The great difficulty in implementing problem-based learning (PBL) in the Universidad Austral Medical School, Chile, was due to inadequate number of teachers wishing to become tutors in this topic. As a result of this, a PBL Peer-Tutoring Program was developed.
ObjectiveTo analyze, the peer-tutors’ experience in this program between 2007 and 2014.
MethodA qualitative, descriptive and exploratory was conducted using an intrinsic case study of the experience of peer-tutor. The techniques and tools used were a questionnaire with its survey and two focus groups with the same thematic script. A Likert scale was used to assess tutor perceptions on the training received. Performance and personal achievements was used in the survey, and a thematic analysis was carried out on all the notes from the focus groups.
ResultsA total of 95 students were trained as peer-tutor between 2007 and 2014, of which 85 of them (89.5%) responded to the questionnaire. The results showed that 84.7% of the tutors agreed on the training received, and 84.4% showed total agreement with their performance perception. The personal achievement item showed the highest responses (89.9%) for total agreement. The focus group highlighted that being a tutor is a great contribution to their personal and professional development.
ConclusionsPeer-tutoring in PBL promotes the early acquisition and practice of the skills described in the admission profiles of the medical student, using their own self-learning skills, effective communication, and the motivation to teach.
La gran dificultad para implementar el ABP en la Escuela de Medicina de la Universidad Austral de Chile, fue el número insuficiente de profesores dispuestos a ser tutores de ABP. Para subsanar lo anterior, se diseñó un programa por tutorías de pares usando estudiantes de cursos superiores para aplicar la metodología de ABP.
ObjetivoAnalizar la experiencia de los tutores por pares en este programa, entre los años 2007 y 2014.
MétodoEstudio cualitativo, descriptivo y exploratorio. Corresponde a un estudio de caso intrínseco de las experiencias de tutores por pares. Las técnicas e instrumentos utilizados fueron un cuestionario con su encuesta y dos grupos focales con el mismo guion temático. Para la encuesta, se utilizó una escala Likert para evaluar las percepciones de los tutores respecto de la formación recibida, sus logros personales y su desempeño. En los grupos focales se realizó un análisis temático de los registros escritos obtenidos por los moderadores.
ResultadosNoventa y cinco estudiantes fueron entrenados como tutores por pares entre los años 2007 y 2014, de los cuales un 89.5% respondió la encuesta. Los resultados mostraron que el 84.7% de los tutores estuvo de acuerdo con la capacitación recibida y el 84.4% se mostró totalmente de acuerdo con la percepción de su desempeño. El ítem logro personal mostró las mayores respuestas (89.9%) para el ítem «acuerdo total». Las sesiones de grupo focal mostraron que ser un tutor es un gran aporte al desarrollo personal y profesional de los estudiantes.
ConclusionesLa tutoría por pares en ABP promueve en los tutores, la adquisición y práctica temprana de las competencias descritas en el perfil de egreso del estudiante de medicina, utilizar sus propias habilidades de auto-aprendizaje, la comunicación efectiva y la motivación para enseñar.
Under the scope of the Society of Knowledge in the XXI century, professional trainings started to incorporate concepts such as “student-centered education,” “skills-based training” and “student mobility”, as well as the quality assurance and accreditation of universities.1,2 In line with the above and in the field of higher education, Chile focuses its efforts to provide the necessary skills to increase global competitiveness. With the establishment of the Quality Assurance System in Higher Education, a new era started where the educational efforts are oriented toward the quality of education and to the student-centered education approach. Thus, Universidad Austral of Chile (UACh) aligns with it by understanding learning as a holistic, permanent, creative and innovative process thus, encouraging teaching and professional development to be centered on quality, pertinence and equity. Education should facilitate people “to learn how to learn”, including the capacity to continue learning throughout life; “to learn how to do”, acquiring the necessary skills to perform in different situations; “to learn how to live together” respecting pluralism, mutual understanding and “to learn how to be”, so as to better develop their own personality in order to act with increasing autonomy, judgment and personal responsibility.
Aligned with the above, the School of Medicine from UACh, proposed a curriculum change in 2004. The new curriculum was meant to be innovative, to develop and consolidate essential generic and transferable skills for the XXI century medical professionals, to achieve a real coherence between the graduated professional and the one the country needs thus, leaving a rigid curriculum for an open and flexible one to train participative and integrated professionals for inter- and transdisciplinary team work, with a leading attitude to solve the people's health needs at individual, family and community levels.3
Consequently, one of the student-centered approached proposed, was the Problem Based Learning (PBL) methodology starting from the first year of medical studies. This was considered a good educational strategy because it can be used as a general strategy throughout the curriculum of a professional career or to be implemented as a working strategy along a specific course and even as a teaching technique applied for the review of certain course's learning objectives.4 It allows both the knowledge acquisition and the development of skills and attitudes.5 During the students’ interaction process, learning about a particular subject and the ability to make a diagnosis of their own learning needs is achieved, as well as the understanding of the importance of working collaboratively, to develop skills for the analysis and synthesis of information, as well as the commitment to their own learning process.6 Working in small groups is a pillar of the student-centered education promoting key skills for future career development, such as “learning how to learn”, teamwork, the use of knowledge in the context of the profession, etc., in addition to the specific competencies of the courses incorporated in the program.6
PBL promotes the student to understand and to have a proper in depth approach of the answers to the problems used for learning, by addressing philosophical, historical and practical issues by using a comprehensive approach and where the structure and the problem solving process are always open, encouraging a conscious learning and a systematic group work in a collaborative learning experience.7
Our first attempt to introduce PBL was in 2005 and 2006 whilst planning the curricula innovation and with the help of some teachers as tutors. Initially, this experience was quite encouraging and involved a small number of students; however the only drawback to start with PBL massively, was the insufficient number of teachers willing to work as PBL-tutors. Consequently, implementing PBL using peer-tutoring appeared as a viable solution. Our choice was to invite senior medical students with previous PBL experience to get trained as peer-tutors. It was in 2007, when the Medical School's Curricula Committee proposed the creation of a training program for PBL peer-tutors, asking to the Health Sciences Education Office to design, to carry out and to permanently monitor the program. Then, 10–12 students from third and fourth year were selected each year based on academic merits, to be trained as PBL peer-tutors. The training workshop was focused on how to manage a peer-tutoring session. Future peer-tutors were provided with theoretical and practical tools to know how to handle, guide, motivate and to evaluate a group of students during their process of self-learning in PBL. Each peer-tutor received a small monetary stimulus for his/her work and also assistantship hours’ credits for his/her academic records, at the end of the semester. The tutors remained for 2–3 years in the program before starting their clinical training.
The aim of this study was to analyze, the peer-tutors’ experience in this program, between 2007 and 2014.
MethodThis is a qualitative, descriptive and exploratory study. It is an intrinsic case study of Peer- tutors’ performance, shared the same experience. The techniques and instruments used were a questionnaire with its survey and two focus groups with the same thematic script. A thematic analysis of the tutors’ notes was carried out.
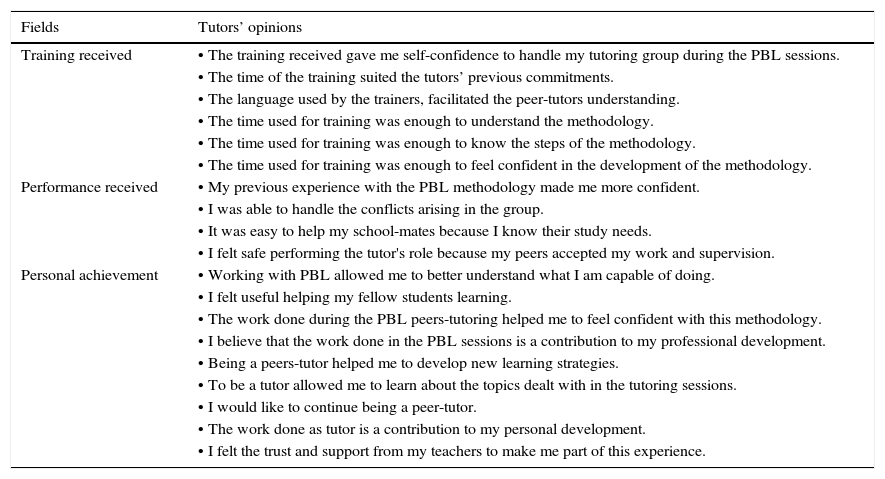
All tutors completed the training program since 2007, were asked to express their opinion by answering a Likert scale based survey composed of 4 ordinal categories: total agreement, medium agreement, limited agreement and disagreement; to collect their perceptions in relation to the consulted three areas, namely: training received, performance perceived and personal achievement (Table 1).
Aspects addressed in every field of the survey.
| Fields | Tutors’ opinions |
|---|---|
| Training received | • The training received gave me self-confidence to handle my tutoring group during the PBL sessions. |
| • The time of the training suited the tutors’ previous commitments. | |
| • The language used by the trainers, facilitated the peer-tutors understanding. | |
| • The time used for training was enough to understand the methodology. | |
| • The time used for training was enough to know the steps of the methodology. | |
| • The time used for training was enough to feel confident in the development of the methodology. | |
| Performance received | • My previous experience with the PBL methodology made me more confident. |
| • I was able to handle the conflicts arising in the group. | |
| • It was easy to help my school-mates because I know their study needs. | |
| • I felt safe performing the tutor's role because my peers accepted my work and supervision. | |
| Personal achievement | • Working with PBL allowed me to better understand what I am capable of doing. |
| • I felt useful helping my fellow students learning. | |
| • The work done during the PBL peers-tutoring helped me to feel confident with this methodology. | |
| • I believe that the work done in the PBL sessions is a contribution to my professional development. | |
| • Being a peers-tutor helped me to develop new learning strategies. | |
| • To be a tutor allowed me to learn about the topics dealt with in the tutoring sessions. | |
| • I would like to continue being a peer-tutor. | |
| • The work done as tutor is a contribution to my personal development. | |
| • I felt the trust and support from my teachers to make me part of this experience. |
In order to collect further detailed first-hand personal tutoring experiences; two focus group sessions were conducted with 2 and 3 years old peer-tutors at the time of this study. Due to the tutors’ diverse activities, it was impossible to coordinate both groups attending to a single focus group session.
The topics addressed in the focus group were: (1) Reasons to remain being a PBL peer-tutor, (2) Self-confidence with this activity throughout these experiences over the years, (3) Interest in a future academic career, (4) PBL peer-tutor work versus medical training.
Ethical considerationsThe publication of these data for academic and/or research purposes was approved by the Faculty of Medicine's Ethics Committee and the participants’ voluntary informed consent. This was not initially requested because peer tutoring sessions were one of the course activities.
ResultsNinety five peer-tutors were trained between 2007 and 2014 and worked as PBL peer-tutors in different courses from 1st to 3rd year Medical School, and in other Schools of the Faculty of Medicine. Considering the entire period, 85 peer-tutors answered the survey, representing 89.5% of all students trained.
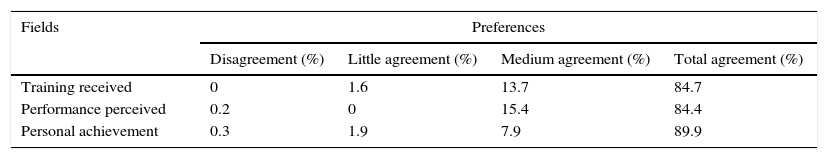
The percentage distributions of the preferences in the 3 areas consulted are shown in Table 2. The results showed that 84.7% of the peer-tutors expressed Total Agreement with the training received, followed by 13.7% which corresponded to Medium Agreement. Aspects related to group management and time spent in the initial training, were perceived by the peer-tutors as sufficient and adequate, respectively.
Similarly, the tutors’ perceptions of their performance were; 84.4% Total Agreement and 15.4% Medium Agreement. Previous experience with PBL peer-tutors at the same school gave them self-confidence to perform as peer-tutor, and to better understand the group's cognitive needs.
The personal achievement dimension is the one with the highest responses; 89.9% for the Total Agreement category, followed by 7.9% for Medium Agreement. This dimension counts for discovering new skills, developing other strategies for learning and to reinforce essential key concepts for their future life as doctors.
Despite the three very well evaluated areas by the tutors, the excellent perception of the “Personal Achievement” dimension is highlighted. Tutors believe that tutoring is a great contribution to their personal development, and they feel more self-confident and useful when facilitating peers’ learning.
The focus group sessions were conducted. One focus group session was planned for tutors who were in 5th year of Medical School (n=9) and with three years of experience in PBL tutoring at the time of this study, and the other for 4th year students (n=6) with two years of experience. The tutors’ responses in the focus group sessions were collected and analyzed according to the topics addressed. Regardless of the years of experience, all the peer-tutors shared the same perceptions.
Reasons to remain being a PBL peer-tutorThe answers were: “Because it's fun,” “I like being a pseudo teacher”, “I like to guide and teach other students.” “It is gratifying”, “I like to share with other students of the Medical School”, “This activity has a reasonable and flexible workload” and “There are good coordination and communication with the tutors’ training team”. “Instructions are clear to follow.” In addition, “tutors and students develop self-confidence”, “they learn how to consolidate knowledge, which is very good for the following years in the Medical School.”
Based on the answers it is possible to perceive that Tutors feel that this activity forces them to organize, to understand and to consolidate knowledge, it allows them to share their relevant clinical experiences to the study case to promote students motivation. Tutors also think it is very good to show real clinical cases to the students who are starting their medical training.
Regarding the tutoring environment, tutors agree on the fact that it is a very comfortable atmosphere, with students feeling free to participate and without fear of making mistakes. Students are relaxed, not afraid to ask or being laughed at. They feel that this way of working can be applied to any case. Peer-tutors enjoy this activity very much because it takes them close to the reality of teaching. Some would imitate the good tutor they had when they knew PBL methodology, in the first year of Medical School. Others pointed out that what matters most to them is to develop a different way of learning, not just rote learning. In consensus, they feel that students dare to ask more than in traditional classes because they are in a small group.
Self-confidence with this activity throughout these experiences over the yearsEveryone answered yes. They mentioned that thanks to the PBL peers-tutor sessions carried out in previous years, they were able to approach and to organize a study case using this methodology. They feel more confident to deal with a patient, to apply clinical reasoning, to mentally structure the relevant information and to know how to act in the clinical practice.
Interest in a future academic careerThey replied to have thought of teaching in the future. They feel that the PBL model helps them to organize themselves better, to be more self-confident. It provides them with tools for group managing and motivation, and allows them to sort out ideas, efficiently. They also mentioned to have learned more medical knowledge as tutors than as students; they learned how to be organized as well as to know how to teach others and to develop a more efficient mental structure. They have learned new things and reinforced previous acquired knowledge.
One female student said she had always wanted to be a teacher. This comment was shared by another student who pointing out that PBL tutoring has reinforced this feeling in her. Two students said they did not want to be teachers before, but after doing peer tutoring, they have seriously considered that possibility.
PBL peer-tutor work versus medical trainingThey mentioned that being a peer-tutor in PBL allowed them to develop self-confidence on the knowledge to be tutored. It has motivated them to be sociable and to interact with other students from the Medical School; it promotes the curiosity for searching, to learn how to manage concepts in different forms for “others” to learn. They have learned to be patient and to encourage students to explain their peers’ different medical concepts, according to their own pace. They have become versatile in the way of delivering knowledge. They are responsible, meet schedules, have clear objectives, and stimulate the acquisition of knowledge by their peers, adequately.
Discussion and conclusionsPeer tutoring has been used for many years in secondary and university education, with students showing learning difficulties or as part of the methodology of a particular subject of the study curriculum.8 These authors suggest that peer tutoring is one of the most practical approaches to customize instruction in an educational setting. However, some medical schools have used senior students in teaching roles with school's freshmen, with excellent results.9 In addition, Isaza et al., reported their experience with a peer-tutors Program at the Faculty of Medicine in Rosario, Bogotá, Colombia.10 These authors showing the benefits of this practice, the process experienced by the students, the customized instruction and the importance of the social interaction in the building up of knowledge. They also highlighted the synergistic value of an experience that not only starts the period of teacher training and academic support, but also promoting a proactive attitude toward learning.
When inquiring about the existence of academic support services in US Medical Schools and Canada, 56% of graduates were happy with the tutorial assistance given by peers during their training.11 In 1989, 127 medical schools were surveyed in USA and from those who responded (48.8%), 75.8% had peered-tutoring programs.12
In our country, some universities have also incorporated trained peer tutors, as a beneficial and motivating academic experience to encourage learning among students13; (Estupiñan et al., 2014 International Congress University and Vulnerable Communities. Veracruz, México). Despite the fact that the PBL methodology is standardized, its success depends largely on tutors’ teaching strategies to facilitate group dynamics and learning rhythms of an individual as well as a group.14
The large number of students per courses and the lack of expert PBL-tutors or teachers willing to become PBL-tutors, are world-wide problems and one way to cope with them, is to use trained higher courses medical students to work as PBL peer-tutors.15 However, in 2007, the UACh Medical School created a PBL peer-tutoring program to successfully put into practice the PBL methodology. The peer-tutors program emerged as a viable alternative to incorporate this new educational approach early in the Medical School. This training program allowed medical students to experience a student-centered education by working under the essential PBL concepts, and also to train medical students from higher courses to work as peer-tutors.
Every year there is a great interest from the students to apply for this training program, because of their own experience as PBL students, as well as the personal experience tutors have shared with them over the years. In addition, evaluating their tutors has given them a critical judgment and opinion of the peer-tutors role. Kassab considers important and necessary to have a prior training as tutor, and a permanent support during PBL-tutoring sessions.16
Peer-tutors share their academic experiences with their groups and this represent a great input to the learning process of the new students of the same school. It is a pleasant instance of learning to have peer-tutors. It has potentially positive effects on tutors; it triggers the commitment to become socially responsible toward their school classmates and it is a role-model for the new generations of students.8
A peer-tutor is able to tune better with their peers, thus providing a better guidance and support in the self-learning process. On the other hand, in the IV Latin American Conference on abandonment in higher education Medellin, Colombia 2014, Maillard mentioned that it is an enriching experience for the tutor to promote values that strengthen their personal life and professional future.
In order to know the student–tutors perception regarding peer tutoring, the PBL training team invited them to participate in a focus group to discuss their perceptions regarding the work in PBL tutorials. Both, students who had three years as tutors, as well as those with two years’ experience, agreed that the activity was fun, rewarding, well-coordinated, with time adequate to their personal availability. It allowed them to sort out, consolidate and reflect on the specific knowledge involved in each session thus, taking advantage of sharing their personal clinical experiences with their peers. In addition, it is worth mentioning the increasing acceptance of peer-tutors by the students. In a more relaxed atmosphere, they felt free to express themselves and to make questions and therefore, enriching the process of self-learning. In addition, tutors stimulate a far more significant way to learn than the traditional one, by sharing their own experiences in the clinical setting, especially with students in the early years of Medical School.
Moreover, this activity required from them to organize the knowledge prior the tutoring session and as a result of this, it helped them to systematize it for their own benefit, to become more self-confident, to organize themselves better, to be more responsible with time-schedules, to develop a reflective and critical attitude and an in-depth acquisition of knowledge.
Interestingly, the PBL peer-tutors perception is in line with various authors such as Salerno-Kennedy et al.,17 Isaza et al.,10 and Escupiñan et al. (2014 International Congress University and Vulnerable Communities, Veracruz, México), who reported that peer-tutors have a very positive view of their role.
Peer-tutoring in PBL reinforces the skills and outcomes of the medical student graduate's profile, and it also stimulates the development of their own self-learning, communication and teacher's motivation skills. The above is very important because it prepares peer-tutors early in their training, to perform with maturity and self-confidence throughout their medical training.
Finally, we concluded that using peer-tutors resulted in students empowered of their future professional role in society and familiarized with a holistic approach to health problems.
Limitations, strengths and areas of weaknessThis study was designed to know the peer-tutors perceptions of their own performance and accomplishments, and not the students ‘perceptions of their tutors.
One of the greatest strengths was the high level of interest and motivation shown by the peer-tutors throughout the peer tutoring season. This greatly facilitated the organization of the Focus Group and the information collection using the survey, even from those peer-tutors who had already graduated from the medical school at the time of this survey.
Previous presentationXXII Congreso de la Sociedad Española de Educación Médica. III Reunión Hispano-Portuguesa de Educación Médica. Murcia, España, Octubre 2015.
Award and recognitionPanel mode.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial supportNone.
Author contributionA. V.: Development of research, interpretation and analysis of results, drafting and preparation of the manuscript, review, editing and submission.
R. C.: Development of research, interpretation and analysis of results, drafting and preparation of the manuscript, English revision editing.
J. G.: Data collection, tabulation of surveys and execution of tables.
Conflict of interestThere is no conflict of interest.
We would like to thank peers-tutors from the Austral University of Chile Medical School, for their permanent work with undergraduate medical students.
Peer Review under the responsibility of Universidad Nacional Autónoma de México.