Rupture of pseudoaneurysms is rare but can be life-threatening complications of acute or chronic pancreatitis, usually due to enzymatic digestion of vessel walls crossing peripancreatic fluid collections. We report the case of a 40 year-old female, with multisystemic lupus and anticoagulated for prior thrombotic events, admitted for probable cyclosporine-induced acute pancreatitis. Hemodynamic instability occurred due to abdominal hemorrhage from two pseudoaneurysms inside an acute peri-pancreatic collection. Selective angiography successfully embolized the gastroduodenal and pancreatoduodenal arteries. The hemorrhage recurred two weeks later and another successful embolization was performed and the patient remains well to date. The decision to restart anticoagulants and to suspend cyclosporine was challenging and required a multidisciplinary approach. Despite rare, bleeding from a pseudoaneurysm should be considered when facing a patient with pancreatitis and sudden signs of hemodynamic instability.
Os pseudoaneurismas são complicações raras mas graves da pancreatite aguda ou crónica. São causados pela digestão enzimática de artérias que atravessam colecções inflamatórias. Descreve-se o caso de uma doente do sexo feminino, de 40 anos, com lúpus sistémico e anticoagulada por trombose venosa profunda, admitida por pancreatite aguda associada à ciclosporina. Apresentou sinais de hemorragia abdominal causada por dois pseudoaneurismas dentro de uma colecção peri-pancreática. Foi então realizada angiografia com embolização da artéria gastroduodenal e pancreatoduodenal. Houve recidiva duas semanas depois, com necessidade de nova embolização bem-sucedida. A decisão de suspender a ciclosporina e reintroduzir anticoagulantes nesta doente de alto-risco é controversa. Apesar de raros, os pseudoaneurismas devem ser considerados perante um doente com pancreatite e sinais de hemorragia.
Most cases of pancreatitis are mild and have a favorable prognosis. However they can also be present with a severe form and have ominous complications. Vascular events range from asymptomatic venous thrombosis to severe life-threatening arterial bleeding.1 Hemorrhage from pseudoaneurysms is considered a quite rare complication of acute or more commonly chronic pancreatitis, which is thought to be caused by leakage of pancreatic enzymes that erode the wall of adjacent visceral arteries. The vessel wall may also be damaged by ischemia and compression by inflammatory or necrotic collections. A pseudoaneurysm may also occur after biliopancreatic surgery.2 The most frequently involved vessels are the splenic artery in about 30–60%, the gastroduodenal artery in 20–25% and the pancreatoduodenal artery in 10–15% of the cases. Involvement of the hepatic or left gastric arteries is even less common.3 Bleeding may occur into the gastrointestinal tract and present as melena or hematochezia through the main pancreatic duct (hemosuccus pancreaticus), into a pseudocyst/peripancreatic collection or into the peritoneal cavity. Pseudoaneurysm hemorrhage may occur from a few days to several years after the onset of pancreatitis.4
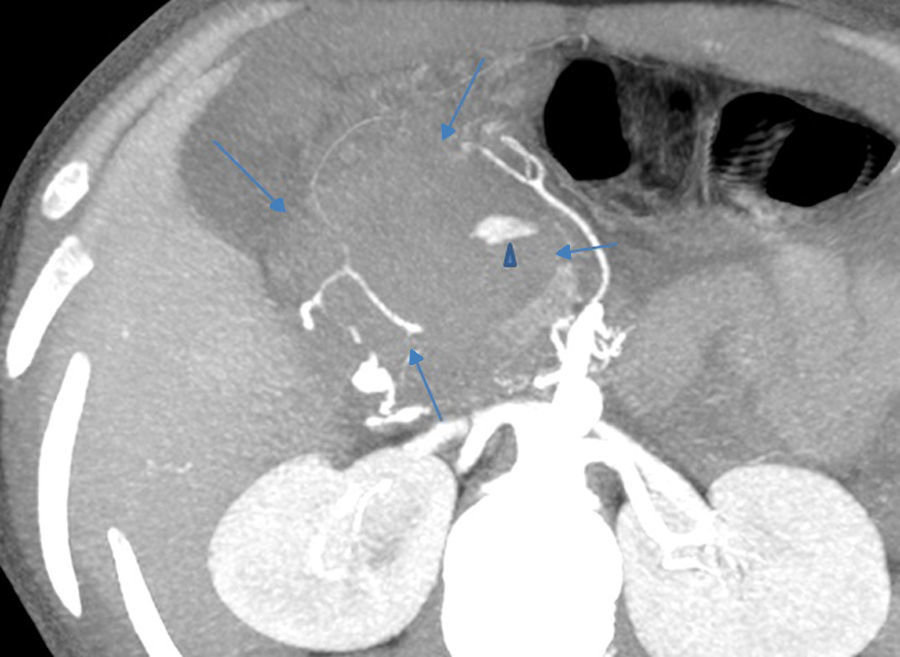
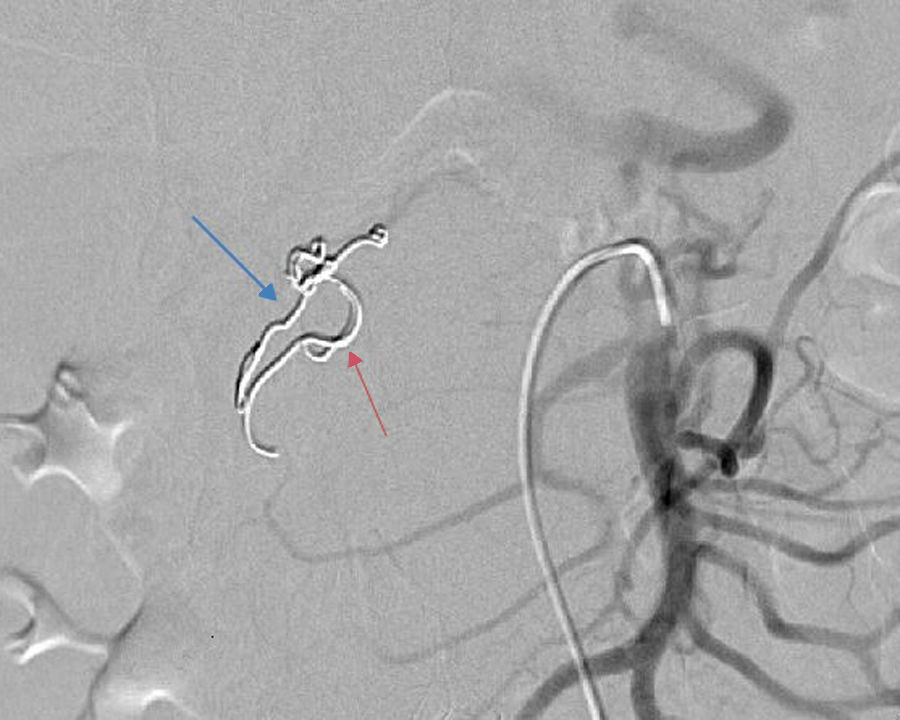
When this diagnosis is suspected, contrast-enhanced CT angiography is an excellent modality for identifying and locating the pseudoaneurysm as well as it can demonstrate features of chronic pancreatitis. It may show simultaneous opacification of an aneurysmal artery and pseudocyst or penetration of contrast within a pseudocyst after the arterial phase.5 This is necessary for subsequent selective angiography, the gold standard method for definitive diagnosis and treatment of pseudoaneurysms. Proximal embolization with coils is the preferred technique and has replaced surgical ligation of the damaged artery as the best method for treatment.6 Injection of a haemostatic gelatin sponge (spongostan®), cyanoacrylate, thrombin or placement of covered stents may also be useful. Published case series include a relatively low number of cases, but show that embolization is a safe method with high success rate and relatively low risk of recurrence or ischemia.7,8 To the best of our knowledge, there is only one other case report of a pseudoaneurysm complicating a probable drug-induced acute pancreatitis.3
According to Badalov classification,9 cyclosporine is a class III drug concerning the risk of inducing acute pancreatitis, which means that there are at least two known cases in medical literature, but with no consistent latency time between exposure to the drug and ensuing symptoms or evidence of positive rechallenge. Those cases occurred in post-transplant setting.10 Despite the paucity of clinical reports about cyclosporine-induced acute pancreatitis, there is an experimental model that suggests a deleterious role for the drug in pancreas transplant recipients, causing pancreatitis more often than tacrolimus.11 Since rechallenge is not an option due to obvious medical and ethical concerns, diagnosis of drug-induced pancreatitis relies on careful history taking and high index of suspicion.
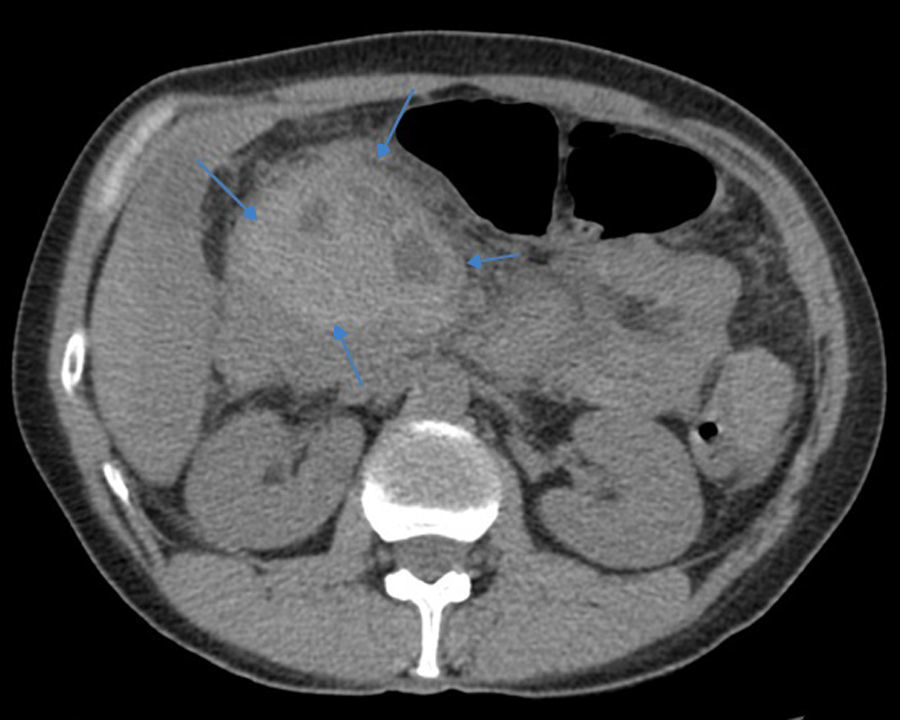
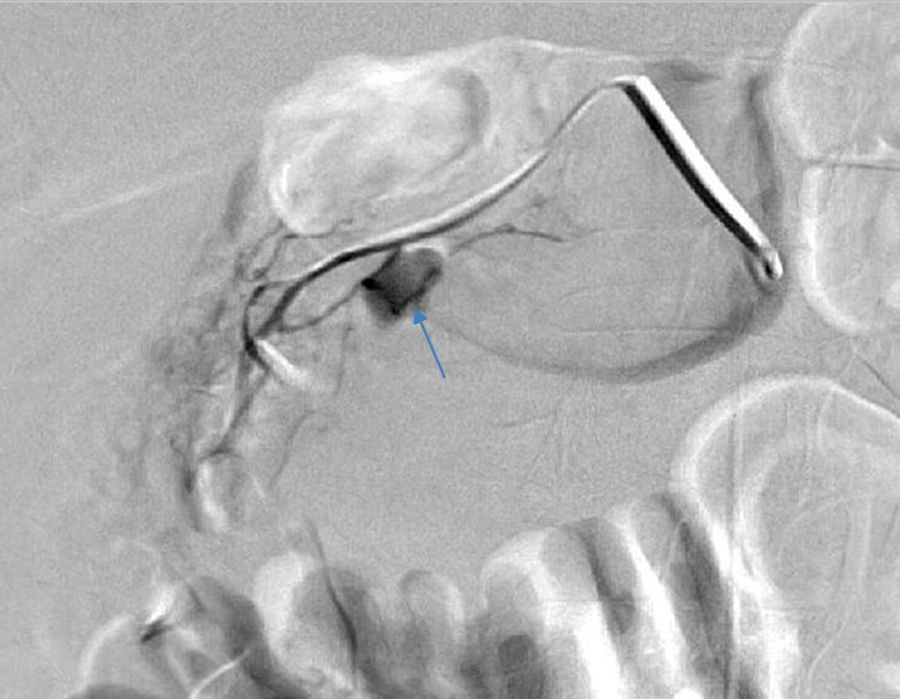
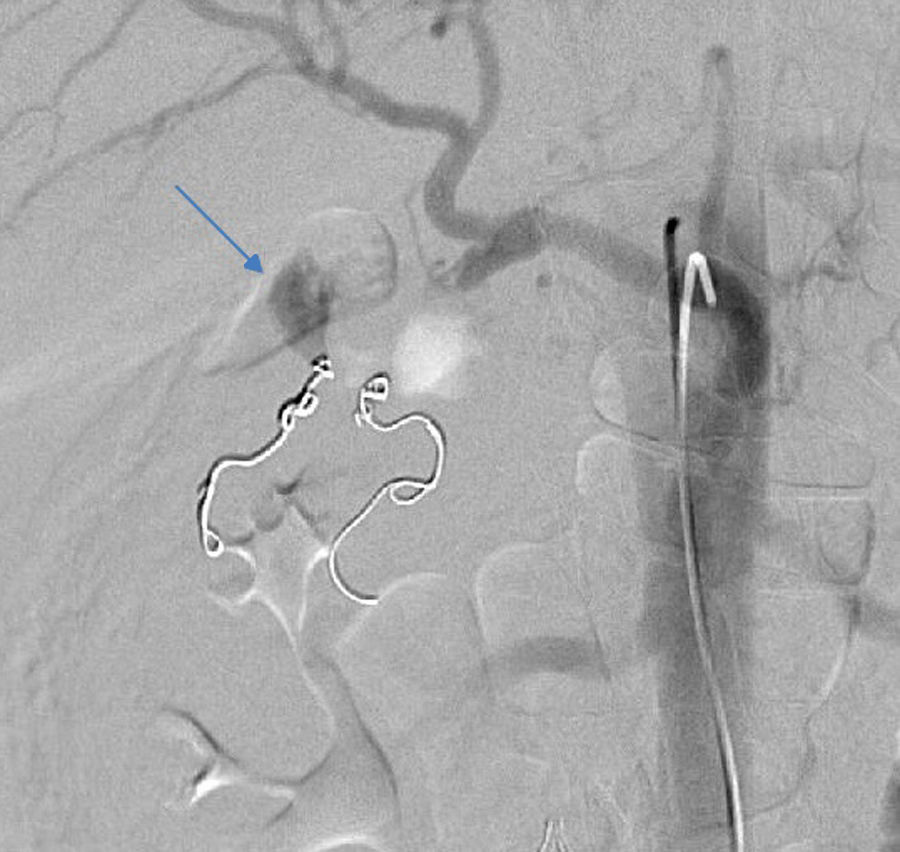
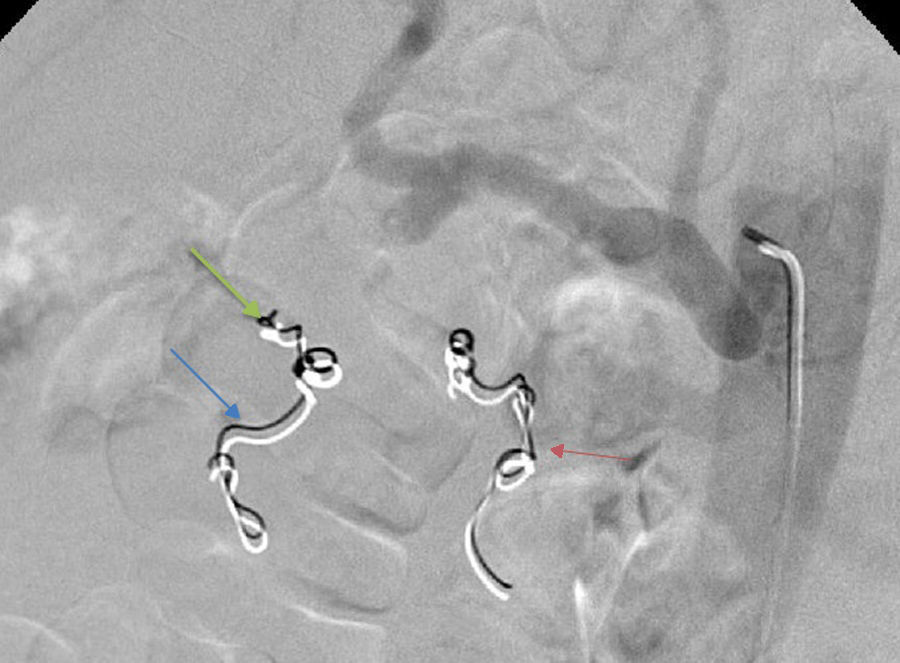
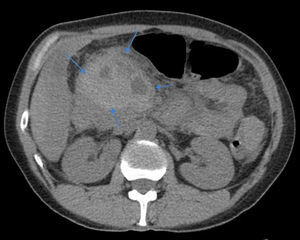
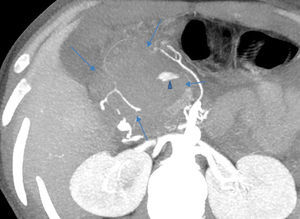
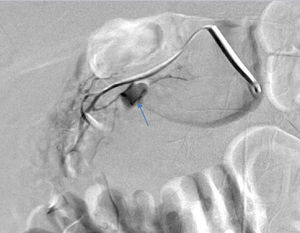
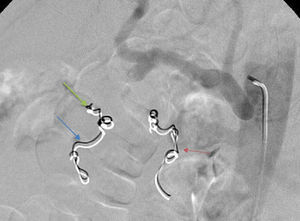
2Case reportWe present the case of a 40 year-old female patient with a medical history of severe systemic lupus erythematosus (SLE) and secondary anti-phospholipidic syndrome, with past episodes of venous thrombosis (pulmonary and deep venous thrombosis in 2008) that led to placement of a filter in the inferior vena cava and in the right iliac vein. The patient was anticoagulated with warfarin. She was also taking prednisolone, hydroxychloroquine, ramipril, sertraline and alprazolam. Due to lupus reactivation, she was recently medicated with cyclosporine. There was no history of alcohol consumption, familial history of pancreatitis, cholelithiasis or hypertriglyceridemia. There were also no previous endoscopic or surgical abdominal interventions. Two weeks after being prescribed with 150mg of cyclosporine, she was admitted to the emergency room with acute epigastric abdominal pain with lumbar irradiation, fever, nausea and vomiting that started four days before admission. Elevated levels of amylase and lipase (more than three times above the upper normal limit) supported the diagnosis of acute pancreatitis. There were no Ranson criteria at admission, BISAP score (bedside index for severity in acute pancreatitis) was zero and there were no signs of organ failure or SIRS (systemic inflammatory response syndrome). Three days after admission, the patient suffered a lipothymia and a brisk fall in her hemoglobin levels was noticed (from 119g/L to 64g/L). An abdominal CT was conducted revealing a peripancreatic acute fluid collection with active bleeding within (Figs. 1 and 2). The collection developed about a week after disease onset. It was located close to the bifurcation of the gastroduodenal artery into the right gastroepiploic artery and the anterior superior pancreaticoduodenal artery. The patient was transferred to our center for an angiography of the celiac trunk and superior mesenteric artery. Two pseudoaneurysms in the gastroduodenal and pancreatoduodenal arteries with active bleeding were diagnosed and successfully embolized with two coils (Figs. 3 and 4). The procedure was successful and there were no signs of iatrogenic regional ischemia, which could occur due to limited blood supply caused by the embolization. Initially, the patient was unstable, but her hemodynamic status improved with adequate fluid resuscitation, fresh plasma and packed red blood cells transfusion. After controlling the hemorrhage, it was decided to immediately restart anticoagulation, given the major risk of thrombosis in a patient with phospholipidic syndrome and a filter in the inferior vena cava. The following week was uneventful and the patient was discharged and told to maintain the same medication, including cyclosporine and enoxaparin. About one week after being discharged, the patient had a recrudescence of the abdominal pain and was again admitted to her local hospital. In the following day, a new sudden fall in hemoglobin levels occurred (123g/L to 48g/L) and a second angiography was performed. Again there were signs of active bleeding into the peripancreatic collection and the gastroduodenal artery was embolized with a third coil (Figs. 5 and 6). The procedure was successful and there was a favorable evolution with no signs of hemorrhage until discharge. After consulting with the patient's Rheumatologist, it was decided to stop cyclosporine as it probably caused the pancreatitis. Until this date, the patient remains well and without further complications.
Several issues regarding this case merit careful analysis. First, the etiology of the pancreatitis should be discussed. After a thorough medical history, most causes of pancreatitis were excluded. The patient had no history of alcoholism or smoking, recent acute illness, abdominal trauma or surgery. There was no familial history of pancreatitis. She denied complaints of long-standing abdominal pain, weight loss or steatorrhea that could suggest chronic pancreatitis. Laboratory analysis excluded hypertriglyceridemia and hypercalcemia as potential causes as well. There was no elevation of hepatic enzymes or bile duct dilation suggestive of microlithiasis. Abdominal ultrasound and CT scan showed no signs of cholelithiasis, bilio-pancreatic lesions or chronic pancreatitis (CP). However, in early stage CP, imaging methods may show only minimal changes. Endoscopic ultrasonography (EUS) has been shown to be highly accurate for the identification of gallbladder sludge/microlithiasis, common bile duct stones, and pancreatic diseases (pancreatic neoplasms and chronic pancreatitis)12 and would be useful to exclude these diagnoses in our patient. In patients considered to have idiopathic acute pancreatitis, after negative initial work-up for biliary etiology, EUS is recommended as the first step to assess for occult microlithiasis, neoplasms and chronic pancreatitis.13
Concerning medication, only cyclosporine was recently introduced. Prednisolone and ramipril are also potential agents of drug-induced acute pancreatitis. However, the patient was taking these medications for over three years. The remaining medication (warfarin, hydroxochloroquine, sertraline and alprazolam) were also prescribed a few years before this episode. It seems more likely that cyclosporine was the culprit due to the short lapse of time between starting this medication and the beginning of clinical manifestations. This is consistent to what is described in one of the case reports of cyclosporine-induced pancreatitis. This supports our hypothesis as consistent latency time among cases is one of the criteria suggested in Badalov classification.9 Drug-induced acute pancreatitis is a rare entity, difficult to diagnose since it has no distinguishing clinical features. Several distinct mechanisms were suggested and include direct toxic effect (such as furosemide), immunologic reaction (with 6-mercaptopurine or aminosalicylates), ischemia (for azathioprine), increased viscosity of pancreatic fluids (e.g., corticosteroids) intravascular thrombosis (with estrogens) or accumulation of a toxic metabolite (drugs such as valproic acid or tetracyclines).14 Due to this variety of causative mechanisms, the time between exposure to the drug and initial symptoms may be as short as a few days for immunologic reactions or even several months if there is slow accumulation of toxins. There was no eosinophilia or skin rash, but these findings are seldom found in such cases.
Another possible etiology for this episode is lupus pancreatitis. It is a quite rare and ill-defined entity. It has no specific diagnostic criteria and it usually occurs during a flare of SLE. Usually its treatment is based in high-dose corticosteroids.15 The patient recently had a flare of SLE. However, her full recovery from it and being medicated with a potent immunosuppressive agent like cyclosporine and a low dose of corticosteroids argue against this diagnosis. Furthermore, according to the patient's Rheumatologist, there were no signs of a new SLE flare when the pancreatitis occurred – absence of cytopenias, rash, renal or neurological abnormalities. Due to the quiescent status of SLE, it was considered relatively safe to suspend cyclosporine. The risk of a new episode of pancreatitis and hemorrhage was considered more significant and life-threatening than the risk of a new flare of SLE.
Another pertinent clinical issue was the decision to reinstate anticoagulation. When peritoneal hemorrhage was first suspected, anticoagulation was suspended but after the first embolization, it was decided to restart it a few hours later. The recurrence of the hemorrhage was probably bolstered by this decision. However, given the very high risk of thrombosis due to the phospholipidic syndrome and two vascular filters, it would be at least equally risky not to restart anticoagulation. In these high-risk patients, the decision to suspend or restart anticoagulation should be made in a case-by-case basis. In our patient's case, the first angiography was successful and there were apparently no technical issues that could have contributed to the rebleeding episode. There is probably no advantage in switching to the new oral anticoagulants (NOACs), as their risk of gastrointestinal or abdominal bleeding is at least similar to older vitamin K antagonists.16
Both angiographies were life-saving procedures for our patient. This case highlights the importance of having a 24-hour interventional radiology team on call with expertise in these procedures. When available, angiography with embolization is usually the preferred method to perform hemostasis. Its success rates are high but rebleeding is not an uncommon event (up to 19–23%).17 Surgery remains an important treatment modality especially in massive bleeding, after embolization or stenting failure or for treatment of the underlying condition (e.g., bleeding from a post-operative pseudoaneurysm).
In conclusion, when evaluating a patient admitted for an acute pancreatitis with a severe gastrointestinal bleeding, hemoperitoneum or hemodynamic instability, hemorrhage from a pseudoaneurysm should be suspected and immediately treated if present. To the best of our knowledge, this is only the second described case of hemorrhage from a pseudoaneurysm after drug-induced acute pancreatitis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.