The intrauterine device (IUD) is a highly effective, inexpensive, generally well tolerated and widely used contraceptive method. A serious but rare complication is perforation of the uterus and migration to the abdomen.1 The risk of uterine perforation (UP) is reported to be between 1 in 350–2500 women, although the actual incidence could be higher, since many of these cases are asymptomatic. While most IUD uterine perforations do not involve other organs, a small percentage cause erosion and perforation of other abdominal organs, among them the small intestine, for which fewer than 10 cases have been described.2 The following case of small bowel perforation by an IUD describes this rare complication.
A 29-year-old patient came to the emergency department for moderate intensity hypogastric pain associated with amenorrhoea and negative pregnancy test. She had a history of irregular menstruation and insertion of a T-shaped IUD 14 months previously. She did not report any complications at the time of placement and denied expulsion. Abdominal examination revealed moderate intensity pain on deep palpation in the hypogastric region with no guarding, normal size intrapelvic uterus, and no palpable tumours. During the gynaecological examination, the threads of the IUD were not observed in the external cervical orifice. Rectal examination was normal.
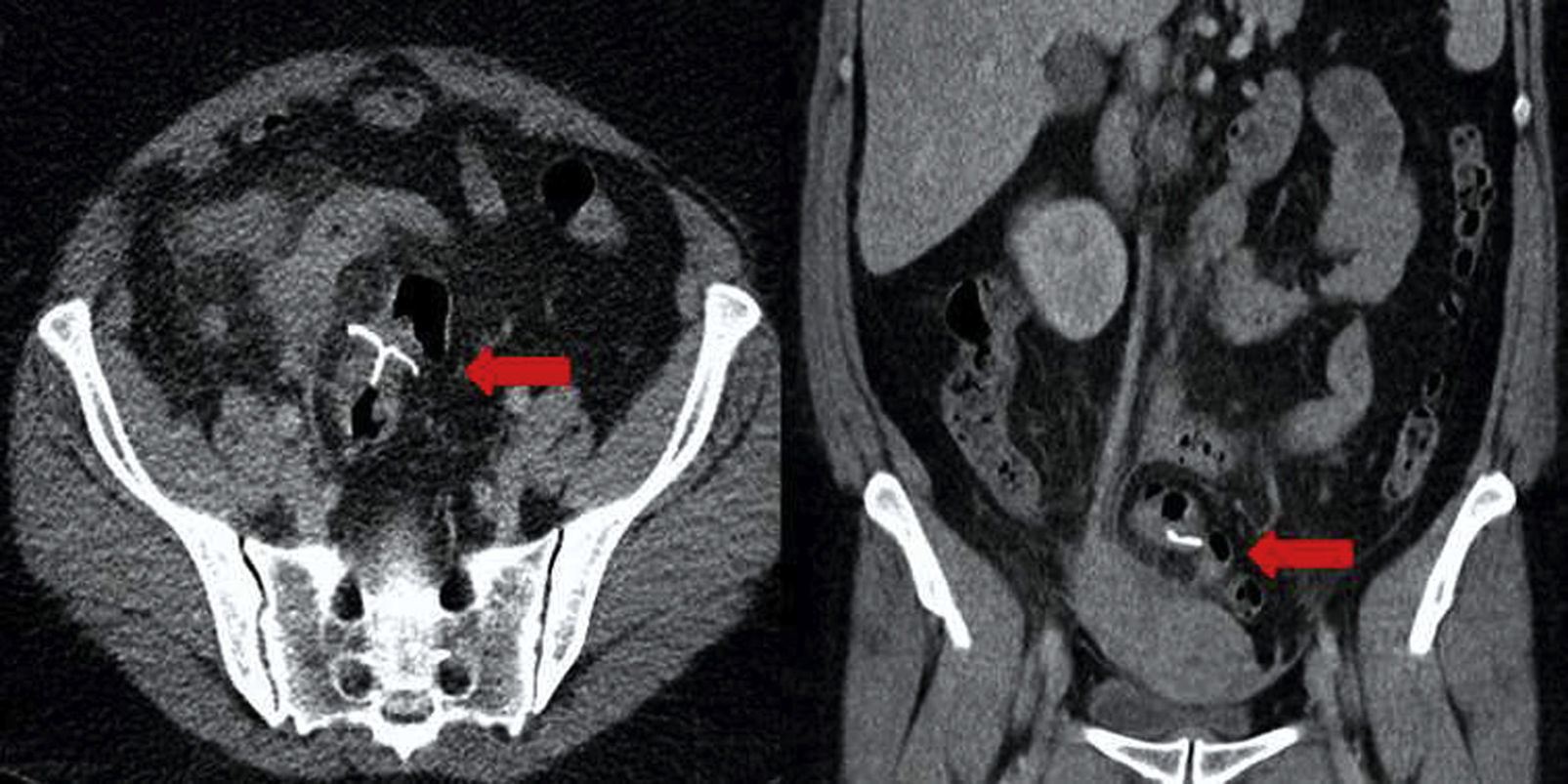
Plain abdominal X-ray identified the IUD in the pelvic cavity. Ultrasound revealed normal uterus and ovaries, with the IUD near the fundus of the uterus, without confirming the intrauterine position; computed tomography showed the IUD in the abdomen, outside the uterus, with no evidence of free air or fluid collection (Fig. 1).
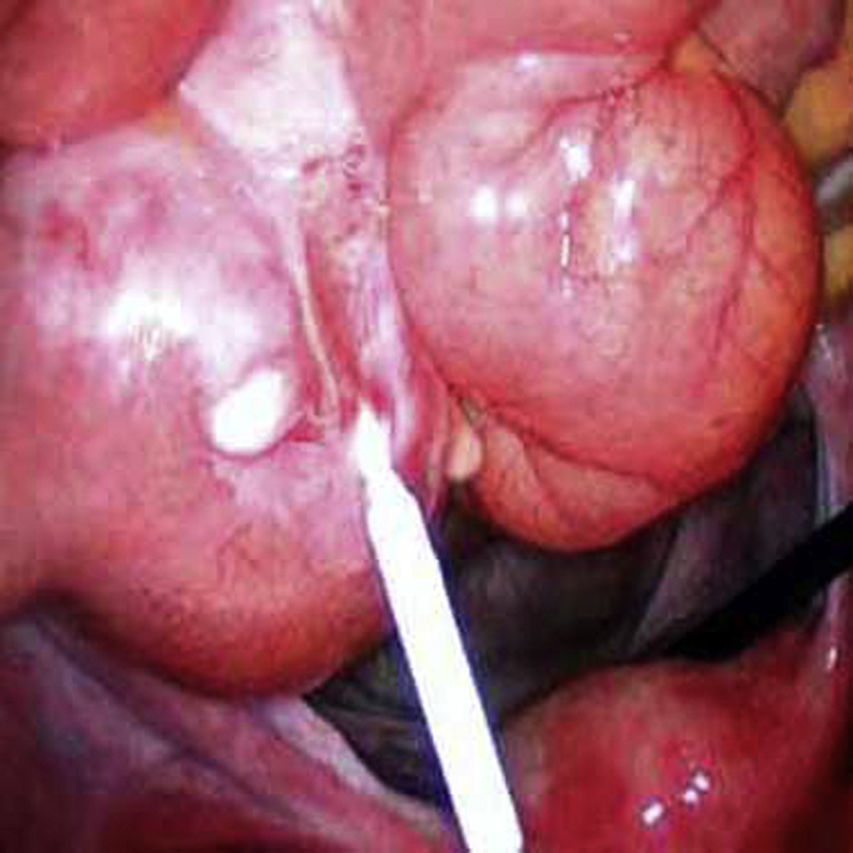
Laparoscopy was performed, finding the IUD embedded in the small bowel 10cm from the caecal valve, with the vertical portion exiting through the intestinal wall (Fig. 2). Laparoscopic resection of the affected bowel portion was carried out to completely remove the IUD, with termino-terminal anastomosis and no complications. The UP site did not require repair. Histopathological examination revealed the IUD embedded completely in the bowel wall, surrounded by granulation tissue and fibropurulent exudate, consistent with a chronic inflammatory response. The patient presented no complications and was discharged on the second postoperative day.
The discovery of an IUD in the peritoneum is almost exclusively associated with complete UP.3 Another more unusual possibility includes tubal migration of a linear IUD.4 There are several risk factors that contribute to UP: type of device, insertion technique, myometrial defects, nulliparity and history of abortion.2 Expulsion of the IUD is a rare event, occurring in the first year in between 3% and 10% of users. When the threads are not visualised in the external cervical orifice in the gynaecological examination, it is because the device is inside the uterus, but the threads are broken or tangled, the IUD has been expelled or is in the uterine wall or abdominal cavity.3
The triad of chronic abdominal pain, fever and intermittent diarrhoea with absence of the IUD are considered symptoms of bowel injury. Although abdominal pain is the most common symptom, one third of cases are asymptomatic.1 In the case of copper IUDs, the release of material from the IUD can cause abdominal pain, omental adhesions and bowel perforation.5
Ultrasound confirms the location of the IUD in the abdominal cavity. Accurate detection depends on several factors such as the type of IUD and uterine abnormalities.6 The characteristics of the artefacts (shadows) that help establish the location when direct visualisation is not possible should be taken into account. Plain abdominal X-ray can help in the localisation, and abdominal CT is indicated to locate the exact site and to determine complications such as perforation of neighbouring organs, adhesions and abscesses.7
Various studies recommend that all IUD be removed as soon as possible after diagnosis of UP and/or migration, regardless of the type or location. This is mainly due to their potential to form adhesions that cause chronic pain, intestinal obstruction and infertility. Another reason is migration to adjacent structures, leading to more laborious and complicated surgical removal.8 Copper IUDs are found in half of cases involving intestinal perforation. The intestinal areas most affected are the sigmoid colon, small intestine and rectum.2,9
Laparoscopy is the method of choice for the removal of intra-abdominal IUDs, although they cannot always be retrieved due to incomplete visualisation. Laparotomy is necessary when they cannot be found by laparoscopy. The IUD should be removed carefully and the bowel segment repaired.5 The bowel segment affected may occasionally be resected and termino-terminal anastomosis performed.1,5 Care must be taken not to remove it by pulling the threads, as it can cause intraperitoneal contamination with intestinal contents, with a risk of sepsis.1 Some cases in which colonoscopy has been used to remove devices in the rectum have been described.10
In summary, an IUD outside the uterus can be asymptomatic or present as acute abdomen after migration to the peritoneal cavity. UP should be considered in the differential diagnosis in any female patient presenting with abdominal pain who uses this type of contraceptive. Perforation of the small bowel by an IUD is a rare but serious complication.
Please cite this article as: Torres-Cepeda D, Reyna-Villasmil E. Perforación del intestino delgado por dispositivo intrauterino. Gastroenterol Hepatol. 2016;39:495–496.