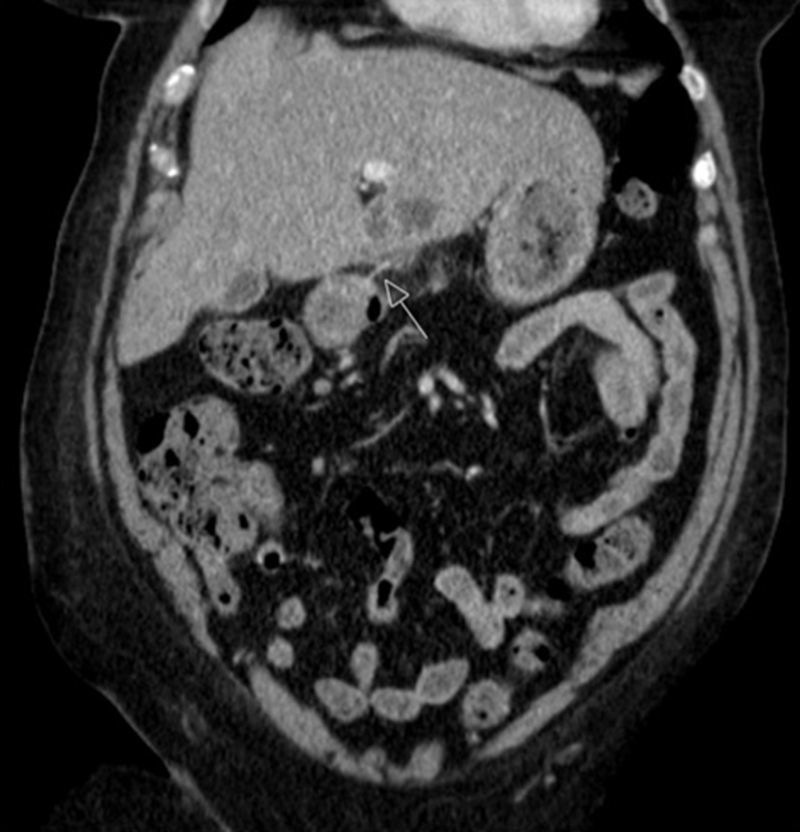
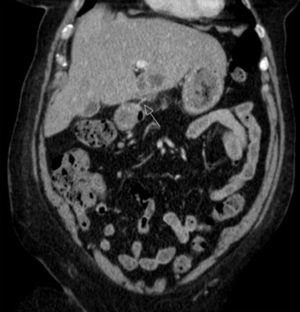
The authors present the case of a 80 years-old woman, with no relevant medical history, which presented to the emergency department for fever (38–39°C), chills, nausea and vomiting, and persistent pain in the right hypochondrium lasting for two days. Initial clinical assessment revealed hypotension, hypoxemia (pO2<70mmHg), slight leukocytosis, CRP 176mg/L and increased lactates (3.0mmol). Imaging studies (chest X-ray and ultrasonography) showed no change. The patient was hospitalized in an intermediate care unit where she was started on antibiotics with a diagnosis of sepsis of unknown origin. Two days after, the patient was clinically better, with improvement of the inflammatory parameters, but maintained abdominal complaints and so it was performed an abdominal CT scan where we were able to identify a linear foreign body with approximately 30mm perforating the intestinal wall at the level of the pylorus, contacting with the hepatic parenchyma where a multiloculated abscess with 44mm was seen (Fig. 1 [arrow]). After additional conversation with the patient, it was found to be of a fishbone ingested days before. Consequently, an upper endoscopy was performed where it was found a swollen area in the antero-superior duodenal bulb wall with a central fistulous opening (Fig. 2). After discussion with the surgical team it was decided to maintain a conservative strategy (antibiotics plus imaging surveillance). Once there was gradual improvement of the clinical picture, the patient was transferred to the surgery ward and then discharged to outpatient consultation. During the following six months the patient made regular visits, remaining asymptomatic and with imaging resolution of the abscess.
A myriad of ingested sharp-pointed objects have been described. The ones most commonly associated with complications are chicken and fish bones. Patients suspected of swallowing sharp-pointed objects must be evaluated to define the location of the object. However, not always the patients are aware of foreign body ingestion, and in these cases the diagnosis is only made on the occurrence of complications, such as in the reported case. Cases of hepatic abscess due to fish bone penetration are rare and may be fatal.1 Until today, less than 12 cases have been described in the literature. The possible mechanism of the liver abscess secondary to fish bone migration from the duodenum it's the creation of a duodenohepatic fistula covered by duodenal serosa.2 Since the first reported case, treatments usually include drainage of the abscess, removal of the foreign body, and administration of appropriate antibiotics.3 Surviving patients described in previous reports were all surgically treated, except for one case.4 If there is a strong suspicion of bowel perforation by a foreign body or if a foreign body is detected preoperatively, surgery is considered the treatment of choice in current clinical practice, but when the diagnosis is not initially suspected, and if the patient shows a clinically improvement, a conservative approach can be attempted. In our case, once the patient was better under empirical antibiotics it was preferred not to submit the patient to a surgical procedure. Although controversial, the decision turned out to be favorable for the patient as she fully recovered, allowing an outpatient follow-up and six months after discharge she was asymptomatic and the infection fully resolved. So we suggest that medical approaches could be attempted first in such cases. Once the patient experiences signs of clinical deterioration surgical intervention should be promptly considered.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.