading to weight loss, as well as occasional right upper quadrant abdominal pain. He had been under treatment for a depressive syndrome for the previous 5 months and his medication had been changed due to a rise in serum aminotransferases. Liver function tests at admission showed pronounced cholestasis (total bilirubin 13.9 mg/dl, conjugated bilirubin 9.1 mg/dl, alkaline phosphatase 703 U/L, gamma glutamyl transferase 72 U/L) and mild hepatic cell necrosis (alanine aminotransferase 99 U/L (normal < 41 U/L) aspartate aminotransferase 44 U/L (normal < 37 U/L) without liver failure. Ultrasound showed intra- and extrahepatic bile duct dilation with several nodules on the gallbladder wall (fig. 1). Magnetic resonance cholangiopancreatography also revealed an obstructive tumor in the distal extrahepatic duct (figs. 2a-b). All lesions showed the same radiological pattern.
Fig. 1. Ultrasound revealed intra- and extrahepatic bile duct dilatation with multiple hyperechogenic polypoid mural masses in bile tree and gallbladder.
Figs. 2a-b. Magnetic resonance cholangiopancreatography showed an obstructive intraluminal mass in the distal common bile duct (CBD) and multiple polypoid mural gallbladder masses.
Because of the spread of the disease, surgery was rejected. Percutaneous drainage and biopsy of the gallbladder and biliary duct lesions were performed, and an endoprosthesis was placed.
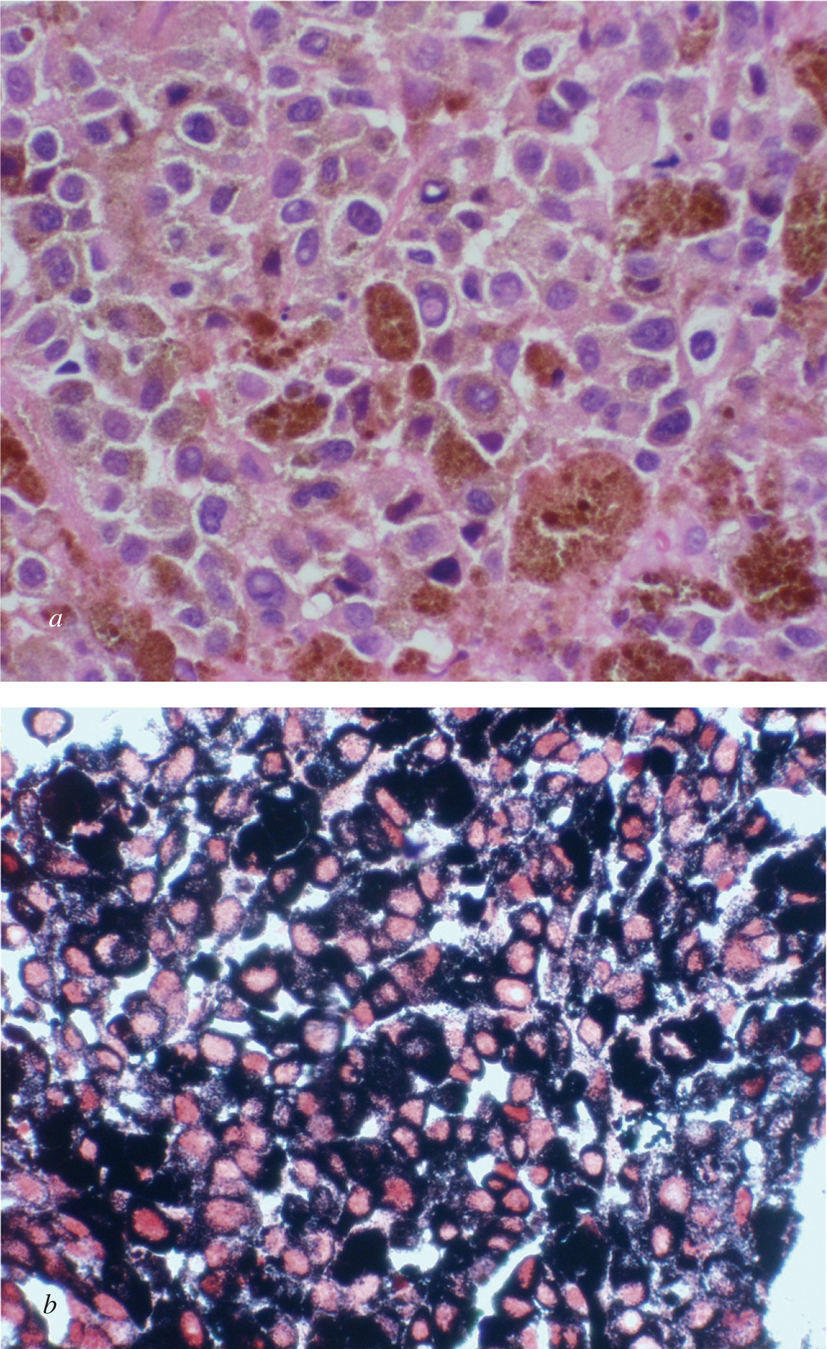
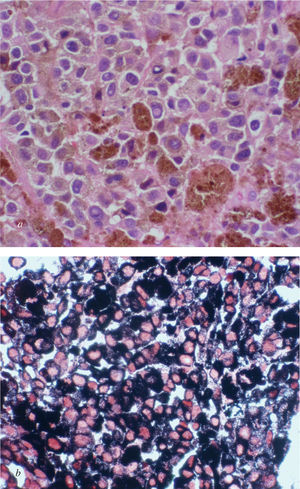
Pathological findings were positive for malignant melanoma cells (figs. 3a-b). Histologically, neoplastic cells were large, hyperchromatic and had irregular nuclei, as well as a moderate eosin cytoplasm, with a significant presence of melanic pigment. They showed a poorly cohesive pattern and were sometimes found in isolation. Nucleoli were prominent with occasional nuclei pseudoinclusions. Neoplastic cells were reactive to antibodies to S-100 protein, HMB-45 and vimentin and were negative to keratin antibodies (Q116).
Figs. 3a. Wide cytoplasm cells with abundant melanic pigment, irregular nuclei with cytoplasmic inclusions, and mitotic figures (hematoxylin-eosin stain x400). b) Abundant melanic pigment is shown in black (Fontana stain x400).
A thorough physical examination including particular attention to the skin, eyes, and digestive tract failed to reveal another primary source. We concluded that the primary site of the malignant melanoma was the biliary tract itself.
Due to disease progression, chemotherapy was indicated. Beginning in March 2001, three cycles of 850 mg/m dacarbazine every 21 days and 3nterferon 2b 3 million/3 times a week were administered, but the disease spread to the stomach, spleen and lymph nodes. In October 2001, a new palliative line of chemotherapy was initiated with three cycles of carboplatine AUC 5, but the disease spread to subcutaneous, peritoneal, kidney and gastrohepatic areas. The patient had good quality of life and pain was controlled with metamizol, despite disease progression for 5 more months. He was included in a clinical trial of a new chemotherapy protocol but was withdrawn from the program because of poor clinical course. He died in June 2002.
DISCUSSION
Although malignant melanoma usually originates on the skin, it can also develop from squamous mucous membranes, uvea, retina, and leptomeninges. Primary gastrointestinal melanoma is rare and most gastrointestinal melanomas are metastatic from primary cutaneous lesions, which are the most common tumors to metastasize to the gallbladder. New diagnostic imaging techniques allow a presumptive diagnosis to be made, as in our case1.
It is important to establish a diagnosis of primary tumor, and the steps to do so are well documented. Firstly, the clinical absence of a primary cutaneous or visceral melanoma must be verified. To distinguish primary from metastatic melanoma, a junctional component, formed by clustered melanocytes at the mucosa-submucosa junction adjacent to the tumoral mass, must be identified and defined by immunoreactivity (S100). This is the most conclusive histologic evidence for primary melanomas in unusual locations2-4.
Primary malignant melanoma of the CBD was first described by Zaide5 in 1963. Since then, seven other cases have been reported. The first case reported was a 47-year-old man with a 3-month history of obstructive jaundice. He was treated by cholecystectomy and resection of the CBD. There was no evidence of metastatic lesions and he was alive 6 months after surgery.
The second case, published by Carstens et al6 in 1986 and Wright et al7 in 1988, describes biliary tract obstruction in a 30-year-old man due to a primary malignant melanoma. A Whipple resection was performed and the primary origin of the tumor was confirmed by immunohistochemistry and electron microscopy. The patient had lymph node metastases and developed multiple liver metastases 1 month after surgery. He died 6 months later.
In 1991, two more cases were published. Deugnier et al2 described an obstruction of the extrahepatic bile duct due to malignant melanoma in a 34-year-old woman. Treatment consisted of a left hepatectomy with partial right hepatic bile duct and CBD resection. Clinical course was poor, with progressive involvement of lymph nodes and subcutaneous nodules. The patient died 18 months after diagnosis.
In the same year, Zhang et al8 reported a 58-year-old man presenting with obstructive jaundice caused by a CBD mass and another mass involving the gallbladder. After histologic diagnosis, a Whipple operation was performed. Two years after resection, the patient was alive and apparently disease-free.
Gates et al9 reported two cases in 1996. The first concerned a 45-year-old man with a 1-month history of obstructive jaundice. A Whipple technique was carried out, and 6 years later he was well and without signs of disease. The second case was a 43-year-old man who had experienced symptoms similar to those of the previous cases for 2 months. He underwent a right hepatectomy, cholecystectomy, and excision of the extrahepatic biliary tree for a lesion at the junction of the CBD. He remained alive and well 11 months after resection10.
The last case before ours was published in 2000 by Wagner et al4. A 48-year-old man presented with symptoms of acute cholecystitis. An open cholecystectomy was performed on an acalculous and necrotized gallbladder. He had an uneventful postoperative course and 6 weeks later he presented obstructive jaundice caused by a primary malignant melanoma. Initially, a T-tube was inserted into the proximal bile duct and 4 weeks later a Whipple operation was performed. Three months later he presented brain metastases and died 9 months after the initial diagnosis.
Metastatic melanoma rarely involves the CBD. Necropsies show only 6% of cases with CBD metastases in patients with primary melanoma at another site9. Primary melanoma of the CBD is usually an intraluminal polypoid tumor with a single pedicle. In contrast, metastatic melanoma has usually been described as multiple, small, flat and pigmented nodules3,8,11. The criteria used to make the diagnosis of primary melanoma include size and shape of the tumor, the presence of junctional activity (S-100 protein) and, most importantly, the lack of other primary sites3,8. Nevertheless, Higgins et al12 have questioned the existence of primary melanoma in the gallbladder and bile duct because they found a metastatic melanoma at these sites with the features of a primary tumor. Further studies and follow-up are required to understand this entity but, given its rarity, this will not be easily achieved.