Levodopa is the gold standard treatment for Parkinson's disease (PD). However, due to its short plasma half-life, requiring repeated doses, long-term levodopa use (usually within 5–10 years after initiating treatment) is associated with motor fluctuations and dyskinesias. Impaired gastric emptying is also common in PD patients and leads to unpredictable responses to oral medication. These facts induce disability and lower quality of life.1 Therapeutic alternatives for patients with advanced PD include deep brain stimulation, continuous subcutaneous apomorphine infusion and intrajejunal levodopa-carbidopa infusion. Continuous intraduodenal/intrajejeunal infusion of a levodopa-carbidopa (L-C) gel (Duodopa®, Abbvie) – which contains levodopa 20mg/ml plus carbidopa 5mg/ml – improves motor fluctuations2,3 (off time and severity and dyskinesia), non-motor symptoms,4 autonomy for basic activities5 and quality of life.6 This therapy is performed by placing a specific percutaneous endoscopic gastrostomy (PEG) kit (Frecka® PEG gastric set) that contains inside a 9Fr duodenal pigtail (Freka® CH9 intestinal tube) probe. This technique requires cooperation between the neurologist that sets the indication for this treatment and does a close surveillance of the patient, and the Gastroenterologist/Endoscopist that places the PEG probe and performs the surveillance and replacements of the device.
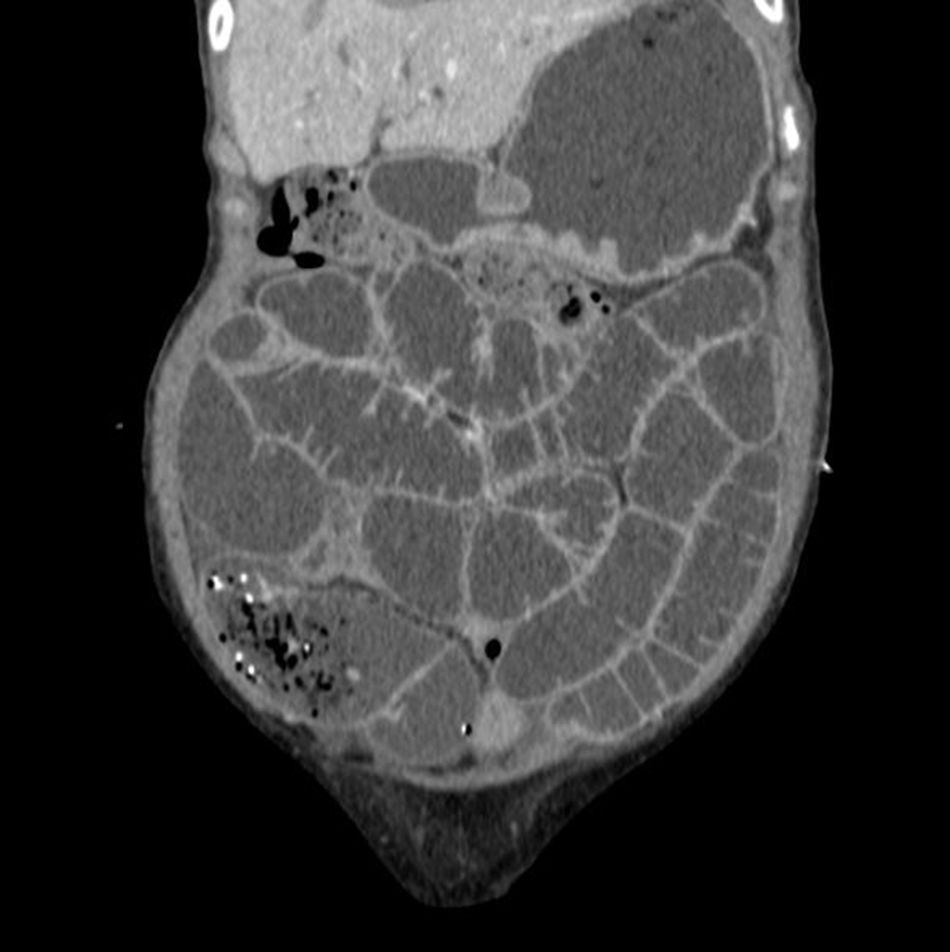
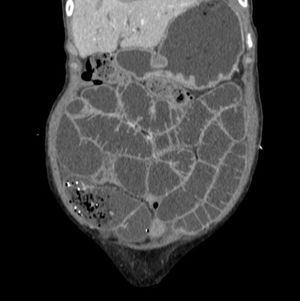
A 76 year-old woman with advanced PD complicated with motor fluctuations required Duodopa® administration to control her motor symptoms. Therefore, a PEG-Duodopa was placed, with Propofol sedation, after informing the patient and her family about the benefits and the possible risks related to the procedure. Thirty minutes before the PEG-duodopa allocation, the patient received antibiotic prophylaxis with Cefazolin 2g. It was performed without any immediate complications and lack of complications was verified by immediate endoscopic control, as usual. The patient was discharged from hospital 2 days after the procedure, with marked improvement of the motor symptoms, since PEG-duodopa was used for the first time 24h after its allocation. After eleven days, the patient was admitted to the emergency room because of abdominal distension with pain and vomiting, which was highly suggestive of an intestinal obstruction. Plain abdominal X-ray showed the duodenal probe tip of the Freka® CH9 Intestinal Tube projected in right iliac fossa and absence of pneumoperitoneum. Severe abdominal pain persisted despite administration of analgesics, so an urgent abdominal CT was indicated to discard any other complication. It confirmed the presence of the pigtail probe coiled in the ileum due to distal migration, conditioning severe retrograde small bowel dilation (Fig. 1). Since the patient had no response to conservative treatment, emergency surgery was indicated, performing an ileostomy, extraction of the probe and primary suture without associated complications. Ten days after surgery, after discussing the case between surgeons, endoscopists and neurologists, and with the agreement of the patient, placement of a new duodenal pigtail type probe was carried out without further complications.
Continuous L-C gel infusion is a highly effective and well accepted alternative for the treatment of advanced PD patients.5,6 Duodenal infusion avoids problems related to delayed stomach transit. It has a similar safety profile to oral medication providing better control of motor and non motor symptoms in those cases. However, specific complications related to probe placement cannot be overlooked. They include complications related to: (a) the stoma, like infection, granuloma development, etc., (b) the gastrostomy probe, like buried bumper syndrome; and (c) the pigtail probe: distal migration, bending, or probe break. Events that involve the probe are very frequent (a study7 described that more than 60% of the patients had at least 1 event with duodenal probe after one year with continuous L-C infusion). Distal migration is generally asymptomatic, with spontaneous anal expulsion. Perforation or intestinal obstruction8 secondary to probe migration as in the case exposed is exceptional.