Diuretics have been used for decades in the treatment of hypertension. Its efficacy has been demonstrated in numerous clinical trials. It is well known that the reduction in cardiovascular risk is a consequence of the reduction in blood pressure levels regardless of the drug used, but thiazide diuretics continue to be first-line drugs, especially in low doses and combined with other drugs. The debate on the advantages of using chlorthalidone or hydrochlorothiazide continues, however hydrochlorothiazide is drug most used and for which there is greater availability. The association with potassium-sparing diuretics increases the effectiveness and reduces the adverse reactions of thiazides. A new group of drugs, close to potassium-sparing diuretics, that antagonise aldosterone synthase are showing promising results as antihypertensives. There are no significant differences between men and women regarding the antihypertensive effect of thiazide diuretics.
Los diuréticos son desde hace décadas utilizados en el tratamiento de la hipertensión arterial. Su eficacia ha sido demostrada en numerosos ensayos cínicos. Aunque se acepta que la disminución del riesgo cardiovascular es consecuencia de la reducción de las cifras de presión, con independencia del fármaco usado, los diuréticos tiazídicos siguen siendo fármacos de primera línea, sobre todo en dosis bajas y combinados con otros fármacos. Continúa abierto el debate sobre las ventajas de utilizar clortalidona o hidroclorotiazida, pero esta sigue siendo la más utilizada y para la que existe mayor disponibilidad. La asociación con diuréticos ahorradores de potasio aumenta la eficacia y disminuye las reacciones adversas de los tiazídicos. Un nuevo grupo de fármacos, próximos a los diuréticos ahorradores de potasio, que antagonizan la aldosterona sintasa están mostrando resultados prometedores como antihipertensivos. No hay diferencias significativas entre hombres y mujeres respecto al efecto antihipertensivo de los diuréticos tiazídicos.
Among the antihypertensive drugs available, diuretics are the oldest and the first to demonstrate efficacy with acceptable tolerability. Their introduction into therapeutics in the 1950s ushered in a major change in the treatment of arterial hypertension. A group of patients treated with diuretics was a constant feature of the first large-scale clinical trials conducted during the 1960s and 1970s, when antihypertensive therapeutics were being researched scientifically. In some of these studies, a diuretic was used as an add-on drug in the event that the drug initially used was not efficacious enough.
Diuretics comprise a heterogeneous group of drugs whose main effect is to increase urine output. Their general mechanism of action is to modify ion transport at different sites in the nephron and to stimulate renal excretion of water and electrolytes, primarily sodium and chloride. Diuretics are categorised according to their mechanism and site of action as carbonic anhydrase inhibitors, osmotic, thiazide, loop or high-ceiling, and potassium-sparing diuretics. The most commonly used antihypertensives are thiazides, which are sometimes combined with potassium-sparing diuretics. Loop diuretics are used only in selected circumstances.
There is a wealth of information available regarding the use of diuretics to treat high blood pressure. On 31 December 2023, the PubMed database contained 25,864 papers (diuretics AND hypertension), of which 3277 were randomised clinical trials; 338 were meta-analyses, and 250 were systematic reviews. In the last 5 years, the results of 174 randomised trials and 94 systematic reviews have been published, giving an idea of the interest in the subject.
According to the report by the Spanish Medicines Agency concerning the use of antihypertensive drugs in Spain published in 2021,1 diuretics accounted for 13.7% of antihypertensive drug prescriptions, while renin–angiotensin system inhibitors accounted for 61.6%. In 2010, the percentages were 16.4% and 58.8%, respectively. The decrease in the relative weight of diuretics is striking despite the fact that over the same period, antihypertensive prescriptions rose by 6.9%. The report does not discriminate between drugs used in monotherapy or in association and one cannot rule out the possibility that indications other than hypertension are included in the calculation.
We will review the main characteristics of thiazide diuretics, with special attention paid to the results of the latest published meta-analyses and to information that can enable the most suitable drug to be chosen. We will also discuss new developments in the aldosterone antagonist group of drugs.
Thiazide diureticsThiazide diuretics were the first well-tolerated, efficacious antihypertensive drugs to be introduced into therapy. For over half a century, they have been regarded as first-line treatment, both in monotherapy and in combination with other drugs. Similarly, they have been shown to reduce cardiovascular morbidity and mortality in numerous studies.
This class includes benzothiadiazine derivatives, hence the name, as well as those known as thiazide-like drugs with analogous pharmacological effects, albeit having a different chemical structure. All have the same mechanism of action and similar effects, although there are differences in their pharmacokinetic properties. The first to be introduced into therapeutics was chlorothiazide, followed by chlorthalidone, hydrochlorothiazide, indapamide, and xipamide. Hydrochlorothiazide, chlorthalidone, and indapamide are currently the most widely used and the advantages of each over the others have been the subject of debate for years.
Mechanism of actionDiuretics increase urine flow by boosting sodium excretion (natriuresis) and an accompanying anion, usually chloride. Continued diuretic administration leads to a net deficit in total body sodium, however the effect is time-limited due to renal compensatory mechanisms, such as activating the sympathetic nervous system and the renin–angiotensin–aldosterone system (RAAS), lowering blood pressure, renal epithelial cell hyperplasia, enhancing renal epithelial transporter expression, and, possibly, disturbances in natriuretic hormones such as atrial natriuretic peptide. Diuretics can modify how the kidney deals with other cations including potassium, protons, calcium, or magnesium, in addition to anions such as chloride, bicarbonate or phosphate, and uric acid. Furthermore, diuretics may indirectly alter renal haemodynamics.2
The exact mechanism by which thiazide diuretics lower blood pressure is not fully understood. They decrease extracellular volume by inhibiting a sodium–chloride cotransporter, encoded by the SLC12A3 gene, which is responsible for sodium reabsorption in the distal convoluted tubule; therefore, blocking it increases sodium excretion and decreases cardiac output. The effect on pressure is maintained by decreasing peripheral resistance, although cardiac output and extracellular volume return to pre-treatment values. Hydrochlorothiazide can open calcium-activated potassium channels, which results in hyperpolarisation of vascular smooth muscle cells and causes calcium channels to close, thereby decreasing calcium entry and hindering vasoconstriction. Hydrochlorothiazide also inhibits vascular carbonic anhydrase, which could modify smooth muscle cell pH and facilitate the mechanism described. These effects have been demonstrated extensively in vitro; however, their role in the antihypertensive response of thiazides remains speculative.2–4 There is no doubt that its main action is on the sodium–chloride cotransporter given that the antihypertensive effect of thiazides is less marked in patients with kidney failure. Moreover, people with functional mutations in the SLC12A3 gene have lower blood pressure than those without mutations.5
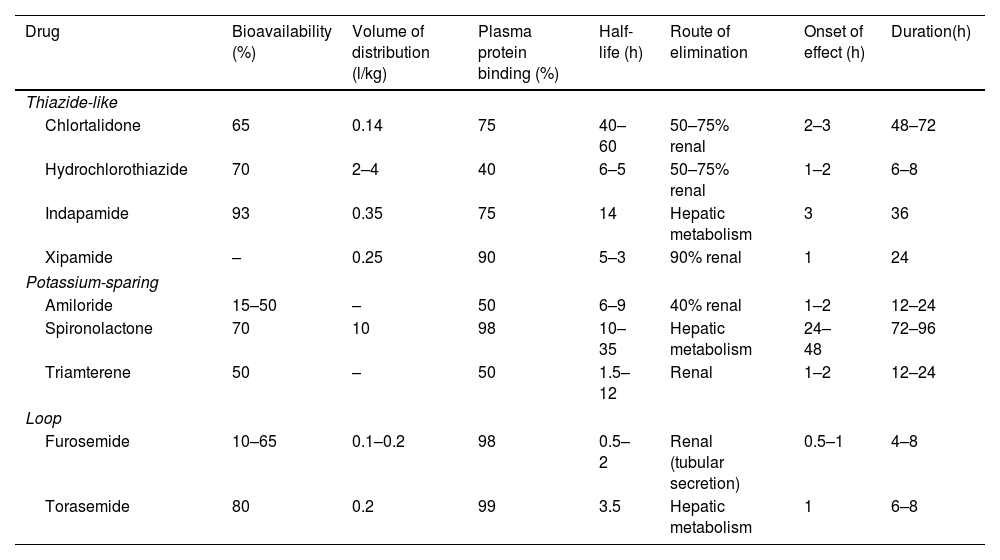
Pharmacokinetic propertiesThiazides are well absorbed orally, with greater absorption when taken with food; their bioavailability ranges from 65 to 95%, but may be lower in patients with heart failure. Hydrochlorothiazide and, to a greater extent, chlorthalidone bind to red blood cell carbonic anhydrase resulting in a circulating reservoir which may account for why the effect of chlorthalidone lasts longer. They are eliminated via active transport in the proximal tubule (a prerequisite for them to work) and compete with uric acid in this transport. Most of the drugs in this class are excreted unchanged, but indapamide undergoes intensive hepatic metabolism first.6
The effect typically begins 3h after administration and its duration is directly related to their plasma half-life. Thiazides cross the placenta and may result in decreased extracellular volume in the foetus; they should therefore not be used in pregnant women. They are also excreted in breast milk, however not in sufficient concentration to produce effects in the infant.2
Table 1 lists the pharmacokinetic characteristics of the most widely used thiazide diuretics in Spain.
Pharmacokinetic characteristics of diuretics.3,6,7
| Drug | Bioavailability (%) | Volume of distribution (l/kg) | Plasma protein binding (%) | Half-life (h) | Route of elimination | Onset of effect (h) | Duration(h) |
|---|---|---|---|---|---|---|---|
| Thiazide-like | |||||||
| Chlortalidone | 65 | 0.14 | 75 | 40–60 | 50–75% renal | 2–3 | 48–72 |
| Hydrochlorothiazide | 70 | 2–4 | 40 | 6–5 | 50–75% renal | 1–2 | 6–8 |
| Indapamide | 93 | 0.35 | 75 | 14 | Hepatic metabolism | 3 | 36 |
| Xipamide | – | 0.25 | 90 | 5–3 | 90% renal | 1 | 24 |
| Potassium-sparing | |||||||
| Amiloride | 15–50 | – | 50 | 6–9 | 40% renal | 1–2 | 12–24 |
| Spironolactone | 70 | 10 | 98 | 10–35 | Hepatic metabolism | 24–48 | 72–96 |
| Triamterene | 50 | – | 50 | 1.5–12 | Renal | 1–2 | 12–24 |
| Loop | |||||||
| Furosemide | 10–65 | 0.1–0.2 | 98 | 0.5–2 | Renal (tubular secretion) | 0.5–1 | 4–8 |
| Torasemide | 80 | 0.2 | 99 | 3.5 | Hepatic metabolism | 1 | 6–8 |
Some data are from the data sheets of the various drugs. Available at: https://cima.aemps.es/cima/publico/home.html (consulted on 14/03/2024). The patient's circumstances may alter bioavailability, as well as the percentage of renal elimination and, as a result, the onset and end of effect.
The dosage of hydrochlorothiazide used as an antihypertensive is 12.5–25mg/day. The antihypertensive effect appears after several weeks (between 4 and 6), even if there is no increase in diuresis; hence, the initial dose should not be modified before this period of time has elapsed. Doses of 6.25mg are not particularly effective in monotherapy, but are useful when administered together with other antihypertensives, given that diuretics have an additive effect with almost all groups. The association is especially beneficial in association with RAAS inhibitors, because both angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin II receptor antagonists (ARA-II) can lead to hyperkalaemia that offsets the hypokalaemia induced by the thiazides. Additionally, diuretics stimulate the RAAS, which enhances the effect of ACE inhibitors and ARA-II.7
As for thiazide-like diuretics, chlorthalidone is used at doses of 25–50mg/day which are similar to those of hydrochlorothiazide, although chlorthalidone is more potent and 1mg of this drug is more effective than 1mg of hydrochlorothiazide; indapamide is administered at doses of 2.5mg in the form of immediate-release tablets or 1.5mg in delayed-release formulation, and xipamide is prescribed at doses of 10–20mg/day. There are insufficient data to define equally effective doses of indapamide or xipamide with respect to hydrochlorothiazide.
Adverse reactions, drug interactions, and contraindicationsExcessive potassium excretion and, consequently, hypokalaemia, is the best-known adverse reaction of thiazides; is linked to their mechanism of action, and promotes the development of arrhythmias, most notably torsade de pointes and ventricular fibrillation, which can lead to sudden death. They occur more often at high doses.3,8
Most of the serious adverse effects caused by thiazides involve abnormalities in fluid and electrolyte balance and include extracellular volume depletion, hypotension, hypotension, hypokalaemia, hyponatremia, hypochloraemia, metabolic alkalosis, hypomagnesemia, hypercalcemia, and hyperuricemia.9 A recent study comparing thiazide-treated patients with those receiving other antihypertensives concludes that initiation of thiazide diuretic therapy can entail a risk of hyponatremia, which is greater among older individuals and those with comorbidities.10 They also decrease glucose tolerance. New diagnoses of diabetes have been reported to be more common among individuals treated with diuretics than among those treated with other drugs (53.5% vs. 30.6%).11 This may have a physiopathological explanation inasmuch as insulin secretion is potassium-dependent and diuretic-induced hypokalaemia could decrease the secretion of insulin and thereby foster hyperglycaemia. It is important to note that thiazide-induced diabetes mellitus is not associated with an increased risk of cardiovascular disease.12 Hypokalaemia can undermine the antihypertensive effect and cardiovascular protection in patients with hypertension. In addition, plasma levels of LDL-cholesterol, total cholesterol, and triglycerides may also increase.
Thiazide diuretics rarely cause central nervous system (e.g., vertigo, headache), gastrointestinal, hematologic, or dermatologic (e.g., photosensitivity and skin rashes) disorders. The incidence of erectile dysfunction is higher than with other antihypertensive agents.13
These diuretics may lessen the effects of anticoagulants, uricosurics, and insulin, and increase those of certain anaesthetics, diazoxide, digitalis, lithium, loop diuretics, and vitamin D. The effectiveness of thiazide diuretics may be decreased by the co-administration of non-steroidal anti-inflammatory drugs, both selective and non-selective COX-2 inhibitors, and bile acid sequestrants. Amphotericin B and corticosteroids increase the risk of hypokalaemia.2
There is a paucity of information concerning their use in the paediatrics population; however, they should be avoided when hypertension coexists with obesity due to possible adverse metabolic effects. Because of their chemical structure, they are contraindicated in people with hypersensitivity to sulphonamides.
Antihypertensive effectGiven alone, thiazide diuretics reduce blood pressure and, when combined with other antihypertensives, increase their effect. All diuretics have a very flat antihypertensive dose-response curve, so that increasing the dose does not lead to a proportional increase in effect on blood pressure. Nevertheless, there is a correlation between dose and the incidence of adverse reactions, which are more prevalent at higher doses. As a result, lower doses are currently being used, especially in combination, than those used in early studies.14
For years, the choice of drug to initiate antihypertensive treatment has been the subject of debate. The decision was challenging owing to the fact that the evidence available was scant because there were no head-to-head comparisons between the different types of drugs, which were developed over a period of more than 30 years. Thus, there were major differences in the number of patients treated and in how the trials were designed. A number of systematic reviews have been published that probe the efficacy of antihypertensive drugs, but most of the trials included in these reviews used stepwise treatment and combined different classes of drugs.15,16 Some have assessed efficacy against untreated patients, or effectiveness at specific ages.17,18 Overall, these reviews, as well as a new meta-analysis including more than 340,000 patients,19,20 have reached a consensus about the importance of normalising blood pressure. This is because in terms of reducing cardiovascular events, the benefit of treatment, regardless of other circumstances, has to do with the magnitude of blood pressure reduction and the different drugs have a similar effect in preventing cardiovascular mortality and morbidity. In addition, most hypertensive patients will require a combination of drugs to achieve adequate control. However, in the absence of sufficient data, we cannot rule out the possibility that some drugs have specific effects beyond that of blood pressure reduction that may affect the results. The pooled assessment of the different studies also reveals that the benefit is greater in older patients and those at higher cardiovascular risk, and that on average a decrease in systolic blood pressure by 5mm of mercury results in a 10% risk reduction.20
Thiazide diuretics and their analogues are the most widely studied group of antihypertensive drugs and have been compared with most other groups.21,22 In 2023, the results of a collaborative Cochrane systematic review23 were published regarding the role of thiazide diuretics versus other antihypertensive drugs. Twenty trials enrolling a total of 90,000 patients and 26 comparator groups treated with alpha- or beta-blockers, calcium antagonists, ACE inhibitors, ARBs, aliskiren, or clonidine were included. The key findings are that there is no difference between groups with respect to the effect on mortality, albeit diuretics may reduce cardiovascular events more than alpha-blockers, beta-blockers, and calcium antagonists, and they are likely to reduce cerebrovascular accidents more than ACE inhibitors. No conclusions could be drawn from the analysis concerning differences between diuretics and ARBs or renin inhibitors.
For years now, there has been ongoing discussion about the efficacy of hydrochlorothiazide and chlorthalidone in reducing major cardiovascular events, with some authors arguing that chlorthalidone or indapamide would be preferable to hydrochlorothiazide given that they have a longer duration of action.24 A meta-analysis25 was published in 2011 that aimed to determine whether the widespread use of hydrochlorothiazide as an antihypertensive was justified. Nineteen trials with ambulatory blood pressure monitoring were included and analysis found that the effect of the diuretic at doses of 12.5 or 25mg/day was very similar and inferior to that observed with any of the comparator drugs: beta-blockers, calcium channel blockers, ACE inhibitors, or ARBs. The 50mg dose achieved similar reductions in blood pressure as the other drugs. The study concluded that low-dose hydrochlorothiazide was unsuitable for first-line antihypertensive treatment and justified the preferential use of chlorthalidone based on the results of the study as well as those of a previous meta-analysis comparing the effect of both drugs.26 Another meta-analysis27 was published in 2012 that compared the effect of hydrochlorothiazide, chlorthalidone, and bendroflumethiazide. An order of potency of bendroflumethiazide>chlorthalidone>hydrochlorothiazide was established for systolic and diastolic pressure reduction, correlating with the affinity of each drug for the sodium–chloride cotransporter in the distal convoluted tubule. Doses that produced identical effects were 25mg hydrochlorothiazide, 8mg chlorthalidone and 1.5mg bendroflumethiazide. Other meta-analyses also provide evidence of chlorthalidone being more efficacious.28,29
Despite all the available information pointing to the apparent superiority of chlorthalidone, the differences in the design of the trials analysed left the question open and the definitive answer would have to come from the results of an ad hoc clinical trial. The outcomes of just such a study were published in late 2022 when the results of a pragmatic, open-label trial comparing the efficacy of chlorthalidone and hydrochlorothiazide in reducing cardiovascular events in hypertensive patients came out. The trial had a composite primary endpoint of non-fatal myocardial infarction, stroke, hospitalisation for heart failure, urgent coronary revascularisation for unstable angina, and non-cancer death.30 The total study population included 13,523 hypertensive subjects (mean age 72.5 years) treated with hydrochlorothiazide at a dose of 25 or 50mg daily and who were randomised to continue hydrochlorothiazide or switch to chlorthalidone (12.5 or 25mg daily). Baseline systolic blood pressure was 139mmHg in both groups and remained essentially unchanged throughout the study. After 2.4 years of follow-up, there was no intergroup difference in the incidence of events. This was the first clinical trial specifically designed to compare both drugs and the results fail to demonstrate any difference between both drugs in reducing cardiovascular events. The design and interpretation of the results of this study have been criticised,31,32 leaving the question unanswered, and the fact is that hydrochlorothiazide prescription far exceeds that of thiazide-type diuretics. In Spain, there are 13 drugs with hydrochlorothiazide as the active ingredient and more than 500 with hydrochlorothiazide combined with other antihypertensive agents, many of them in triple combinations, whereas there is only one with chlorthalidone and three with chlorthalidone combined with atenolol or spironolactone. Ten years ago, there were six combinations.
What do clinical guidelines say?Numerous guidelines on the diagnosis and treatment of hypertension have been instrumental to improving the management of hypertensive patients worldwide. Although they concur on the essentials, they differ on issues such as classification, the values at which to initiate drug treatment, and the selection of starting drugs.33,34 The possibility has been raised that hypertension may be overdiagnosed and overtreated in some settings, or the reverse, depending on the knowledge of health professionals and the health care system. To avoid such disparities, the need for a single, independent, international guideline has been postulated,35 although some authors consider this proposal unfeasible and unnecessary.36
The Spanish guideline updated in 202237 and the European guideline of 202338 argue that the debate surrounding the first choice of drug has become less heated because there is no doubt that the benefit of treatment is due to the reduction in blood pressure and not to the properties of the drugs themselves39; moreover, most hypertensive individuals require a combination of drugs to initiate treatment in order to control their blood pressure. The guidelines coincide on the existence of five types of drugs: ACE inhibitors, ARBs, beta-blockers, calcium antagonists, and diuretics. Likewise, they all recommend the preferential use of thiazide and thiazide-like drugs, whether in monotherapy or in combination.
Other diureticsLoop diureticsHigh-ceiling or loop diuretics such as furosemide, bumetanide, or torasemide are not first-line antihypertensives. They increase diuresis by inhibiting a sodium–potassium–chloride cotransporter located in the thick segment of the ascending limb of the loop of Henle, hence their name.
They are authorised for use as monotherapy at low doses in essential hypertension, but are most commonly used in hypertensive patients with renal clearance of less than 30ml/min/1.73m2, in whom thiazides are ineffective. They are also indicated for individuals with comorbidities, such as nephrotic syndrome or congestive heart failure, and, in general, in situations in which sodium retention and oedema are present. In hypertensive emergencies they can be administered parenterally.37,38
From a pharmacokinetic point of view, the main characteristics of this class of drugs are their short half-life, longer for torasemide, and their high capacity to bind to plasma proteins so that glomerular filtration is minimal. They are excreted by tubular secretion, hence their efficacy in patients with a low glomerular filtration rate (Table 1). The most commonly used is furosemide, although when administered orally, its absorption is erratic and its bioavailability is extremely variable; torasemide has greater bioavailability and its effect tends to be more predictable.2,3 The efficacy of furosemide and torasemide in reducing blood pressure or cardiovascular morbidity is similar; nevertheless, according to the results of a recent meta-analysis of almost 12,000 patients with heart failure, torasemide prevents more hospitalisations than furosemide, although there is no difference in mortality.40
The most common adverse effects are hyponatraemia with volume depletion and hypokalaemia. Less commonly, they can increase urinary elimination of calcium and magnesium, thereby contributing to the development of arrhythmias.
Potassium-sparing diureticsPotassium-sparing diuretics can be divided into two groups according to their mechanism of action: the so-called adolsterone antagonists that block the mineral-corticoid receptor of the distal tubule and those that inhibit the epithelial sodium channel. They are weak diuretics, but they boost the antihypertensive effect of diuretics that act on the proximal tubule.2 Their main pharmacokinetics are reflected in Table 1.
Mineral-corticoid receptor antagonists, such as spironolactone or eplerenone, have a slow-onset yet persistent diuretic and antihypertensive effect and, in combination with calcium antagonists and RAAS inhibitors, play an important role in the treatment of patients with refractory hypertension.41,42 Their most common adverse effect is hyperkalaemia, in particular in patients with chronic kidney disease; in addition, spironolactone can cause menstrual disturbances, erectile dysfunction, gynaecomastia, or benign prostatic hyperplasia, calling for careful use, especially in men. Eplerenone has fewer adverse effects, but is also less potent. Most effects are related to the steroidal chemical structure of these compounds, although finerenone, which has a non-steroidal structure, works by antagonising the receptor, but has little antihypertensive activity.
Amiloride and triamterene, which inhibit the epithelial sodium channel of the distal tubule, are ineffective as antihypertensives in monotherapy, but highly beneficial in preventing potassium loss when combined with thiazides. In fact, the combination of amiloride plus hydrochlorothiazide is regarded as a monodrug and was the diuretic used in the control group of the INSIGHT trial,43 which examined the effects of the calcium antagonist nifedipine in a controlled-release formulation. In Spain, triamterene is only marketed in combination with furosemide.
A recent network meta-analysis44 of 276 randomised, double-blind trials published between 1964 and 2016, of which 39 included any group treated with potassium-sparing diuretics (23 amiloride, 13 triamterene, 3 spironolactone), with 58,807 participants (mean age 55 years; 45% female; mean follow-up 10 weeks), has demonstrated that the effect of thiazides on blood pressure is dose-dependent and that it is greater when associated with potassium-sparing diuretics than when administered alone. The association minimises thiazide-induced hypokalaemia and hyperglycaemia but does not modify the effects of thiazides on lipids.
Aldosterone synthase inhibitorsAlthough not potassium-sparing diuretics in the strict sense of the word, it seems worthwhile to comment on the first clinical results obtained with drugs with a new mechanism of action – the selective inhibition of aldosterone synthase, an enzyme responsible for catalysing the final steps of aldosterone synthesis, the inhibition of which leads to decreased aldosterone and increased plasma renin and potassium, without altering cortisol levels. In 2023,45 the results of a phase II trial with baxdrostat, the first of such inhibitors, were published. A total of 274 patients with refractory hypertension treated with three drugs, one of which was a diuretic, received 0.5, 1, or 2mg baxdrostat or placebo for 12 weeks. The patients exhibited a dose-dependent decrease in blood pressure and the difference of those treated with 1 and 2mg compared to those treated with placebo were statistically significant. The incidence of adverse effects was not particularly high, except for some patients who experienced hyperkalaemia, although treatment did not have to be discontinued. Preliminary results have also been published46 for lorundrostat, another selective aldosterone synthase antagonist, which at doses of 50 and 100mg for eight weeks yielded a significantly greater decrease in blood pressure than placebo in individuals with uncontrolled hypertension previously receiving two or three drugs. As in the previous case, the most important adverse effect was elevated plasma potassium. Further studies are necessary, but there is no doubt that this mechanism of action opens up new possibilities in the treatment of both refractory and obesity-related hypertension, which is highly dependent on aldosterone.
Sex-related differences in the hypertensive responseHypertension affects both men and women, but until recent years there has been no differentiated information on the clinical characteristics and effects of antihypertensive drugs in either sex. A study published in 200847 reviewed 31 randomised clinical trials of antihypertensive drugs involving 103,268 males and 87,349 females and concluded that the effect was comparable both in terms of lowering blood pressure and cardiovascular events; the study did not analyse possible differences for the different drug classes.
As far as diuretics are concerned, it must be noted that many of the clinical trials are old and were conducted at a time when few women were included, especially women of childbearing age. As a result, information concerning differences between men and women is scant. Adverse effects of thiazides, especially on electrolytes, have been reported to be more common in women, while those of aldosterone antagonists are more common in men. There are also data suggesting that control is more often achieved in men. There are some analyses for newer pharmacological groups that, on the whole, have found no notable differences. A position paper on the difference in hypertension as a function of sex has recently been published, sponsored by several European scientific societies,48 but specifically designed studies are needed to address the distinctive features of women and men from a physiopathological, clinical, and therapeutic point of view.
ConclusionsThe advantages of treating hypertensive patients with drugs when lifestyle modification alone is not enough is unanimously accepted and for more than 70 years, thiazide diuretics have proven their antihypertensive effectiveness and their ability to reduce the incidence of major cardiovascular events. Most hypertensive individuals require more than one drug to control their blood pressure and diuretics are at the forefront of these drug combinations and often as initial treatment. Questions as to which diuretic to choose and at what dose have been answered by the scientific evidence for decades. The most widely used and best studied thiazide diuretic is hydrochlorothiazide at doses ranging from 12.5 to 25mg/day, although in circumstances such as refractory hypertension, 50mg/day can be used.
Nonetheless, the debate regarding the potential benefits of using thiazide-like diuretics, especially chlorthalidone, remains unresolved. Numerous studies support the possibility that it may be more effective than hydrochlorothiazide, but a pragmatic clinical trial designed to answer the question has demonstrated that there is no difference, albeit both the design and interpretation of results have been criticised. On the other hand, there is evidence that association with potassium-sparing diuretics improves efficacy and reduces the adverse reactions to thiazides.
Beyond speculation or debate about the choice of drugs or the place of diuretics in treatment, the evidence is that what is important in order to reduce cardiovascular risk is that blood pressure be lowered. To this end, more than one drug is often needed, and thiazide diuretics or similar drugs should be included in the treatment of most hypertensive individuals.
Conflict of interestsThe author has no conflict of interests to declare with respect to the present article.