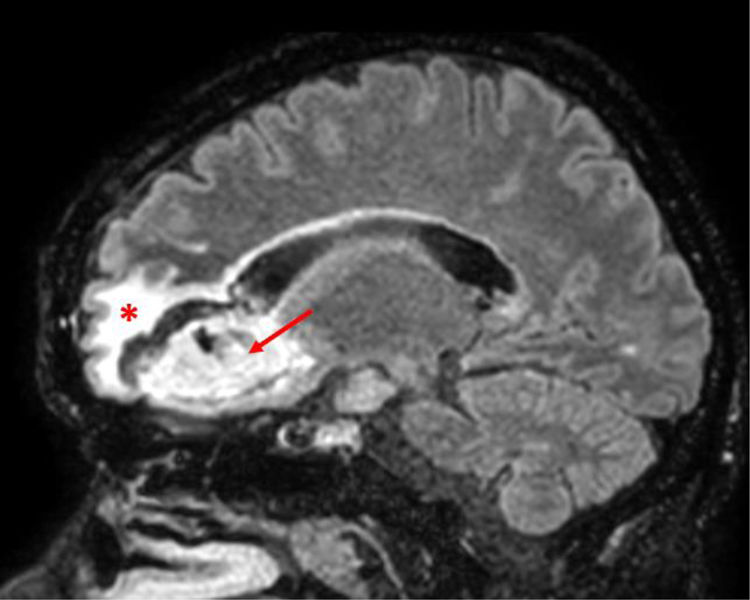
array:24 [ "pii" => "S2387020621006422" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.12.036" "estado" => "S300" "fechaPublicacion" => "2021-12-10" "aid" => "5591" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2021" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2021;157:e339-e340" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S002577532100083X" "issn" => "00257753" "doi" => "10.1016/j.medcli.2020.12.034" "estado" => "S300" "fechaPublicacion" => "2021-12-10" "aid" => "5591" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2021;157:e339-e340" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Absceso cerebral por <span class="elsevierStyleItalic">Cutibacterium acnes</span> en un paciente con infección por el VIH" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e339" "paginaFinal" => "e340" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Brain abscess due to <span class="elsevierStyleItalic">Cutibacterium acnes</span> in a patient with HIV infection" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 600 "Ancho" => 750 "Tamanyo" => 47015 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Corte sagital de resonancia magnética donde se aprecia LOE con captación de contraste en anillo a nivel del lóbulo frontal izquierdo (flecha), con importante edema perilesional (asterisco).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "María José Arche Banzo, Herminia Lozano Gómez, Sandra Herrero García" "autores" => array:3 [ 0 => array:2 [ "nombre" => "María José" "apellidos" => "Arche Banzo" ] 1 => array:2 [ "nombre" => "Herminia" "apellidos" => "Lozano Gómez" ] 2 => array:2 [ "nombre" => "Sandra" "apellidos" => "Herrero García" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020621006422" "doi" => "10.1016/j.medcle.2020.12.036" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621006422?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S002577532100083X?idApp=UINPBA00004N" "url" => "/00257753/0000015700000011/v1_202111210516/S002577532100083X/v1_202111210516/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020621006082" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.12.029" "estado" => "S300" "fechaPublicacion" => "2021-12-10" "aid" => "5590" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2021;157:e341-e342" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Frontal fibrosing alopecia in a woman with vulvar erosive lichen planus" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e341" "paginaFinal" => "e342" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Alopecia frontal fibrosante en una mujer con liquen plano erosivo vulvar" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1381 "Ancho" => 1505 "Tamanyo" => 311056 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(a) Red erosion on the inner side of left minor labia, surrounded by a whitish area (arrow). A small whitish area is also noted on the inner aspect of right minor labia (asterisk). (b) Small scarring alopecic area placed in the right fronto-temporal side (asterisk), with subtle loss of density in the right sideburn. (c) No frontal hairline recession. (d) Dermoscopy showed loss of follicular openings (asterisk) with subtle perifollicular hyperkeratosis (arrows), and a whitish background (Dermlite 2PRO HR, polarized light, 10×).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "María Librada Porriño-Bustamante, Pablo Lázaro-Ochaita, María Antonia Fernández-Pugnaire" "autores" => array:3 [ 0 => array:2 [ "nombre" => "María Librada" "apellidos" => "Porriño-Bustamante" ] 1 => array:2 [ "nombre" => "Pablo" "apellidos" => "Lázaro-Ochaita" ] 2 => array:2 [ "nombre" => "María Antonia" "apellidos" => "Fernández-Pugnaire" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S0025775321000828" "doi" => "10.1016/j.medcli.2020.12.033" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321000828?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621006082?idApp=UINPBA00004N" "url" => "/23870206/0000015700000011/v1_202112030828/S2387020621006082/v1_202112030828/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020621006380" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.12.033" "estado" => "S300" "fechaPublicacion" => "2021-12-10" "aid" => "5586" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2021;157:e337-e338" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Spontaneus gas gangrene due to <span class="elsevierStyleItalic">Clostridium septicum</span> in a neutropenic patient" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e337" "paginaFinal" => "e338" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Gangrena gaseosa espontánea por <span class="elsevierStyleItalic">Clostridium septicum</span> en paciente neutropénica" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Elena Cuenca Fito, Elsa Ots Ruiz, M. Soledad Holanda Peña" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Elena" "apellidos" => "Cuenca Fito" ] 1 => array:2 [ "nombre" => "Elsa" "apellidos" => "Ots Ruiz" ] 2 => array:2 [ "nombre" => "M. Soledad" "apellidos" => "Holanda Peña" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775321000786" "doi" => "10.1016/j.medcli.2020.12.029" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775321000786?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621006380?idApp=UINPBA00004N" "url" => "/23870206/0000015700000011/v1_202112030828/S2387020621006380/v1_202112030828/en/main.assets" ] "en" => array:17 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Brain abscess due to <span class="elsevierStyleItalic">Cutibacterium acnes</span> in a patient with HIV infection" "tieneTextoCompleto" => true "saludo" => "Dear Editor:" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e339" "paginaFinal" => "e340" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "María José Arche Banzo, Herminia Lozano Gómez, Sandra Herrero García" "autores" => array:3 [ 0 => array:4 [ "nombre" => "María José" "apellidos" => "Arche Banzo" "email" => array:1 [ 0 => "mariajosearchebanzo@gmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "*" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "Herminia" "apellidos" => "Lozano Gómez" ] 2 => array:2 [ "nombre" => "Sandra" "apellidos" => "Herrero García" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Servicio de Medicina Intensiva, Hospital Clínico Universitario Lozano Blesa, Zargoza, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Absceso cerebral por Cutibacterium acnes en un paciente con infección por el VIH" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 600 "Ancho" => 750 "Tamanyo" => 47015 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Sagittal section of an MRI scan showing a SOL with annular contrast uptake at the level of the left frontal lobe (arrow), together with a large perilesional edema (asterisk).</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Establishing a differential diagnosis of cerebral space-occupying lesions (SOLs) is currently a challenge at a disciplinary level. Reaching an early and accurate diagnosis can lead to significant improvements in the vital prognosis and morbidity linked to the disease.</p><p id="par0010" class="elsevierStylePara elsevierViewall">In this paper we describe the case of a 36-year-old man from Ghana, without a remarkable previous medical history. He visited the Emergency Department due to experiencing a persistent headache of several weeks’ evolution. A brain computed tomography (CT) scan revealed a left, frontal, cerebral SOL with annular contrast uptake and a large perilesional edema. Considering this finding, he was admitted to the Infectious Diseases Department.</p><p id="par0015" class="elsevierStylePara elsevierViewall">An immunity study revealed a human immunodeficiency virus (HIV) infection with an acquired immunodeficiency syndrome (AIDS) clinical category of C3 and an initial CD4 lymphocyte count of 7 cells/mm<span class="elsevierStyleSup">3</span>. Targeted treatment for cerebral toxoplasmosis with sulfadiazine, pyrimethamine, and trimethoprim-sulfamethoxazole was started, together with dexamethasone for his perilesional edema. A magnetic resonance imaging (MRI) scan showed multiple cerebral lesions, all of which also exhibited annular contrast uptake (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0020" class="elsevierStylePara elsevierViewall">His clinical evolution was unfavorable in the following weeks, with the onset of pancytopenia, a high fever, and a progressively lower level of consciousness, owing to which he had to be admitted to the Intensive Care Unit (ICU) with orotracheal intubation and mechanical ventilation. Given his clinical worsening, the antibiotic coverage was broadened with meropenem, vancomycin, clindamycin, and fluconazole, and antiretroviral therapy with abacavir/dolutegravir/lamivudine was also started.</p><p id="par0025" class="elsevierStylePara elsevierViewall">A lumbar puncture was performed, obtaining a sample of colorless cerebrospinal fluid (CSF), albeit with positive polymerase chain reaction (PCR) and IgM serology tests for human herpesvirus 6 (HHV-6). In addition, a stereotactic biopsy of the SOL yielded findings compatible with an infectious process. Ganciclovir was subsequently also added to his treatment regimen, without achieving improvements in his level of consciousness. Finally, after spending three weeks in the ICU, a microbiological culture of the biopsy sample revealed isolates of <span class="elsevierStyleItalic">Cutibacterium acnes</span>. Thus, his antibiotic therapy was adjusted once again and de-escalated to ceftriaxone and vancomycin.</p><p id="par0030" class="elsevierStylePara elsevierViewall">After developing multiple nosocomial infections during his two-month hospital stay, the patient eventually passed away.</p><p id="par0035" class="elsevierStylePara elsevierViewall"><span class="elsevierStyleItalic">Cutibacterium acnes</span> (formerly known as <span class="elsevierStyleItalic">Propionibacterium acnes</span>) is an opportunistic, gram-positive, anaerobic, aerotolerant bacillus capable of forming filaments. It is part of the normal human mucocutaneous microbiome, mainly of the sebaceous glands, with infections by this microorganism being more frequent in immunocompromised patients or those with foreign prosthetic material.<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,2</span></a></p><p id="par0040" class="elsevierStylePara elsevierViewall">Because it is a slow-growing germ with low virulence, the infection often remains latent up to several months after the inoculation. It can cause infections in multiple locations, including postoperative central nervous system (CNS) infections or brain abscesses originating in the sinuses. It is also involved in the pathogenesis of acne vulgaris and has been associated with synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome (chronic recurrent multifocal osteomyelitis with acne and pustulosis). Considering that recent research on CNS infections by <span class="elsevierStyleItalic">Cutibacterium</span> sp. has shown that other pathogens are involved in 29% of patients and that 38% have been classified as contaminants, clinical correlation is crucial.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3,4</span></a></p><p id="par0045" class="elsevierStylePara elsevierViewall">Its diagnosis is reached by means of a culture of samples for at least 7–10 days in anaerobic conditions. Its identification by Matrix Assisted Laser Desorption/Ionization Mass Spectrometry (MALDI-TOF) is also possible.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a></p><p id="par0050" class="elsevierStylePara elsevierViewall">Targeted therapy for <span class="elsevierStyleItalic">C. acnes</span> should be administered in monotherapy with a beta-lactam antibiotic (ceftriaxone or amoxicillin), teicoplanin, or vancomycin. This microorganism is intrinsically resistant to metronidazole (despite growing in anaerobic media) and is often resistant to aminoglycosides. In cases of infection of prosthetic material, combined treatment with levofloxacin and rifampicin is ideal, and removal of the prosthetic material, debridement, or the drainage of collections is essential.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3–5</span></a></p><p id="par0055" class="elsevierStylePara elsevierViewall">The existing literature, mainly consisting of clinical case reports, indicates that the antibiotic treatment should be prolonged for six weeks, although the determining factor that can aid in establishing the appropriate treatment duration is the patient’s clinical response.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a></p><p id="par0060" class="elsevierStylePara elsevierViewall">Given the increase in the number of infections by this microorganism and the diagnostic challenge that they represent, <span class="elsevierStyleItalic">C. acnes</span> should be considered as a potential agent in CNS infections. Its atypical clinical presentation and neuroimages, as well as a history of immunosuppression, CNS surgery, or head trauma, should lead to a suspicion of this entity.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflicts of interest</span><p id="par0065" class="elsevierStylePara elsevierViewall">The authors declare that they have no conflict of interest and that they have not received any type of financial support for the conduct of this study.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:3 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflicts of interest" ] 1 => array:2 [ "identificador" => "xack571968" "titulo" => "Acknowledgments" ] 2 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "⋆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Arche Banzo MJ, Lozano Gómez H, Herrero García S. Absceso cerebral por Cutibacterium acnes en un paciente con infección por el VIH. Med Clin (Barc). 2021;157:e339–e340.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 600 "Ancho" => 750 "Tamanyo" => 47015 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Sagittal section of an MRI scan showing a SOL with annular contrast uptake at the level of the left frontal lobe (arrow), together with a large perilesional edema (asterisk).</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Brain abscess-diagnosis and management" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "A.A. Bhand" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "07.2004/JCPSP.407410" "Revista" => array:6 [ "tituloSerie" => "J Coll Physicians Surg Pak" "fecha" => "2004" "volumen" => "14" "paginaInicial" => "407" "paginaFinal" => "410" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/15279742" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Sinusitis esfenoidal erosiva asintomática" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "E.A. Mena-Domínguez" 1 => "J. Santos-Pérez" 2 => "T. Millas-Gómez" 3 => "G.A. Landínez-Cepeda" 4 => "M.C. Martín-pascual" 5 => "D. Morais-Pérez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Rev Soc Otorrinolaringol Castilla Leon Cantab La Rioja" "fecha" => "2013" "volumen" => "4" "paginaInicial" => "111" "paginaFinal" => "116" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Abscesos cerebrales: análisis de factores pronóstico e influencia del tratamiento antibiótico protocolizado en su evolución" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J. Gómez" 1 => "E. García-Vázquez" 2 => "M. Martínez" 3 => "J. Martínez" 4 => "J. González" 5 => "M.A. Pérez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "An Med Interna (Madrid)" "fecha" => "2008" "volumen" => "25" "numero" => "7" "paginaInicial" => "331" "paginaFinal" => "334" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Absceso cerebral post-traumático recidivante: Revisión de un caso" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "R. García-Angelo" 1 => "M.E. Pérez-Chacón" 2 => "D.A. Vila-Melgarejo" 3 => "A. Flores-Herbas" 4 => "L. Camacho-Aguilar" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Rev Méd-Cient “Luz Vida”" "fecha" => "2012" "volumen" => "3" "paginaInicial" => "61" "paginaFinal" => "65" ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Eficacy and safety of cefotaxime in combination with metronidazole for empirical treatment of brain abscess in clinical practice: a retrospective study of 66 consecutive cases" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "A.K. Jansson" 1 => "P. Enblad" 2 => "J. Sjölin" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s10096-003-1055-7" "Revista" => array:6 [ "tituloSerie" => "Eur J Clin Microbiol Infect Dis" "fecha" => "2004" "volumen" => "23" "paginaInicial" => "7" "paginaFinal" => "14" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/14669073" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] "agradecimientos" => array:1 [ 0 => array:4 [ "identificador" => "xack571968" "titulo" => "Acknowledgments" "texto" => "<p id="par0070" class="elsevierStylePara elsevierViewall">We would like to thank the Intensive Care Unit of University Clinical Hospital Lozano Blesa of Zaragoza (Spain).</p>" "vista" => "all" ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015700000011/v1_202112030828/S2387020621006422/v1_202112030828/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015700000011/v1_202112030828/S2387020621006422/v1_202112030828/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621006422?idApp=UINPBA00004N" ]
Journal Information
Vol. 157. Issue 11.
Pages e339-e340 (December 2021)
Share
Download PDF
More article options
Vol. 157. Issue 11.
Pages e339-e340 (December 2021)
Letter to the Editor
Brain abscess due to Cutibacterium acnes in a patient with HIV infection
Absceso cerebral por Cutibacterium acnes en un paciente con infección por el VIH
María José Arche Banzo
, Herminia Lozano Gómez, Sandra Herrero García
Corresponding author
Servicio de Medicina Intensiva, Hospital Clínico Universitario Lozano Blesa, Zargoza, Spain
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail