In Australia, medical students usually undertake a series of 6–8 weeks long clinical specialty placements, and mainly in urban teaching hospitals. As part of a strategy to increase interest in rural careers, students at some medical schools may instead choose longer, more generalist clinical placements through either rural medical schools or rural clinical schools that are affiliated with urban medical schools. These placements involve varying combinations of rotations for periods up to a whole academic year in more generalist hospital and family practice settings. Models include rural longitudinal integrated clerkships (LICs), rural clinical schools, and rural medical schools. Little is known about the effect of these longer placements on career outcomes in Australia.
MethodStudent category and placement data from the Medical Student Outcomes Database project was sourced for three categories of medical students commencing in 2008 and 2009: 276 students with at least 700h (about half an academic year) in rural clinical placements; 772 students at the same medical schools with less than 700h in rural clinical placements; and 5326 students at 16 medical schools that either did not offer longer rural placements or had very small numbers undertaking them. Data were compared from all three groups using the Chi Square statistic.
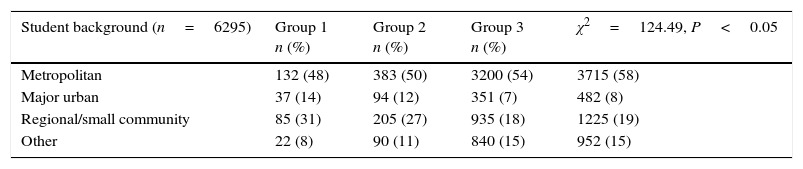
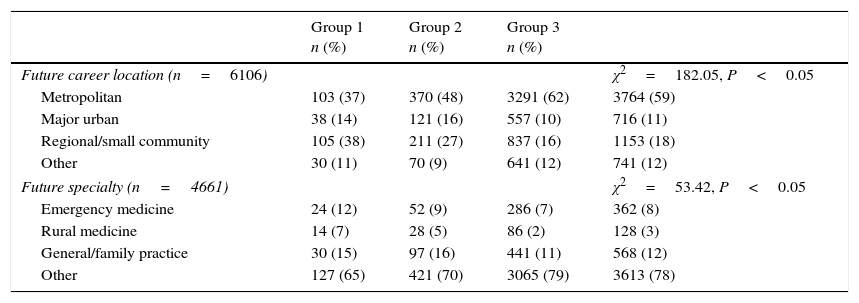
ResultsThere were a total of 3483 students in commonwealth supported places without a rural obligation (CSP); 1375 students in CSPs with a rural obligation; 414 in domestic full fee (DFF) places; and 926 in international full fee (IFF) places. CSP students are more likely, and IFF students are less likely to choose an LRP (χ2 statistic 56.4, P<0.05). Students choosing a LRP are more likely to have a rural background (χ2 statistic 124.5, P<0.05) and a preference for careers outside metropolitan areas, particularly in smaller communities (χ2 statistic 182.2, P<0.05). Future specialty preferences of LRP students are similar to other students, except for emergency medicine and rural medicine, but not for family practice (chi-squared statistic 53.4, P<0.05).
Discussion and conclusionsLonger rural placements appear to be associated with stronger preference at graduation for rural careers, and appear to be a valid strategy for enhancing rural workforce outcomes. More research is needed to determine the outcomes of all models of longer rural placements, including a comparison of the different models that include longer rural placements. The relevance to other education systems and national contexts also needs examining.
En Australia, los estudiantes de medicina rotan en especialidades clínicas durante 6-8 semanas en hospitales urbanos. Para aumentar el interés por las carreras rurales, los estudiantes de algunas escuelas pueden elegir rotaciones de mayor duración (hasta un año) en clínicas rurales. Las rotaciones longitudinales integradas (LIC, por sus siglas en inglés) ocurren en lugares de atención primaria, como clínicas rurales y escuelas de medicina rural.
ObjetivoEvaluar el efecto de las rotaciones rurales más extensas sobre la decisión final en la carrera de medicina en Australia.
MétodoSe estudiaron 3 grupos de estudiantes graduados en 2011: 276 con al menos 700h de prácticas rurales (casi la mitad del año académico), 772 de las mismas escuelas con menos de 700h de prácticas rurales y 5,326 de 16 escuelas que, o bien no ofrecieron rotaciones rurales, o muy pocos las realizaron. Se compararon los datos de los 3 grupos con la prueba de χ2.
ResultadosUn total de 3,483 estudiantes fueron de lugares otorgados por la Commonwealth (CSP); 1,375 de lugares asegurados con rotaciones rurales (MRBS) o médicas (BMP); 414 con pago completo en lugares domésticos (DFF), y 926 en zonas con pago completo internacional (IFF). Es más probable que los estudiantes CSP elijan una LIC en comparación con los IFF (χ2 56.4; p<0.05). Los que eligieron una LIC tuvieron más rotaciones rurales (χ2 124.5, p<0.05) y elección por las carreras fuera de las áreas metropolitanas y en comunidades más pequeñas (χ2 182.2, p<0.05). Aquellos que realizaron LIC tuvieron preferencias similares a las de otros estudiantes en las carreras futuras, con excepción de medicina de urgencias y medicina rural, aunque no para medicina familiar (χ2 53.4; p<0.05).
Discusión y conclusionesLos médicos con rotaciones rurales parecen tener mayor preferencia por carreras en el área rural una vez graduados, lo que parece ser una estrategia que podría aumentar el número de médicos en áreas rurales. Se necesita más investigación para determinar los desenlaces de todos los modelos de las rotaciones rurales, con la inclusión de modelos de hospitales más pequeños de medicina general y modelos de atención primaria. La relevancia para otros sistemas de educación y el contexto en Australia también deben ser estudiados.
The most common model of basic medical education provides medical students with a substantial foundation in the biomedical sciences before exposing patients to them for apprenticeship-style clinical placements that rotate through traditional hospital-based clinical specialties, usually in large academic centres. Over the last four decades, curricula have become more diverse through increased utilisation of smaller hospitals and primary care practice settings, particularly in underserved, often rural, communities, offering more integrated clinical experiences that reflect community and workforce needs.1–3
Three kinds of models have developed from pioneering programmes that immersed either junior or senior medical students in a rural community. Most of these developments are located in North America and Australia,4 although there is one similar model in the United Kingdom.5 In the first model more senior students are immersed for up to a whole academic year in a rural community, are based in primary care learning all general specialties under the guidance of family doctors and visiting consultants, and achieve equivalent student assessment results.6,7 This model has evolved into longitudinal integrated clerkships (LICs), which are offered by several medical schools around the world, adapted to both urban and rural environments.8 Substantial effort goes into making these placements a genuine integration of multiple specialty content through longitudinal participation in patient care journeys in primary and secondary care, which is different to the ‘normal’ primary care placements.9 The second model sees students of urban-based medical schools allocated for at least one of the final two years to a regional or rural clinical school campus for more generalist clinical placements in smaller hospitals and rural primary care clinics.10 The third model sees the entire medical curriculum delivered in regional and rural communities at a ‘rural medical school’.4
In Australia, all three longer rural placement (LRP) models have been adopted by several medical schools as strategies to improve student interest in rural careers.11 Early evaluations of individual programmes suggest that students choose LRPs for a richer learning environment and to ‘test’ the possibility of a living in a rural community, thus exploring the possibility of choosing a rural career more effectively than in shorter placements.12
The medical education funding model in Australia is complex. Most domestic medical students are government-subsidised (commonwealth supported places or CSPs), with some additional places carrying requirements for return of service obligation for a period of rural service, and a smaller number of mostly international students pay full fees. Students in these different categories may have different career expectations and interests.
While all three models build on medical education evidence, more research is necessary to explore their impact on learners across different models and institutions. This paper explores the background and career preferences of medical students choosing to participate in longer duration rural clinical placements, drawing data from all Australian medical schools using a variety of LRP models.
MethodStudent category and placement data were sourced from the Medical Student Outcomes Database project of Medical Deans Australia and New Zealand (MDANZ), a Federal Government funded initiative designed to assist the evaluation of rural medical education strategies.13 In this project questionnaires were administered to students at all Australian and New Zealand medical schools at commencement and exit, and then during postgraduate year 1 (PGY1), with potential linkage to later postgraduate data sources. Data at graduation were analysed for students commencing in 2008 and 2009 (the most recent data available) and divided into three groups. The first included 276 students choosing to spend at least 700h (20h×35h weeks or about half an academic year) in clinical placements in rural communities. For confidentiality reasons, data could be accessed for only the five schools with more than 20 students each in longer rural placements: all of these schools have a substantial rural emphasis in their selection, curriculum and clinical placement practices. The second group included 772 students who had spent less than 700h in rural clinical placements but had attended the same five medical schools. The third group included 5326 students who had spent less than 700h in rural clinical placements and had attended the other 14 medical schools, which tended to be less focused on rural medical education initiatives or had fewer than 20 students with longer rural placements. It is therefore possible that some students who should have been in Group 1 were in Group 3, potentially weakening differences between those groups. Data were analysed using the Chi Square statistic, focusing on rural background and future career preferences of students in the three groups, reflecting differences in duration of rural placements.
Ethical considerations. Ethics approval was covered by the MSOD project, which has approval by ethics committees at all participating Universities (see http://www.medicaldeans.org.au/medical-schools-outcomes-database/for-participants/university-human-research-ethics-compliance).
ResultsData were received for a total of 6374 students, although some data was missing for each of the variables under consideration. There were 3483 students in commonwealth supported places (CSPs) without any rural obligation, 1375 in CSPs with some form of rural obligation, 414 in domestic full fee (DFF), 926 in international full fee (IFF) and 176 in Other places (e.g. Defence Force scholarships). There were differences between the groups with respect to student place category, rural background and future career preference. CSP students were more likely, and IFF students less likely, to choose an LRP (χ2 statistic 56.4, P<0.05). Of interest is the lack of association between CSPs with a rural obligation and longer rural placements. Students who had completed more than 20 weeks of rural placement were more likely to have a rural background (χ2 statistic 124.5, P<0.05) and a preference for careers outside of metropolitan areas, particularly in smaller communities (χ2 statistic 182.2, P<0.05). Future specialty preferences of LRP students are similar to other students, except for emergency medicine, and rural medicine, although not family practice (chi-square statistic 53.4, P<0.05). These data are summarised in Tables 1 and 2.
Student background by group.
| Student background (n=6295) | Group 1 n (%) | Group 2 n (%) | Group 3 n (%) | χ2=124.49, P<0.05 |
|---|---|---|---|---|
| Metropolitan | 132 (48) | 383 (50) | 3200 (54) | 3715 (58) |
| Major urban | 37 (14) | 94 (12) | 351 (7) | 482 (8) |
| Regional/small community | 85 (31) | 205 (27) | 935 (18) | 1225 (19) |
| Other | 22 (8) | 90 (11) | 840 (15) | 952 (15) |
Career preference by location and specialty.
| Group 1 n (%) | Group 2 n (%) | Group 3 n (%) | ||
|---|---|---|---|---|
| Future career location (n=6106) | χ2=182.05, P<0.05 | |||
| Metropolitan | 103 (37) | 370 (48) | 3291 (62) | 3764 (59) |
| Major urban | 38 (14) | 121 (16) | 557 (10) | 716 (11) |
| Regional/small community | 105 (38) | 211 (27) | 837 (16) | 1153 (18) |
| Other | 30 (11) | 70 (9) | 641 (12) | 741 (12) |
| Future specialty (n=4661) | χ2=53.42, P<0.05 | |||
| Emergency medicine | 24 (12) | 52 (9) | 286 (7) | 362 (8) |
| Rural medicine | 14 (7) | 28 (5) | 86 (2) | 128 (3) |
| General/family practice | 30 (15) | 97 (16) | 441 (11) | 568 (12) |
| Other | 127 (65) | 421 (70) | 3065 (79) | 3613 (78) |
This analysis supports the importance of the rural medical education initiatives for medical workforce development in Australia. Students completing longer rural placements of at least half an academic year in a variety of curriculum models are more likely to express a preference at graduation for a rural career location, thus strengthening earlier research findings.14 Further, their career preferences are for the specialties of rural medicine and emergency medicine. These findings provide additional evidence that rural background students should have their interest in rural lifestyle fostered by undertaking a substantial proportion of their clinical placements in rural and regional communities.
There are however insufficient data to go beyond supporting the concept that ‘more may be better’ with respect to rural placements and rural career preferences. The numbers of students undertaking longer rural placements is relatively small and divided amongst the three LRP models that are not available at all Australian medical schools. There are differences between medical schools in the proportions of rural background students and investment in rural medical education. These variables are not independent, as rural background alone is a predictor of future rural careers, and may be even stronger in combination with rural placements.15 There may therefore be a ‘school effect’, with the more rurally-focused medical schools attracting a different student profile that may pre-dispose graduates to a different future workforce preference.
This analysis cannot contribute to the discussion about which of the three LRP models may be most effective. In other research, the strongest rural workforce outcomes appear to come from medical schools with the third LRP model, such as at James Cook University and Northern Ontario School of Medicine.16,17 The Australian Rural Clinical School model (the second LRP model) has also been shown to be effective at fostering rural career interest in urban-background students in metropolitan medical schools.18 It is possible that expanding the availability of longer rural placements through any of the three available models would further increase the proportion of medical graduates with a preference for careers outside of metropolitan centres.
LimitationsData were available from only those medical schools with more than 20 students in each cohort able to undertake longer rural placements. These may be the more rurally-focused medical programmes that may attract more rural background students and invest more in other rural medical education initiatives. Rural predictors are unlikely to be independent variables, so selection bias and confounding are likely. Further, these analyses do not differentiate between the different medical programme models that offer longer rural clinical placements. Further research is necessary to explore the relative effect on rural career preference of the rural longitudinal integrated clerkship, rural clinical school and rural medical school models.
ConclusionRural clinical placements longer than about half an academic year in any of the three models used in Australia may be associated with an increase in preference for careers in rural communities, particularly rural medicine and emergency medicine. Further research is necessary to explore the relative effectiveness of the different models on rural career preference and the relevance to other medical education and health care systems.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was provided.
Conflict of interestThe author has no conflicts of interest to declare.
Peer Review under the responsibility of Universidad Nacional Autónoma de México.