Endoscopy activity has been dramatically reduced to minimum due to COVID-19 outbreak consequences. Endoscopy Units are experiencing shortages in staff, personal protective equipment (PPE), medical equipment as respiratory ventilators and monitors, beds or even physical space. Moreover, cleaning rooms have gained a new role of PPE (i.e. goggles, or face shield) disinfection from different hospital areas. For this reason, it is convenient to be prepared on how to resume non-urgent and non-delayable endoscopy activity and adapt to the natural evolution of pandemic.
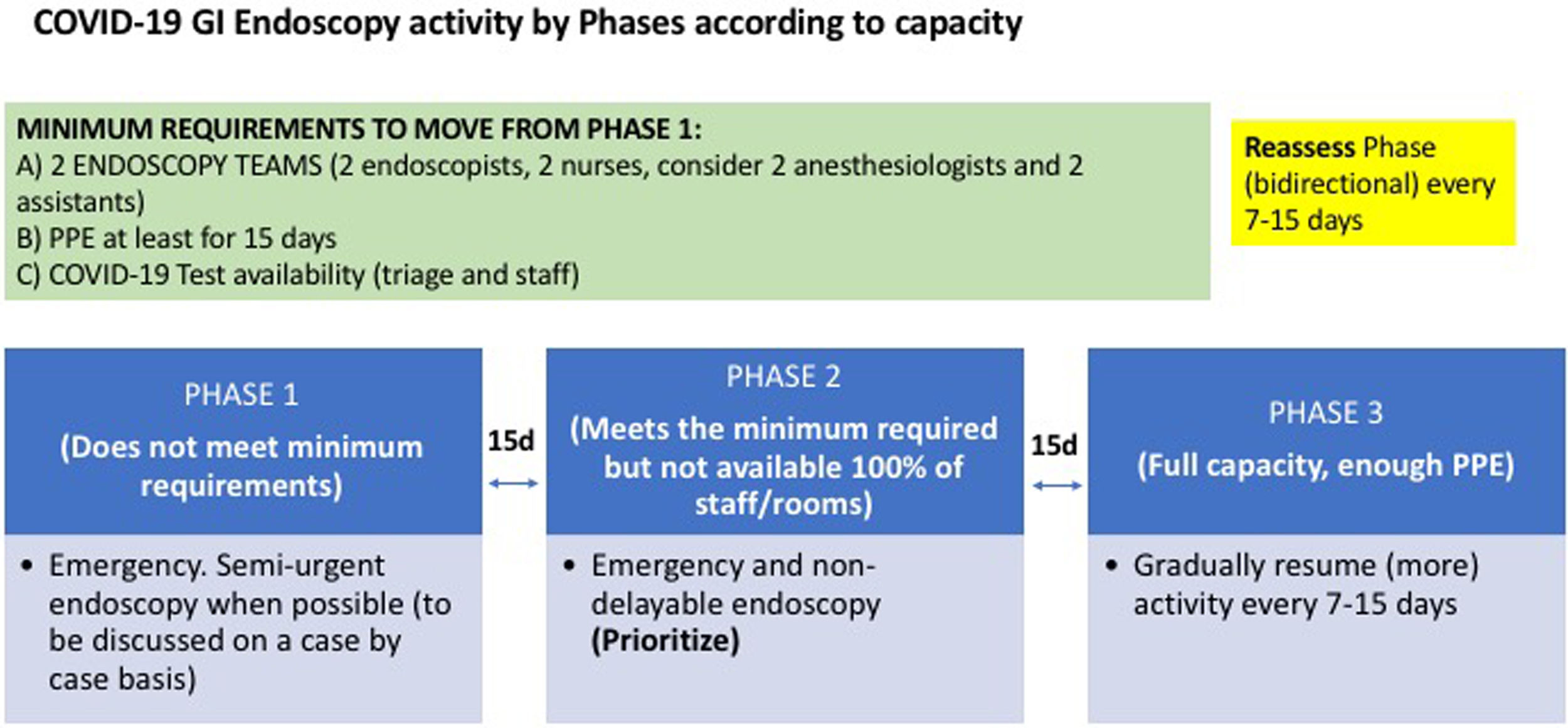
We recommend to progress to an adapted activity in a three-phase system.
For that, some minimum requirements are necessary to move forward on endoscopy activity, grouped in 3 basic needs: Workforce trained in endoscopic procedures, PPE availability and testing capacity for COVID-19 [Fig. 1]. The movement between the phases could be bidirectional depending on pandemic situation. So, the phases will be dynamic returning to a previous phase or progressing to an advanced phase.
With only one team available in the unit, it will be very risky planning to do semi-urgent endoscopy on a regular basis, considering the quarantine likelihood if health care workers get infected. On the other hand, to start assuming more schedule of procedures, it is necessary to expand the number of rooms depending on the capacity of the endoscopy unit. This may imply bringing personnel back from COVID-19 tasks.
Additionally, we are suffering shortages in PPE availability. PPEs are necessary for the COVID-19 era,1–3 and they should be used for every gastrointestinal endoscopy specially in high-risk areas. As its availability for a long time may be difficult to predict, we suggest that supplies should be guaranteed for at least 2 weeks before resuming more activity.
Another concern is the screening of staff and patients. Testing capacity is not widely available right now, but it is recommended to test healthcare workers and patients. As circuits may differ on COVID-19 status, testing might be necessary to detect asymptomatic positive cases and prevent patient-to-patient, staff-to-staff, patient-to-staff and staff-to-patient transmission, taking into account the possible false positives and false negatives due to the variability of the tests.
Once those minimum requirements are met, we could move forward to a second phase, doing priority endoscopic procedures on a regular basis according to a case-by-case management and high/low priority as it has been recommended by ESGE,1 SEED, SEPD, AEG4,5 and other societies. Depending on the pandemic evolution, the adaptation of endoscopy staff to second phase, and the endoscopy unit is reaching a full capacity with enough PPE, it will be possible to gradually assume more activity.
Because epidemiology and sociopolitical measures are continuously changing, we should reassess every 1 or 2 weeks (suspected incubation period6) our local status. And we should be prepared to move not only forward but backwards when needed.