Gastrointestinal foreign bodies (FB) are comprised of food bolus impaction and intentionally or unintentionally ingested or inserted true FB. Food bolus impaction and true FB ingestion represent a recurrent problem and a true challenge in gastrointestinal endoscopy. More than 80–90% of the ingested true FB will pass spontaneously through the gastrointestinal tract without complications. However, in 10–20% of the cases an endoscopic intervention is deemed necessary. True FB ingestion has its greatest incidence in children, psychiatric patients and prisoners. On the other hand, food bolus impaction typically occurs in the elderly population with an underlying esophageal pathology. The most serious situations, with higher rates of complications, are associated with prolonged esophageal impaction, ingestion of sharp and long objects, button batteries and magnets. Physicians should recognize early alarm symptoms, such as complete dysphagia, distressed patients not able to manage secretions, or clinical signs of perforation. Although many papers are yearly published regarding this subject, our knowledge is mainly based on case-reports and retrospective series. Herein, the authors summarize the existing evidence and propose an algorithm for the best approach to FB ingestion.
A definição de corpo estranho gastrointestinal compreende a ingestão acidental ou voluntária de verdadeiros corpos estranhos e o impacto alimentar. Estas entidades representam uma recorrente e desafiadora problemática para os Gastroenterologistas. Em mais de 80 a 90% dos casos referentes à ingestão de verdadeiros corpos estranhos, o mesmo passa através do tubo digestivo sem complicações. No entanto, em 10 a 20% dos casos é necessária uma intervenção endoscópica. A ingestão de verdadeiros corpos estranhos apresenta o seu pico de incidência em crianças, doentes com perturbações psiquiátricas e reclusos. Por outro lado, o impacto alimentar ocorre tipicamente na população idosa, que, na maioria dos casos apresenta uma patologia esofágica subjacente. As situações mais frequentemente associadas a complicações sérias relacionam-se com a presença prolongada de corpos estranhos ou impacto alimentar no esófago, ingestão de corpos estranhos pontiagudos, compridos, pilhas ou ímanes. O médico deve reconhecer precocemente sinais de alarme tais como disfagia completa, incapacidade de deglutir saliva ou sinais clínicos de perfuração. Apesar da publicação anual de artigos referentes a este tópico, a maioria da evidência existente na atualidade apoia-se apenas em case-reports e séries retrospetivas. Este artigo pretende resumir de modo conciso a evidência atual e propor um algoritmo versando o tratamento endoscópico de verdadeiros corpos estranhos e impacto alimentar do trato digestivo superior.
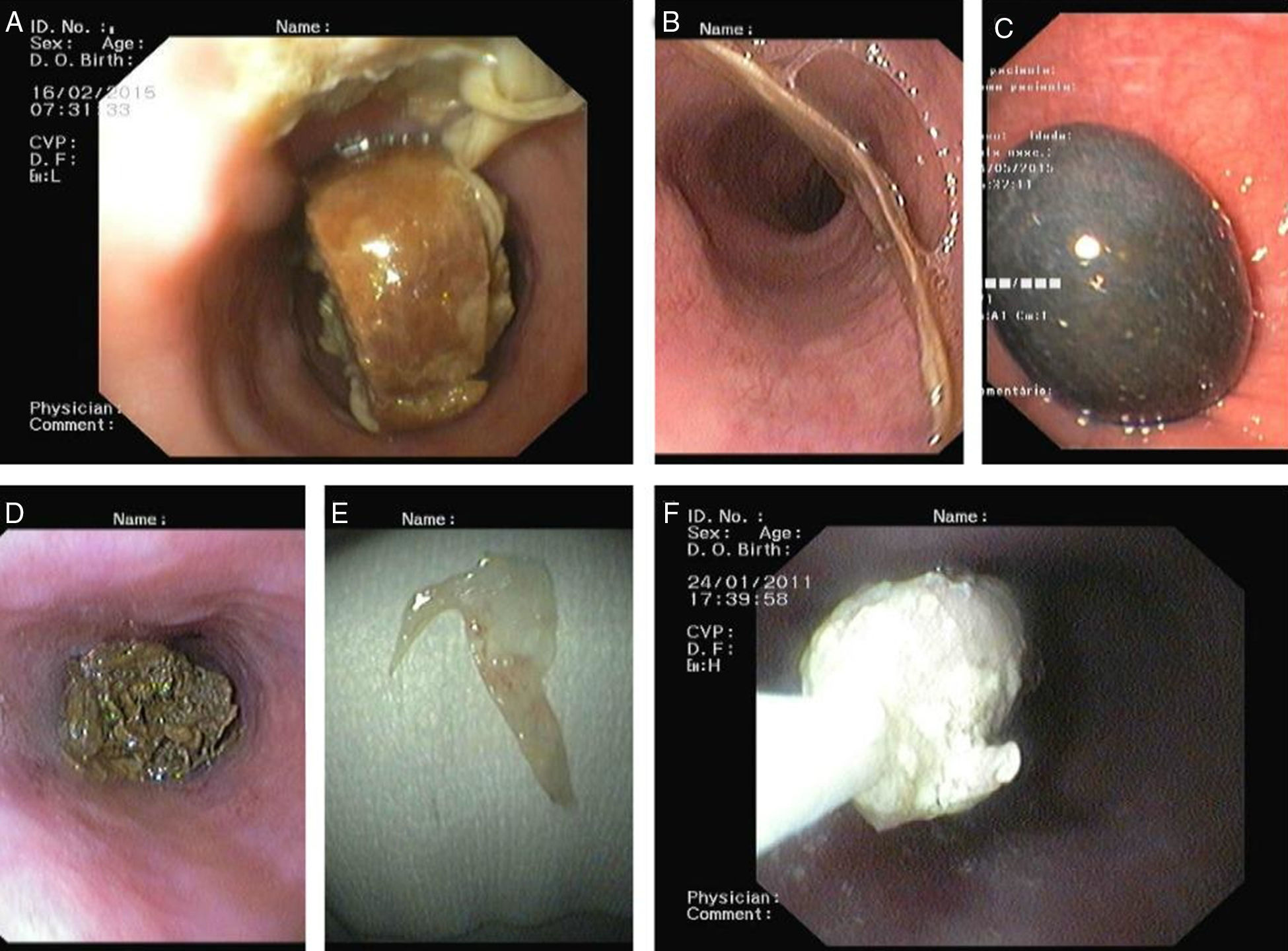
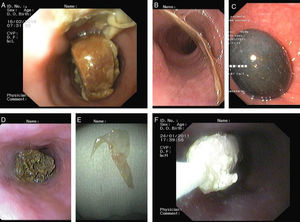
A foreign body (FB, from the Latin corpus alienum) refers to any object that was originated outside the body. Most of the references to FB involve their entrance through natural orifices into hollow organs, thus one of the most common locations for a FB is the digestive tract. The exact incidence of FB ingestion in children and adults is unknown. Annually it is estimated that 1500 deaths occur due to upper gastrointestinal FB ingestion.1 Food bolus impaction is the most common gastrointestinal FB, with an estimated incidence of 16 per 100000persons/year.2 Most of the food impactions (>75%) occur in adults after the fourth decade of life3 and the majority of them have an underlying esophageal motility disorder and/or esophageal luminal pathology (e.g., strictures, rings, webs, diverticula, anastomoses and cancer).2,4–9 Of note, in young adults there is a greater incidence of eosinophilic esophagitis presented at the time of food impaction (10%).8,10 It is estimated that 80% of the non-food or true FB ingestion (mostly coins, buttons, small toys and marbles) occur in the pediatric population due to natural oral curiosity, between the ages of 6 months and 3 years.11,12 Among the adult population, accidental ingestions occur with increased frequency in those who have dental appliances or impaired mental status (elderly, demented or intoxicated patients).13 Iatrogenic foreign bodies are an increasing problem and some of the culprit objects are capsule endoscopy devices, migrated luminal stents, gastrostomy buttons, catheters and dentistry material.13,14 Intentional true FB ingestions occur in the psychiatric patients, prisoners and drug dealers – “drug mules” or “body packers”.15,16 This subset of patients often ingest multiple, complex objects and display a recurrent pattern (Fig. 1).15,17 The FB most commonly swallowed by adults are: fish bones (9–45%; Fig. 2B and E), bones (8–40%) and dentures (4–18%; Fig. 3B and C).18–20 Fortunately, about 80–90% of the ingested FB passes spontaneously and uneventefully.21–23 On the other hand, 10–20% will require endoscopic intervention and approximately less than 1% will require surgical intervention.21 Topographically, the esophagus is the location where most complications occur. Potential complications include perforation, mediastinitis, fistula and aspiration. The complication rate from esophageal FB is directly proportional to the time spent in the esophagus. There are four areas of natural narrowing in the esophagus where impactions usually occur: upper esophageal sphincter, at the level of the aortic arch, crossing of the main stem bronchus and the lower esophageal sphincter. Sharp objects are the most dreaded in the stomach and duodenum. This type of objects are associated with a perforation rate up to 35%.24 Objects greater than 2cm in diameter or longer than 5cm will have difficulty traversing the pylorus, passing through the duodenal sweep, the ligament of Treitz and ileocecal valve.
Twenty-nine year-old prisoner male admitted for voluntary ingestion of multiple metallic foreign bodies. Before endoscopic intervention (A), abdominal radiograph shows multiple metallic objects scattered throughout the gastrointestinal tract. After endoscopic retrieval (B–D): multiple screws, nails, keys, finger ring, pieces of a metallic TV antenna and razor blades were retrieved. Patient was discharged with uneventful outcome.
In adults who are communicative, the history will often provide reliable details regarding the time and type of object ingested. Patients may localize discomfort with poor correlation to the site of impaction.23 In contrast to true FB ingestion, food bolus impactions are almost always symptomatic due to partial or complete esophageal obstruction, and they include subesternal chest pain, dysphagia, gagging and vomiting. Drooling and inability to handle oral secretions may occur in complete obstruction. Of note, adults who swallow non-food FB may not provide a reliable history because they can be mentally impaired or have swallowed items for secondary gain. Children may be asymptomatic (20–40%) and in up to 40% of the cases caregivers do not give history of ingestion.11 In this population, symptoms can be subtle like drooling, poor feeding, irritability and failure to thrive. The physical examination, in both children and adults, does little to aid in the diagnosis but it is important in identifying any complication. If an impaction has occurred proximally in the esophagus and compresses the trachea, wheezing and stridor may be present. Crepitus in the neck may be present in patients with esophageal perforation. Bowel perforation may result in signs of peritonitis. For radiopaque FB, a simple radiographic study might provide crucial information, such as the number, size, location and direction of the FB.25,26 Additionally, radiographs (neck, chest and abdominal) are useful to show perforations, some metal objects and bones.23,27 When one or more FB are identified by an index radiograph, serial radiographs may also provide information regarding FB passage throughout the gastrointestinal tract and the complications resulting from it. Physicians should bear in mind that the presence of fish or chicken bones, glass, wood and thin metals cannot be ruled out by plain radiographies.19,23,25–28 Because false-negative rates with plain film radiographs are as high as 47% in cases of FB suspiction24,29 and 87% in cases of food bolus impaction,30 even after negative or inconclusive findings on radiographic imaging, every patient with a clinical suspicion of a FB or food bolus impaction should undergo endoscopy. In case of perforation suspicion and for the evaluation of non-radiopaque FB, computed tomography (CT) should be preferred to plain radiographs.23,27,31 CT scan can also provide information regarding complication and treatment options. Moreover, endoscopy provides information regarding the presence of underlying pathology, mucosal damage due to the FB/food bolus and can assist in the resolution/dislodgement of the FB or food bolus. When a sharp or pointed FB ingestion is suspected, after a negative initial oro- and hypopharynx careful inspection, a CT scan should be the next diagnostic step.32 Barium studies are not indicated and should be avoided, as it will undermine the endoscopic examination. In patients with persistent symptoms, an endoscopic evaluation should be performed, even if the radiographic studies were negative. Endoscopy is the modality of choice for the diagnosis and management of suspected FB ingestion as the accuracy is near 100% due to direct visualization.
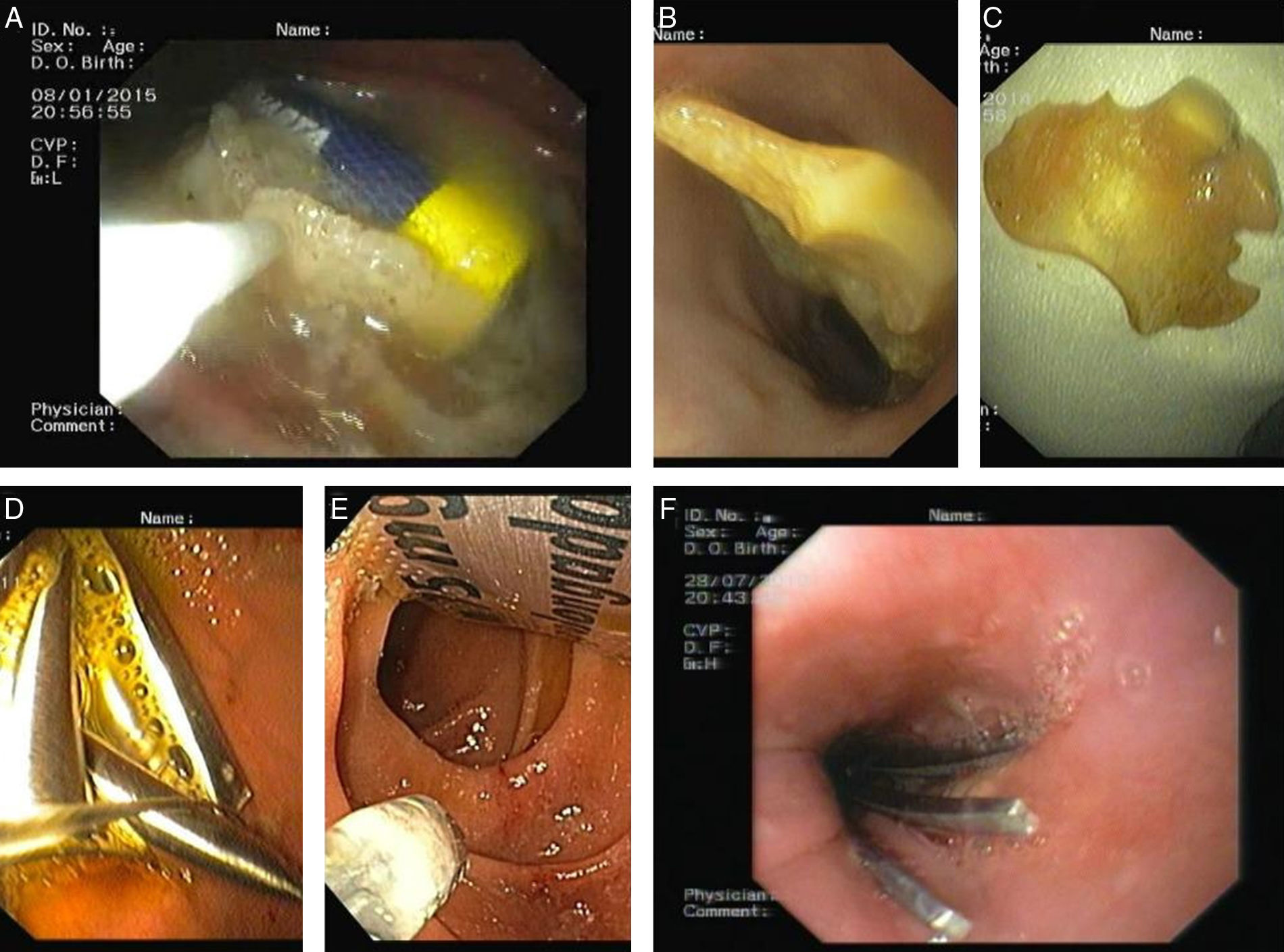
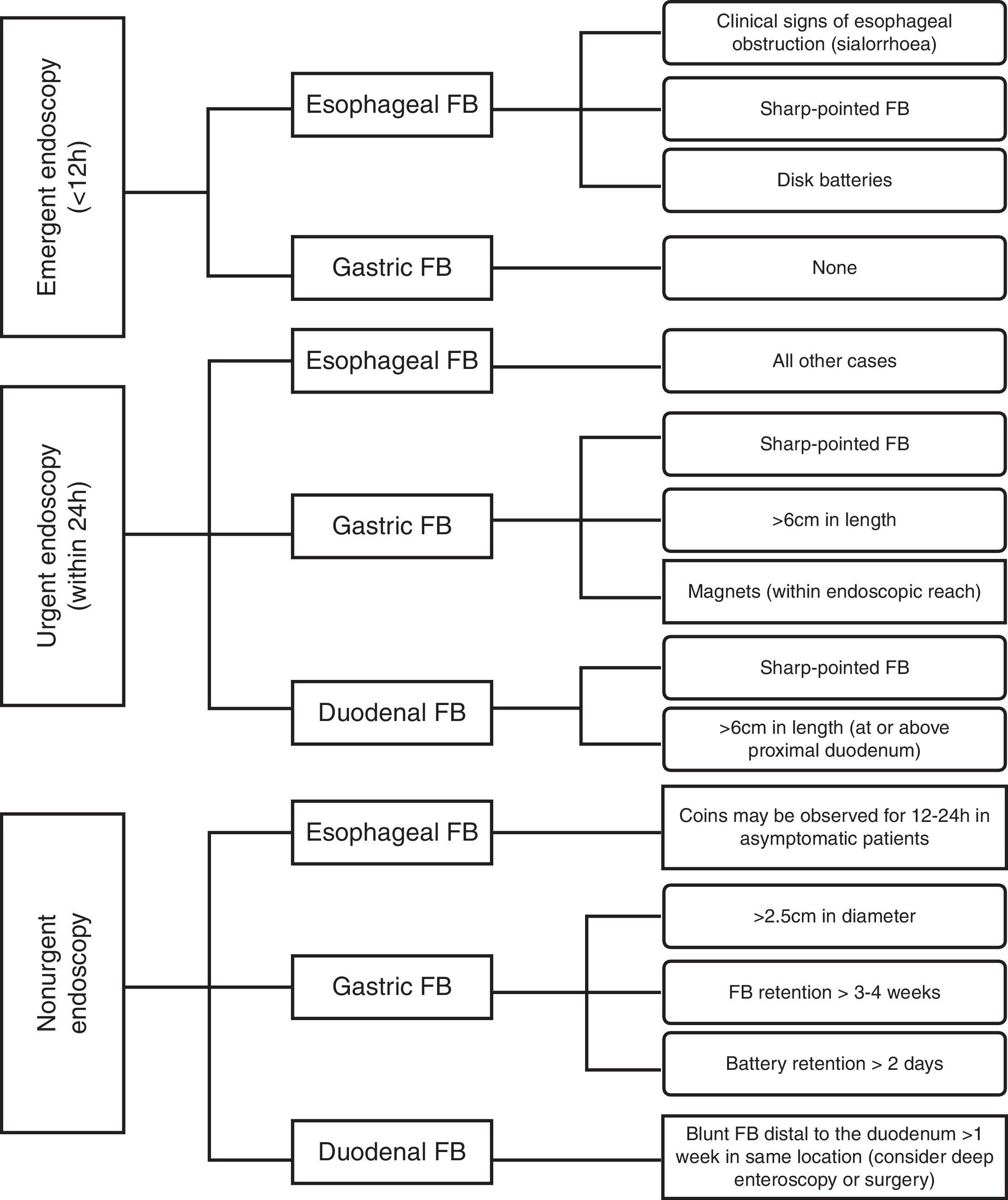
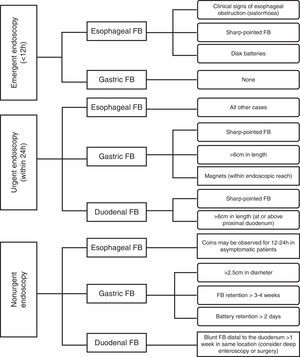
3Endoscopic management3.1Indication, timing and proceduresEndoscopy provides the most accurate diagnostic method in suspected FB ingestion and food bolus impaction.23,33 Endoscopic intervention is deemed necessary in one out of five cases of FB ingestion.3,4 In general, all esophageal FB and food impactions require urgent or emergent endoscopic intervention.34 Because the time that a FB remains in the esophagus is directly related to an increase in complications rates,35,36 they should be removed within 24h,37 preferably within 6–12h after presentation (Fig. 4). In most occurrences, conscious sedation is adequate in order to perform the endoscopic procedure,3 however, surgical consultation and endoscopy under general anesthesia should be considered in patients in whom the duration of the endoscopic procedure for the resolution of an esophageal FB impaction is unpredictable.21 Airway protection should always be considered for patients undergoing endoscopic FB removal. Oropharyngeal suction is required to avoid pulmonary aspiration. Patients with impactions in the upper esophagus may necessitate endotracheal intubation and an overtube in order to protect the airway. Laryngoscopes should be available in case an airway obstruction develops. Otorhinolaryngologists should be involved at an early phase in the management of FB above or at the level of the upper esophageal sphincter. After a failed attempt with flexible endoscopy, a rigid hypopharyngoscopy with compatible forceps can be used for FB retrieval. Endoscopists should recognize some high-risk features that demand an urgent approach: involvement of the upper third of the esophagus, symptoms of complete obstruction (e.g., a patient who is unable to handle secretions) and at-risk objects (e.g., sharp-pointed objects, food bolus impaction and button batteries).23 Foreign bodies that have reached the stomach have a chance to be evacuated spontaneously. Therefore, endoscopic removal of FB in the stomach should only be considered in case of dangerous FB, to avoid them passing the duodenal sweep, or all objects with a diameter larger than 2.5cm.23 Blunt or small objects should be removed only if they are still present after 3–4 weeks.23 When a sharp object has passed the pylorus, perforation may occur in the duodenum or at the ileocecal valve, thus removal should be considered if in the proximal duodenum.38,39 A blunt object remaining in the duodenum for 8 days or greater than 6cm of diameter, should be removed to avoid ischemia and other complications.23 Sharp objects that passed the duodenal curve should be followed daily with radiographs and surgical removal be considered if the FB fails to progress in 3 days. Before initiating endoscopic therapy, the endoscopist should be aware of the type of FB that will be encountered and plan the safest method for retrieval. It may be beneficial to perform a simulation ex vivo to select the best retrieval device.4 In uncooperative patients or patients who have ingested multiple complex objects, intravenous conscious sedation is adequate, but monitored anesthesia care or general anesthesia assistance may be required. In the pediatric setting, general anesthesia with orotracheal intubation is frequently used to remove FB from the upper gastrointestinal tract. Proper documentation and informed consent is important to reduce liability in the event of litigation. Multiple nonendoscopic therapeutic approaches have been studied. Glucagon, given in doses of 0.5–2.0mg, can induce relaxation of the esophageal smooth muscle and the lower esophageal sphincter, allowing the FB or the impacted food to pass.40,41 Success rates in food bolus impactions with glucagon (1mg, intravenously) as primary therapy ranged from 12% to 58%.42–44 Hyoscine butylbromide (butylscopolamine) use in the management of esophageal soft food bolus impaction is reported in three published studies. All of these studies concluded that there was no significant difference in disimpaction rate between those patients treated with hyoscine butylbromide and those who received no treatment.45–47 In the removal of complex or large FB, butylscopolamine is often given to induce aperistalsis. Carbonated beverages are used with the theoretical mechanism of carbon dioxide gas release that distend the lumen and act as a piston to push the object from the esophagus into the stomach, however the effectiveness of this method is unreliable and anecdotal perforations have been reported.48,49 Papain, a meat tenderizer is not recommended due to the lack of efficacy and risk of perforation and mediastinitis.50 Interventional radiographic methods, such as the use of a Foley catheter to extract FB or impacted food bolus are not recommended unless flexible endoscopy is not available.51 Endoscopy is incontestably the best method for the therapeutics of true FB ingestion and food bolus impaction. The success rates are greater than 95% and associated morbidity and mortality range from 0% to 5%.2,4,5,7,52–54 The most consistent predictors of treatment failure and complications include intentional ingestion, ingestion of multiple and complex FB and lack of patients’ cooperation.55
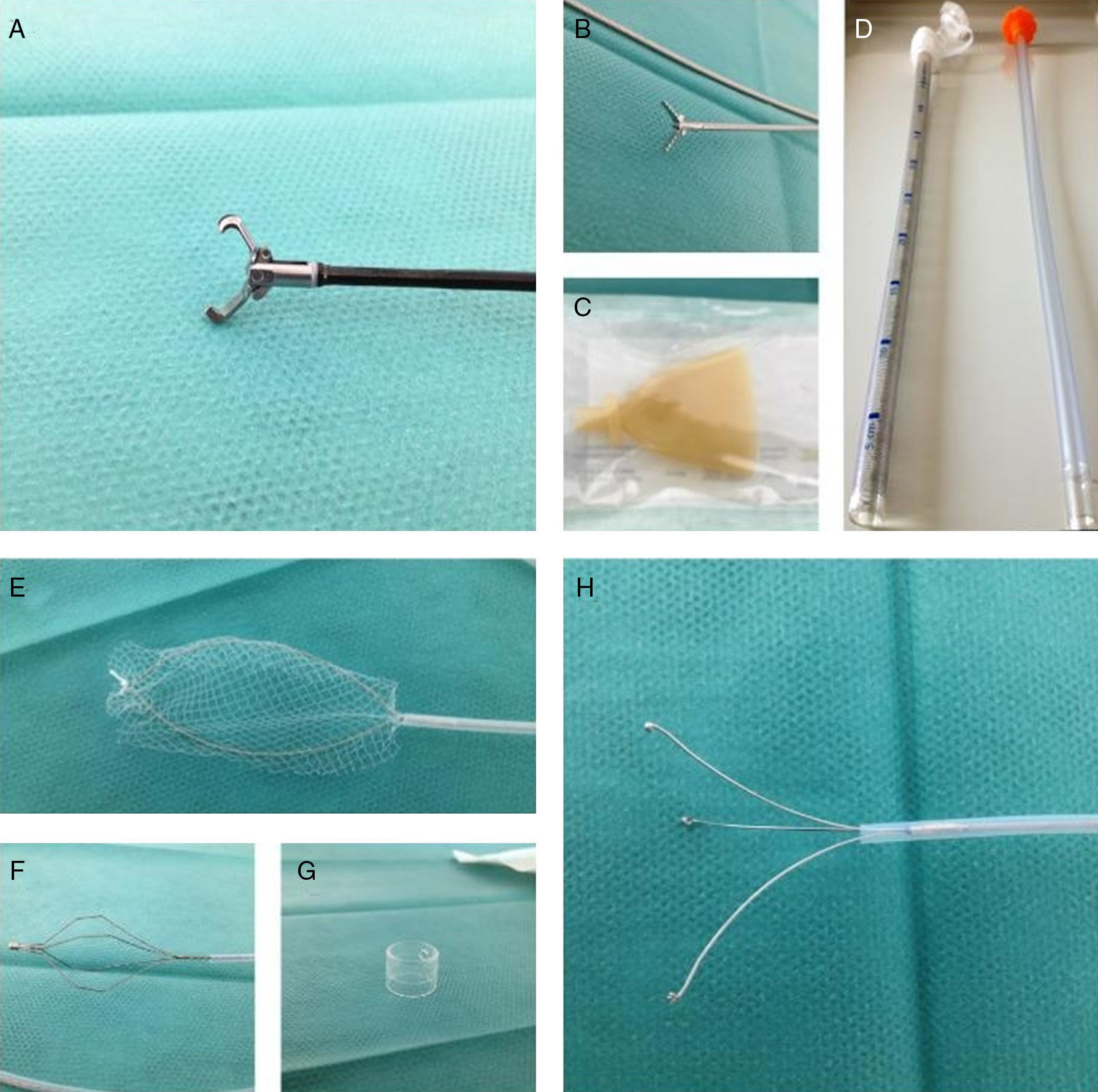
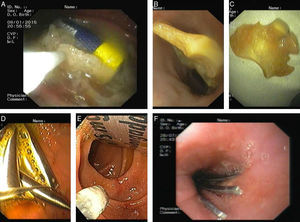
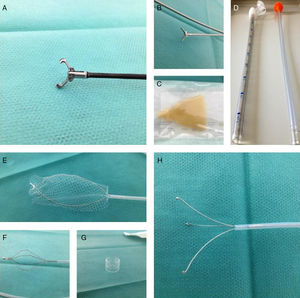
3.2Endoscopes and ancillary equipmentFlexible endoscopes are the preferred endoscope type because of the high success rate, low complications associated and patient comfort.1,56 Both flexible and rigid endoscopic approaches have high success rates (>90%), however, the later is associated with a considerably high perforation rate.56,57 In adults, standard flexible gastroscopes (9.8mm external diameter with 2.8mm diameter single channel) are widely accepted and efficacious. Flexible ultra-thin (nasoendoscopes, external diameter <6mm) endoscopes have been suggested as an alternative to standard flexible endoscopes, however they have no additional benefit and frequently fail to retrieve objects below the upper esophageal sphincter.58 Even though, in children with less than 1 year-old, this small caliber endoscopes should be preferred albeit limiting the choice of retrieval devices. Small sharp objects at the level of the hypopharynx can be removed by otorhinolaryngologists with a laryngoscope and the aid of a Kelly or McGill forceps. Several endoscopes, endoscopic retrieval devices and ancillary material are available to assist in the removal of FB and food bolus impactions (Fig. 5).59 As a general rule, some basic tools must be present in the endoscopic room, such as: rat-tooth or alligator forceps, triprong graspers, polypectomy snares, Dormia baskets and retrieval nets.23,59,60 The choice of the retrieval device is determined by the nature of the FB, instrument channel and endoscopist preference. Retrieval forceps (rat-tooth – Fig. 5A or alligator – Fig. 5B) can be useful for small hard objects (pins, needles or blades), retrieval graspers (Fig. 5H) are preferred for soft objects (food bolus), baskets (Fig. 5F) are useful for round objects, nets (Fig. 5E) and snares are used for smooth objects and food bolus. The first published case reporting the use of an overtube was performed in 1974 by Witzel et al.61 In the following years, a number of modifications were reported with the overtubes. Cotton described, in detail, the insertion technique, its general principles, design, indications and limitations.62 Depending on the location of the FB, standard-sized overtubes that extend past the upper esophageal sphincter (∼25cm) and overtubes of length 45–60cm (Fig. 5D) that extend past the lower esophageal sphincter should also be available.63,64 Advantages of this devices are: airway protection, allowance frequent passages of the endoscope and protection of the gastrointestinal mucosa from lacerations.65 In order to prevent mucosal injury and to protect the patients’ airway during removal of the FB through the pharynx, an overtube is recommended in the removal of the following FB: round objects >2.5cm, long objects >6cm, sharp objects and disk batteries.66 In case of food bolus impaction and bezoars, the use of an overtube should also be considered. A retractable latex-rubber condom-type hood (Fig. 5C; Kimberly-Clark, Roswell, GA, USA) is effective for delivering objects across the sphincter and for preventing mural injury from sharp or pointed edged objects.67 Transparent distal caps (Fig. 5G) can also be used to protect during the removal of small pointed objects.68 The usefulness of laser techniques (e.g., argon-plasma or Nd:YAG laser) for fragmentation of complex metallic FB has been described.69 Magnetic retrievers should not be used because FB are often lost during the procedure.59
4Specific scenarios4.1Food bolus impaction and bezoarsFood bolus ingestion represents the most common cause of unintentional esophageal impaction in adults (Fig. 2).3 In the vast majority of the episodes there is an underlying esophageal pathology directly prompting the impaction (75–100%).2,70 The main predisposing causes are Schatzki rings, peptic strictures and eosinophilic esophagitis (10%).8,10 Other causes, as extrinsic compression, surgical anastomoses, fundoplication wraps or esophageal cancer are less commonly found. Notwithstanding, motility disorders as a culprit are infrequent.71 In the Western World meat is the most frequent cause of impaction (two-thirds of the cases, Fig. 2A and D),42 while in Asia, fish and fish bones (Fig. 2B and E) dominate.2,70 The majority of food bolus impaction may resolve spontaneously, without intervention.55 Complications rarely occur, but are more common if there is a pre-existing esophageal disorder. Also, in esophageal food bolus impaction, the risk of complications increases proportionally to the impaction duration.23 For symptomatic patients, flexible endoscopy is the best diagnostic and therapeutic method.21,60 The endoscopy timing can be defined by the severity of symptoms.72 However, all patients with impaction symptoms should be assessed and treated with endoscopy within 12–24h after presentation.73 The food impact can be removed using two different approaches. The push method is the preferred treatment modality, achieving 90% success rates, with minimal complications.74 The endoscope should pass around the food without difficult. Then, the bolus can be pushed into the stomach using the endoscope.7 If this technique is not possible, the bolus must be dislodged and withdrawn en bloc or by piecemeal approach by using a grasping device and preferably an overtube.2,21 After resolution of the impaction, biopsies of the underlying pathology can be done if appropriate. In cases of esophageal rings or stricture, it is considered safe to perform dilation during the same session, if there is no significant mucosal damage, in order to reduce the risk of recurrence.2,8 Bezoars are defined by organic material compacted and retained, usually in the upper gastrointestinal tract. Some predisposing disorders have been described.75 Bezoars can be categorized by their contents in vegetable fiber (phytobezoar), milk (lactobezoar) or hair (trichobezoar). The most frequent location is the stomach. Endoscopic resolution with the use of retrieval forceps or snares combined with an overtube can be useful. However, in some larger bezoars, surgery may be warranted.76
4.2Sharp and pointed objectsAlthough the majority of the sharp and pointed FB will pass spontaneously through the gastrointestinal tract, perforation may occur in up to 15–35% of the patients.77 Toothpicks and animal (namely chicken and fish) bones are the most likely objects to cause perforation.78,79 When there is a suspicion of a swallowed sharp-pointed object, the patient must be evaluated to define its location. Even after a radiological examination with negative findings, endoscopy must be performed.23 The esophagus is a frequent site of blockage and FB impacted in the esophagus are at a particularly high risk of complications. This risk is 25% higher in the upper esophagus than in other locations.60 Moreover, the vicinity of vital organs makes complications potentially life-threating.80 Therefore, sharp-pointed objects lodged in esophagus represent a medical emergency.23,81 For the retrieval of FB located at or above the cricopharyngeus, direct laryngoscopy is an option. If this method is not successful or if the objects are lodged below the cricopharyngeus, rigid or flexible endoscopy may be performed. Although the majority of objects that reach the stomach will pass without consequences, due to a significant risk of complications that can be as high as 35%, they ought to be endoscopically retrieved if it can be safely performed.23 Otherwise, daily radiographs should be done in order to document their safe passage. Instructions to promptly report abdominal pain, fever, vomiting and gastrointestinal bleeding must be given to all patients.23 For this type of FB, several grasping tools can be used, namely retrieval forceps, retrieval nets and polypectomy snares.82 The use of a protective device such as a cap, an overtube or a protector hood may reduce the risk of mucosal injury. This risk should also be minimized by a careful manipulation and orientation of the object.60
4.3Long or bulky objectsLong or bulky objects are considered those larger than 2.5cm and longer than 5–6cm (Fig. 3).23,34,60 This kind of objects (e.g., toothbrushes or cutlery – Fig. 3F) require endoscopic or surgical intervention and should be removed before passing to the duodenum in order to minimize the risk of perforation.23,60 One study showed that, at the time of the endoscopy, 80% of the aforementioned objects were located in the stomach. Additionally, the risk of perforation reached 15–35% when the pylorus was passed.13 In addition to the consensual emergent endoscopic approach in case of an esophageal obstruction (Fig. 4) or the surgical approach in case of a perforation, if an object longer than 6cm is at or distal to the proximal duodenum and if there is no clinical or radiological evidence of perforation, an urgent endoscopy should be performed. In the considered situation, an overtube (>45cm) and other ancillary material (e.g., retrieval net, polypectomy snare, Dormia basket) can be trustworthy to successfully retrieve the object.23,60
4.4Coins, magnets and batteriesCoins are the most frequently ingested FB in the Western countries, particularly in children (accounting for up to 88% of the ingested FB).60 Coins in the esophagus that are not promptly removed can result in pressure necrosis of the esophageal wall with possible perforation and fistulization.55 They should be differentiated from batteries on radiographs (coins have a smooth and irregular border and batteries show two concentric circles).60 In adults, small coins usually pass through the esophagus and do not need to be retrieved, but larger coins may become lodged.55 The upper esophagus is the main site of impaction. Coins in the distal esophagus are more likely to pass spontaneously than those in the proximal esophagus (56% vs. 27%, respectively).83 If a coin becomes lodged within the esophagus and the patient is asymptomatic, a short period of observation of 12–24h may be acceptable to see if it passes spontaneously into the stomach (Fig. 4). Patients with marked symptoms, such as drooling, chest pain and stridor should have emergent endoscopic intervention to remove the coin. Most coins will eventually leave the stomach and pass through the gastrointestinal tract without obstruction.23 Coins should be removed when blocked in the esophagus and when larger than 25mm or retained for more than 3 weeks in the stomach.60 Retrieval nets is the preferred retrieval device to remove coins, as it allows easy snaring of the coin and also protects the airway as the coin is pulled past the larynx.55 The rat-tooth and grasping forceps (triprong) are ample enough to grasp coins in most cases. In this case, an overtube can be used for airway protection if the coin can be pulled through it.60
Ingested magnets can cause severe gastrointestinal injury and death. The attractive force between two or more magnets or an ingested metal may lead to pressure wall necrosis with possible perforation and fistulization, volvulus or bowel occlusion.23 Biplane radiographs are important to check how many magnets have been ingested and if any other metallic FB is present, which could be hidden behind the magnet(s) in a plain radiograph.60 Therefore, an urgent endoscopy should be performed to remove the magnet before it becomes out of endoscopic reach (Fig. 4). Endoscopic removal of magnets can be performed with rat-tooth forceps, retrieval nets or baskets. If multiple magnets have been ingested a post-procedure radiograph should be performed to ensure that all magnets have been retrieved.55
Children are the most likely to ingest a battery, particularly a disk or button battery.23 Due to corrosive action, low-voltage burns and pressure necrosis, disk batteries can rapidly cause wall necrosis of the esophagus with possible perforation and fistulization.60 Ingestions of cylindrical batteries are rare and nonsevere in most cases with no reports of major life-threatening injuries.55 After radiographic documentation, batteries lodged in the esophagus should be emergently removed by endoscopy, within 12h.23 A retrieval net or basket can be used for button batteries, whereas for cylindrical batteries the use of a polypectomy snare is more adequate (Fig. 3A).60 If the battery cannot be retrieved from the esophagus, it should be pushed into the stomach and retrieved. However, once in the stomach most disk batteries pass without complications. Generally, batteries retained in the stomach do not need to be retrieved. Exceptions are: symptomatic patients, in case of a cylindrical battery retained in the stomach for more than 48h or unless it is a disk battery larger than 20mm and retained in the stomach for more than 48h.23
4.5Narcotic packetsIllicit drugs may be smuggled by swallowing rubber or latex packets, containing most commonly cocaine or heroin. The two larger published case-series showed that most of these body packers, if asymptomatic, can be managed conservatively and discharged after a few days. However, in some cases they might present symptomatic and even severely ill, with the need of intensive care management.84,85 If an obstruction develops, they can present vomiting and abdominal pain. If the packets are ruptured, drug-related symptoms might occur, such as agitation, sweating, dilated pupils, hyperthermia, tachycardia, hypertension and in more severe cases with seizures, status epilepticus, myocardial infarction and ventricular fibrillation (cocaine symptoms) or reduced level of consciousness, respiratory depression, pinpoint pupils and decreased bowel sounds (heroin symptoms).86 Diagnosing and detecting drug packets might not be straightforward owing to the fact that most of these patients will not reveal that they have ingested drug packets due to legal issues. Plain abdominal radiographs can detect drug packets as oval or round soft tissue densities highlighted by a gas halo. Its estimated sensitivity is 85–90%.87 Although false-negative CT scans have been reported, it is a valuable exam in the diagnosis of the most challenging cases. Liquid cocaine (and possibly the liquid forms of other drugs) is more difficult to detect by radiographs due to its aqueous base and therefore radiographic appearance similar to tissues.88 Endoscopic retrieval of these packets is contraindicated for fear of rupture and drug overdose. In order to hasten drug removal, the use of bowel purgatives (namely polyethylene glycol, at a rate of 2L per hour) has been safely used in body packers.89,90 Furthermore, some studies suggest the use of prokynetics (erythromycin, 500mg intravenously or metoclopramide, 10mg intravenously).91 Surgery is indicated for failure of the packets to progress, signs of intestinal obstruction or clinical findings suggestive of rupture.34
5ConclusionIngestion of true FB and food bolus impactions are common. The clinical approach depends on the type of ingested FB (size, shape and chemical composition), patients’ symptoms and clinical findings. In the majority of the FB ingestions, the objects will pass spontaneously throughout the gastrointestinal tract uneventfully, however, endoscopic intervention will be required in 20% of the cases, and a surgical intervention in less than 1%. Emergent endoscopic intervention (within 12h) is warranted for patients presenting with symptoms compatible with a complete esophageal obstruction, sharp-pointed objects and disk batteries in the esophagus.
Author contributionsAll authors contributed equally to the literature research, study design, data collection, data analysis, data interpretation and writing.
FundingNo grant or financial support has been received.
Conflicts of interestThe authors have no conflicts of interest to declare.