Casos Clínicos en Gastroenterología y Hepatología
Más datosSynchronous cancers of the biliary duct system have been rarely described in the literature.1–3 Most of them involved the gallbladder and the common bile duct (CBD) and they have been linked to a congenital malformation where the pancreatic and bile duct merge outside the duodenal wall and they form a abnormally large distal CBD4 called pancreatobiliary maljunction (PBM).4 However, there is scarce information about true biliary duct system cancers not associated to PBM.1–3
We report a rare case of synchronous bile duct cancer not linked to PBM.
A 70 year-old man presented with jaundice and choluria 6 days before admission. He denied abdominal pain, nausea, vomiting or loss of weight. Physical examination only revealed jaundice and mild upper-quadrant abdominal pain. Laboratory tests showed elevated serum levels of aspartate aminotransferase and alanine aminotransferase (286U/L; normal range 10–41U/L and 288U/L; normal range 5–37U/L, respectively), total bilirubin 18.7mg/dl (normal range 0.3–1.3mg/dl), direct bilirubin 14.7mg/dl (normal range 0.0–0.4mg/dl), γ-glutamyltranspeptidase 798U/L (normal range 5–85U/L), alkaline phosphatase 1045U/L (normal range 50–136U/L). Carbohydrate antigen 19–9 levels were normal (4.6U/ml, normal value≤37U/ml).
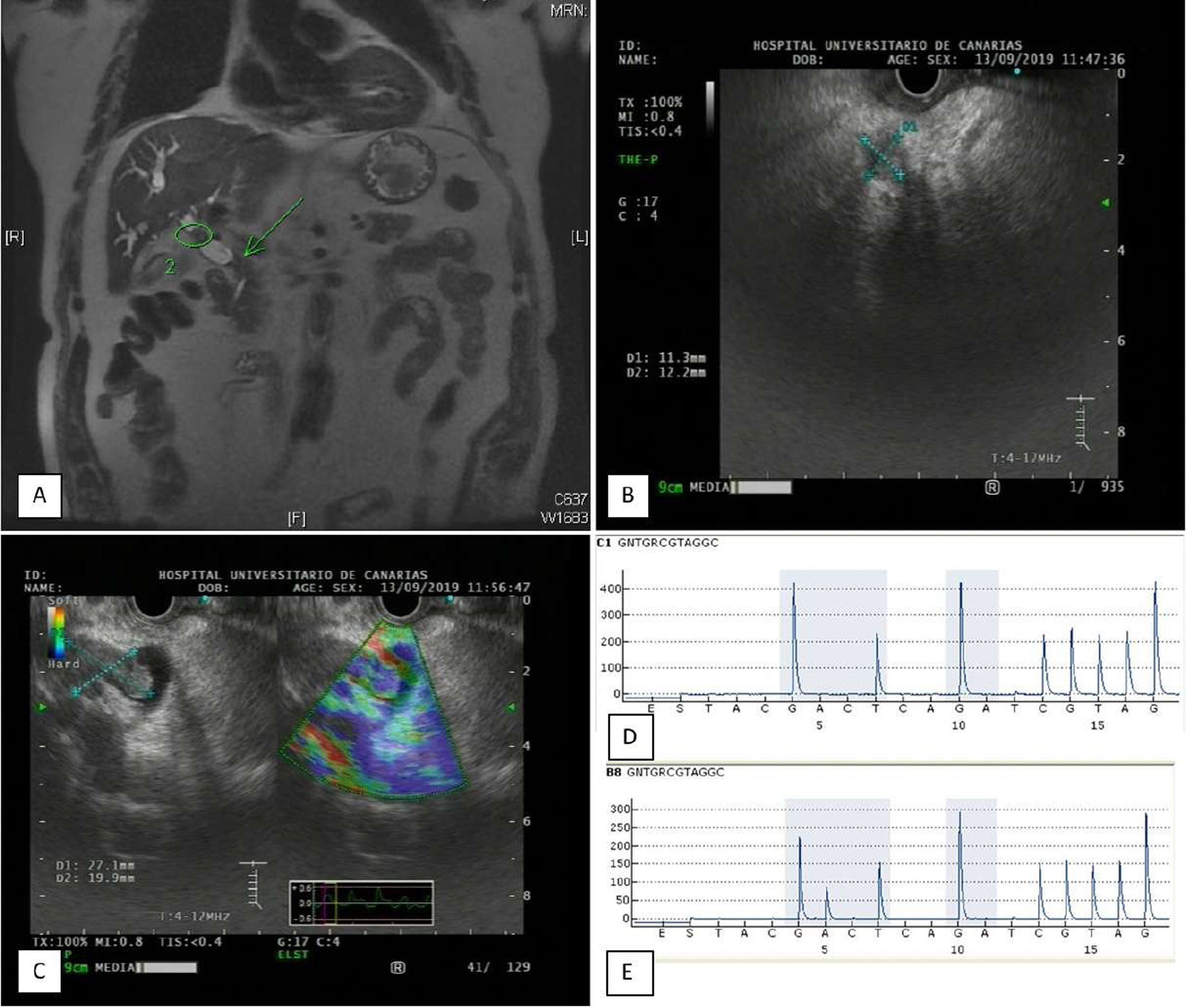
The magnetic resonance cholangiopancreatography (MRCP) revealed intrahepatic bile duct dilation, and a mass suggestive of a cholangiocarcinoma protruding at the level of the CBD bifurcation. In addition, another bile duct dilation was observed in the distal CBD, recommending further studies to rule out an obstructive cause at this level (Fig. 1a). No evidence of anomalous pancreaticobiliary duct union was found in the MRCP. The endoscopic ultrasound (EUS) showed a 9×9mm distal hypoechoic bile duct mass blocking the CBD and an exophytic hypoechoic mass of 27×20mm in size in the left hepatic duct protruding to the proximal CBD (Fig. 1b and c). A fine needle aspiration cytology (FNA) was carried out using a 22 gauge needle over the two masses. Cytological assessment revealed a neoplastic epithelial population (CK19+) mainly organized in irregular clusters exhibiting anisonucleosis, hyperchromasia and irregular vacuolization, being diagnostic of cholangiocarcinomas. However, whereas the distal cholangiocarcinoma had a wild type KRAS expression, KRAS was mutated (G12D) in the proximal one, suggesting a case of synchronous cholangiocarcinoma (Fig. 1d and e). A computerized tomography (CT) showed bilateral lung nodules suggestive of metastasis. A percutaneous transhepatic biliary drainage was performed (PTC). The patient died 2 months later.
(a) Magnetic resonance on the T2-weighted imaging (WI) showed a distal stenosis and dilation of the common bile duct (arrow) and a proximal tumoral mass. (b) Lineal endoscopic ultrasound image showing the distal bile duct stenosis. (c) Lineal endoscopic ultrasound image showing the proximal mass protruding into the proximal common bile duct (left image). The same mass is enhanced by elastography (right image). (d) Pyrogram trace of the codons 12 and 13 of KRAS oncogene from the distal cholangiocarcinoma. Notice the double hight of the G peak at position 4, characteristic of the wild type GGT sequence at codon 12 (left shadowed box). (e) Pyrogram trace of the codons 12 and 13 of KRAS oncogene from the proximal cholangiocarcinoma. Notice the presence of the A peak at position 5 resulting from the GGT>GAT mutation at the second base of codon 12 (left shadowed box).
The presence of double biliary tract system tumors is a rare condition. Most cases reported synchronous gallbladder adenocarcinoma and CBD cholangiocarcinoma and they are often liked to PBM. This condition predisposes to the reflux of pancreatic juice into the biliary tract, promotes genetic alterations and hyperproliferation resulting in biliary cancer. For the diagnosis of PBM, an abnormally long common duct and/or abnormal join of the pancreatic and bile duct should be shown by endoscopic retrograde cholangiography (ERCP), PCT or MRCP.4 In the present case no abnormality was detected by the PTC or the MRCP.
Warren and Gates described the criteria for multiple primary cancers5: (1) each tumor must present a definitive picture of malignancy, (2) each tumor must be distinct and (3) the probability that 1 is a metastasis of the other must be ruled out.
The present case seems to meet these criteria, since in both cases malignancy was confirmed by the cytological assessment; there was no connection between both tumors because one was a Klastkin tumor and the other one a distal cholangiocarcinoma with apparently normal and dilated bile duct in between; and finally, the molecular analysis excluded the possibility that one of the tumors was a metastasis from the other.
It is important to note that because of the rarity of these cases, they could not be easy to diagnose by the imaging techniques and some cases might be diagnosed in more advanced stages. In fact, in the case of Sumiyoshi et al.2 the distal lesion was diagnosed 11 months after the treatment of the proximal cholangiocarcinoma.
In summary, double biliary duct cancers are exceptionally found and not always easy to diagnose by imaging techniques. Awareness of this clinical presentation and a high suspicion of this disease are warranted to the proper management of these patients.
Conflicts of interestThere are not conflicts of interest.
We thank Dr. Eduardo Salido for his valuable comments.