Influenza virus infection is associated with a high disease burden. COVID-19 caused by SARS-CoV-2 has become a pandemic outbreak since January 2020. Taiwan has effectively contained COVID-19 community transmission. We aimed to validate whether fighting COVID-19 could help to control other respiratory infections in Taiwan.
MethodWe collected week-case data of severe influenza, invasive Streptococcus pneumoniae disease and death toll from pneumonia among 25 calendar weeks of the influenza season for four years (2016–2020), which were reported to Taiwan CDC. Trend and slope differences between years were compared.
ResultA downturn trend of severe influenza, invasive S. pneumoniae disease and the death toll from pneumonia per week in 2019/2020 season and significant trend difference in comparison to previous seasons were noted, especially after initiation of several disease prevention measures to fight potential COVID-19 outbreak in Taiwan.
ConclusionsFighting COVID-19 achieved collateral benefits on significant reductions of severe influenza burden, invasive S. pneumoniae disease activity, and the death toll from pneumonia reported to CDC in Taiwan.
La COVID-19, causada por SARS-CoV-2, se ha convertido en un brote de pandemia desde enero de 2020. Taiwán ha contenido efectivamente la transmisión comunitaria de la COVID-19. Por otra parte, la influenza también es una enfermedad que se asocia con una alta carga de morbilidades. El objetivo del estudio es validar si combatir la COVID-19 podría ayudar a controlar otras infecciones respiratorias en Taiwán.
MétodosRecopilamos datos semanales de casos de influenza grave, infecciones invasivas por Streptococcus pneumoniae y número de muertes por neumonía, que se informaron a los CDC de Taiwán en las 25 semanas de la temporada de influenza durante 4años (2016-2020). Comparamos las diferencias de tendencia y de pendiente entre los años.
ResultadosSe observó una tendencia a la baja de la influenza grave, de las infecciones invasivas por Streptococcus pneumoniae y del número de muertes por neumonía por semana en la temporada de influenza de 2019-2020. Se observaron diferencias significativas en la tendencia en comparación con las temporadas anteriores, especialmente después del inicio de varias medidas de prevención de enfermedades para combatir el posible brote de COVID-19 en Taiwán.
ConclusionesPor el número de casos reportados a los CDC de Taiwán, encontramos que la lucha contra la COVID-19 logró beneficios colaterales en cuanto a reducción significativa de la carga de la influenza grave, a las infecciones invasivas por Streptococcus pneumoniae y al número de muertes por neumonía.
Influenza seasons usually run from November (calendar week 44) to following April (calendar week 16) each year. The number of cases commonly peaks during January and February. Influenza virus infection is associated with a high disease burden. The Centers for Disease Control and Prevention (CDC) estimates that influenza was associated with 45 million illnesses, 21 million medical visits, 810,000 hospitalizations, and 61,000 deaths during the 2017/2018 influenza season in the United States.1
A recent study in Japan reported that influenza activity was significantly lower in the 2019/2020 season versus the 2014 to 2019 seasons.2 The reasons for changing influenza activity might include the closure of schools, suspension of large events, and measures to reduce the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission among the Japanese public from early in the year.
In January 2020, the Taiwan government assembled a taskforce to contain the outbreak of Coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2, which was initially described in Wuhan, China. Taiwan had reported 440 laboratory-confirmed cases (including 55 indigenous cases, 349 imported cases and 36 Navy members aboard a combat fleet) after examining 68,335 suspicious persons by May 14 (https://www.cdc.gov.tw/En). Taiwan effectively contained community transmission by deployments of disease prevention measures, several policy decisions, and use of information technology.3–6 The success in the containment of the COVID-19 outbreak in Taiwan could verify the collateral benefit of containing influenza activity.
We proposed that collateral benefits on changing influenza activity and other respiratory infection activity (invasive Streptococcus pneumoniae disease) and outcome (death toll from pneumonia) would have happened in Taiwan.
MethodsWe use Taiwan CDC national data (https://nidss.cdc.gov.tw/en/ and https://nidss.cdc.gov.tw/ch/misc_query.aspx?dc=death_flu&dt=4&position=5) recording the number of PCR-confirmed severe influenza cases requiring admission to an intensive care unit (ICU), invasive S. pneumoniae disease and overall patients died in pneumonia per week among 25 calendar weeks of the influenza season each year (2016–2020). Theil-Sen trend test was used to calculate the trend of each whole influenza season and slope difference in comparison between years (http://www.singlecaseresearch.org/calculators/theil-sen). The slope between the upward trend (before the peak) or downward trend (after the peak) was compared season by season of each year using linear trend estimation method. SAS 9.4 for Windows (SAS Institute, Inc., Cary, NC, USA) was used for statistical analyses.
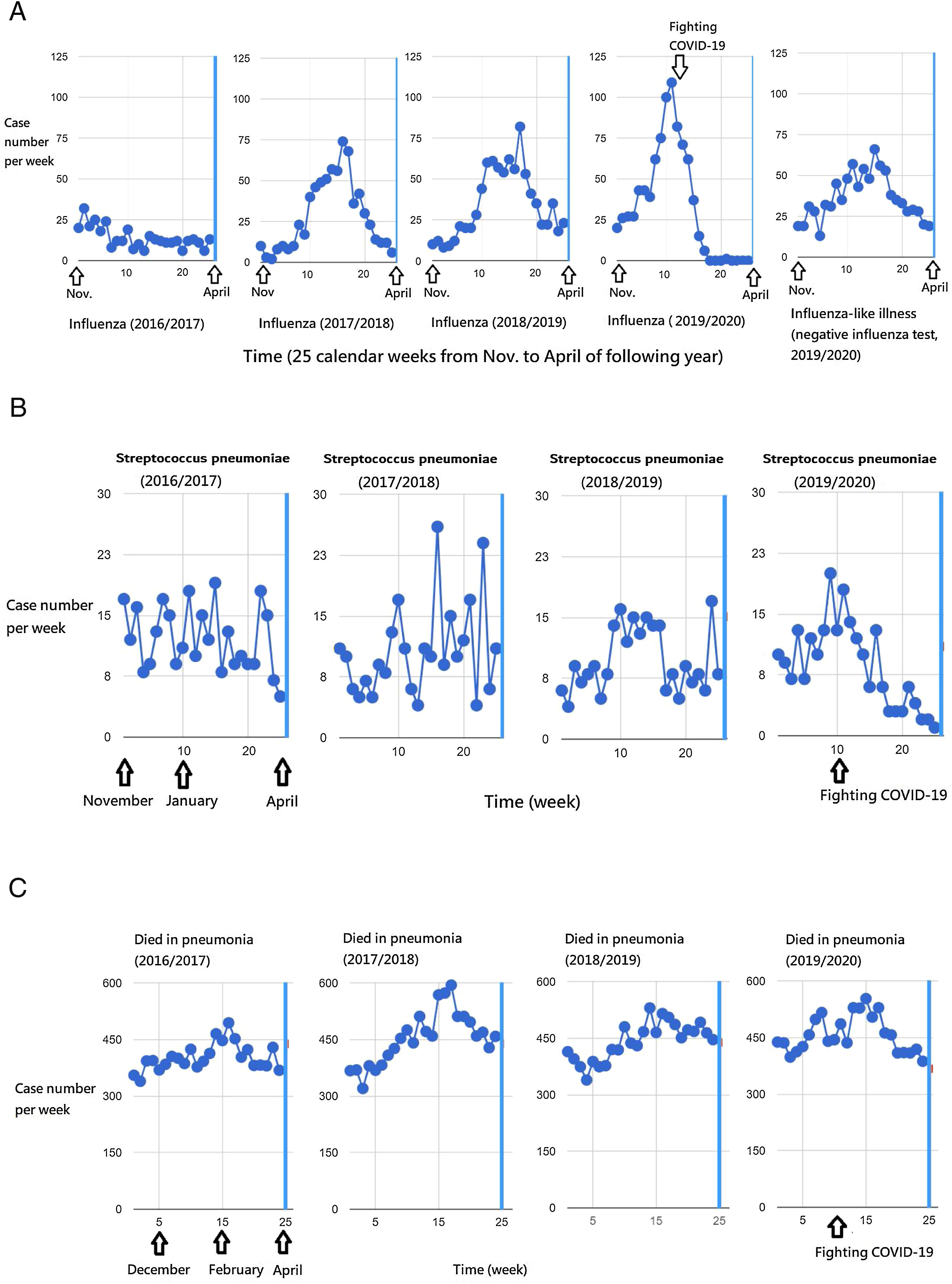
ResultsIn Fig. 1A, the peak weekly number of severe influenza cases increased from 2016/2017 season to 2019/2020 seasons, including 32, 74, 82, 109 cases per week in the four years respectively. The peak occurred in February (2017/2018 and 2018/2019 seasons) and January (2019/2020 season). If the peak in 2019/2020 season occurred in February as usual like the past two seasons, there would be a large outbreak of severe influenza in 2020. Nonetheless, the presumed outbreak did not happen in 2020, and a potential large influenza epidemic was abruptly shortened and reversed in January.
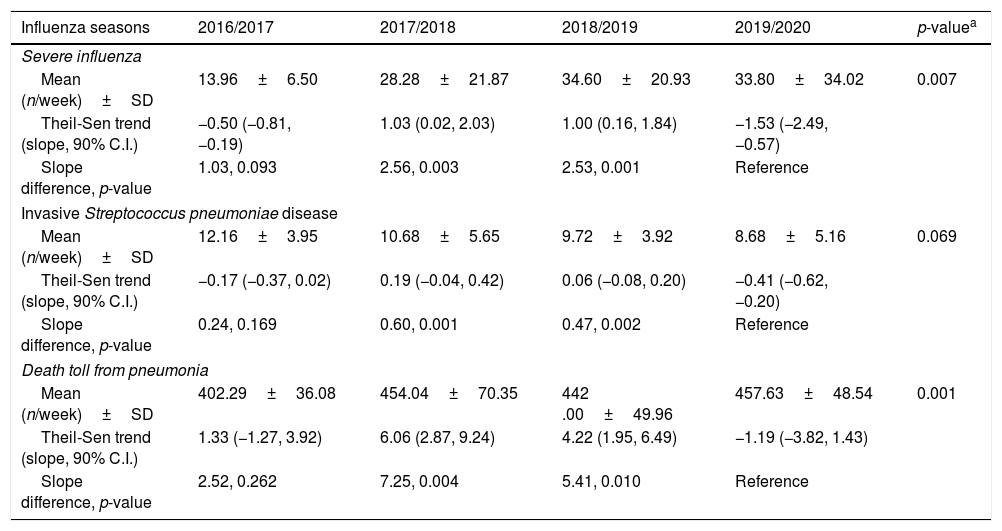
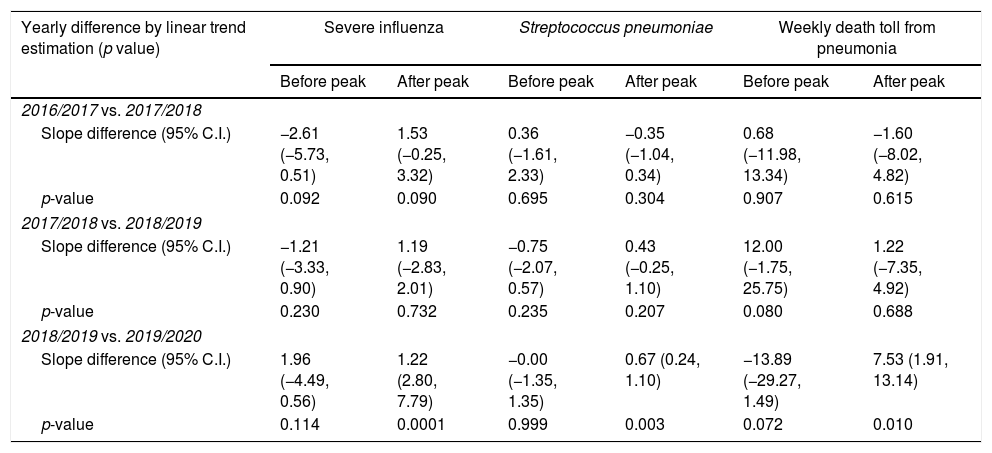
Influenza seasons run 25 weeks from November to following April each year. Taiwan's national severe influenza (2019/2020) case number dropped from a peak in January down to zero in March 2020 (A). The severe influenza and invasive Streptococcus pneumoniae activities were reversed from initiation of the measures to fight the COVID-19 outbreak in January (A and B). The death toll from pneumonia in the 2019/2020 influenza season was slightly downward in contrast to escalating trends of previous influenza seasons (C).
A noteworthy dropping of severe influenza from the top of a 2019/2020 season (109 cases at 2nd calendar week of the year) downhill to zero cases at the 9th calendar week (in early March). During the dramatic decrease in severe influenza cases in the later period of 2019/2020 season, a substantial of cases with severe influenza-like illness up to 66 cases in calendar week 6 and a total of 230 cases in March and April (for 8 weeks) was reported to Taiwan CDC. These cases were confirmed to be negative influenza tests (Fig. 1A). The number of reported negative influenza patients with influenza-like illness among the same 8 weeks in 2020 remained similar to 2019 (totally 216, p=0.297) and even more than 2018 (totally 172, p=0.048).
The trends of severe influenza weekly case number in 2017/2018, 2018/2019, and 2019/2020 revealed slopes of 1.03, 1.00, and −1.53, respectively. Compared to 2019/2020 influenza, the slope difference tests of influenza seasons were 2.56 (p=0.003) in 2017/2018 and 2.53 (p=0.001) in 2018/2019, both reaching statistical significance (Table 1). The trend also showed a downturn of weekly cases of invasive S. pneumoniae disease (slope, −0.41) in 2019/2020 influenza seasons, and compared to which, the trend difference tests were 0.60 (p=0.001) in 2017/2018 and 0.47 (p=0.002) in 2018/2019, both reaching statistical significance (Table 1 and Fig. 1B). Although the death toll from pneumonia in 2019/2020 influenza season is the highest (mean, 455) among the four-year influenza seasons (p=0.001), the trend of the weekly death toll from pneumonia dropped significantly in 2019/2020 (slope=−1.19), which was significantly different to 2017/2018 (slope difference=7.25, p=0.004) and 2018/2019 (slope difference=5.41, p=0.010) (Table 1 and Fig. 1C).
Collateral benefits on national severe influenza, invasive Streptococcus pneumoniae disease and the death toll from pneumonia while fighting COVID-19 from January 2020 in Taiwan, evidenced by significant slope difference compared to previous influenza seasons (25 weeks, from November to April of the following years).
| Influenza seasons | 2016/2017 | 2017/2018 | 2018/2019 | 2019/2020 | p-valuea |
|---|---|---|---|---|---|
| Severe influenza | |||||
| Mean (n/week)±SD | 13.96±6.50 | 28.28±21.87 | 34.60±20.93 | 33.80±34.02 | 0.007 |
| Theil-Sen trend (slope, 90% C.I.) | −0.50 (−0.81, −0.19) | 1.03 (0.02, 2.03) | 1.00 (0.16, 1.84) | −1.53 (−2.49, −0.57) | |
| Slope difference, p-value | 1.03, 0.093 | 2.56, 0.003 | 2.53, 0.001 | Reference | |
| Invasive Streptococcus pneumoniae disease | |||||
| Mean (n/week)±SD | 12.16±3.95 | 10.68±5.65 | 9.72±3.92 | 8.68±5.16 | 0.069 |
| Theil-Sen trend (slope, 90% C.I.) | −0.17 (−0.37, 0.02) | 0.19 (−0.04, 0.42) | 0.06 (−0.08, 0.20) | −0.41 (−0.62, −0.20) | |
| Slope difference, p-value | 0.24, 0.169 | 0.60, 0.001 | 0.47, 0.002 | Reference | |
| Death toll from pneumonia | |||||
| Mean (n/week)±SD | 402.29±36.08 | 454.04±70.35 | 442 .00±49.96 | 457.63±48.54 | 0.001 |
| Theil-Sen trend (slope, 90% C.I.) | 1.33 (−1.27, 3.92) | 6.06 (2.87, 9.24) | 4.22 (1.95, 6.49) | −1.19 (−3.82, 1.43) | |
| Slope difference, p-value | 2.52, 0.262 | 7.25, 0.004 | 5.41, 0.010 | Reference | |
We further look into if time trend (upward slope) of influenza before the peak in 2016/2017, which was insignificantly different from the slope in 2017/2018 (slope difference=−2.61, p=0.092) (Table 2). The statistical insignificance was also found in the results of 2017/2018 vs. 2018/2019 (slope difference=−1.21, p=0.230) and 2018/2019 vs. 2019/2020 (slope difference=1.96, p=0.114). For the downward trend difference after the peak, there was no significant difference in the results of 2016/2017 vs. 2017/2018 (slope difference=1.53, p=0.090) and 2017/2018 vs. 2018/2019 (slope difference=1.19, p=0.732). However, the slope difference between 2018/2019 and 2019/2020 reached statistical significance (slope difference=1.22, p=0.0001). The results were consistent in significant downward slope difference between 2018/2019 and 2019/2020 when examining weekly cases of invasive S. pneumoniae disease (slope difference=0.67, p=0.003) and the weekly number of patients died from pneumonia (slope difference=7.53, p=0.010), whereas the upward slope differences before the peak between different years were statistically insignificant (Table 2).
The slope differences between different time periods of each influenza season.
| Yearly difference by linear trend estimation (p value) | Severe influenza | Streptococcus pneumoniae | Weekly death toll from pneumonia | |||
|---|---|---|---|---|---|---|
| Before peak | After peak | Before peak | After peak | Before peak | After peak | |
| 2016/2017 vs. 2017/2018 | ||||||
| Slope difference (95% C.I.) | −2.61 (−5.73, 0.51) | 1.53 (−0.25, 3.32) | 0.36 (−1.61, 2.33) | −0.35 (−1.04, 0.34) | 0.68 (−11.98, 13.34) | −1.60 (−8.02, 4.82) |
| p-value | 0.092 | 0.090 | 0.695 | 0.304 | 0.907 | 0.615 |
| 2017/2018 vs. 2018/2019 | ||||||
| Slope difference (95% C.I.) | −1.21 (−3.33, 0.90) | 1.19 (−2.83, 2.01) | −0.75 (−2.07, 0.57) | 0.43 (−0.25, 1.10) | 12.00 (−1.75, 25.75) | 1.22 (−7.35, 4.92) |
| p-value | 0.230 | 0.732 | 0.235 | 0.207 | 0.080 | 0.688 |
| 2018/2019 vs. 2019/2020 | ||||||
| Slope difference (95% C.I.) | 1.96 (−4.49, 0.56) | 1.22 (2.80, 7.79) | −0.00 (−1.35, 1.35) | 0.67 (0.24, 1.10) | −13.89 (−29.27, 1.49) | 7.53 (1.91, 13.14) |
| p-value | 0.114 | 0.0001 | 0.999 | 0.003 | 0.072 | 0.010 |
The healthcare systems should report severe influenza cases to CDC in their clinical practice by the law on the prevention and control of infectious diseases in Taiwan. The decreasing influenza activity in February 2020 was not due to the negligence of physicians while focusing on fighting COVID-19 events, because substantial cases of severe influenza-like illness were still reported to the CDC in the same period, and they were turned out to be negative influenza tests. In addition, the reported death toll from pneumonia during late influenza seasons in 2020 was similar to or even higher than those in the same period of previous seasons. Finally, as COVID-19 outbreak prevailed in Wuhan, the influenza-like illness surveillance was suspended to handle the COVID-19 epidemic from the calendar week 3 (January) in Wuhan, China.7 Meanwhile, the COVID-19 pandemic did not really happen in Taiwan, so the CDC did not suspend the usual reporting practice. These facts would not support considering whether fighting against COVID-19 might have an influence on the physicians to report less for other respiratory infections.
The Theil-Sen slope, also known as the nonparametric linear regression slope, is an alternative to the standard linear regression slope and has relatively strong power and precision when data are non-normal and skewed.8 Therefore, we first use this method to measure the weekly case number of diseases through an influenza season. We found a significant downward trend and slope difference of severe influenza, invasive S. pneumoniae disease and death toll of pneumonia in comparison to previous seasons. Then we use the standard linear trend estimation to measure different periods before and after the peak of an influenza season, and we documented significant downward slope difference occurring after initiation of fighting COVID-19 in February 2020.
The Taiwan government did not lockdown cities nor close schools, restaurants, and nursing institutes. Why Taiwan could effectively contain the COVID-19 outbreak? SARS-CoV-2 was not tested by mass screening but was tested for risk persons who exposed to infected cases and for targeted indications of anyone with a fever, upper respiratory tract symptoms, or pneumonia of unknown etiology. For example, our hospital has conducted surveillance for SARS-CoV-2 in 3268 patients with relevant illness from outpatient clinics, wards, and ICUs by April 28. Among them, only 1 imported case was detected (data from the intranet of Chi Mei Medical Center). Our results supported limited community transmission in Taiwan.
Taiwan government has made several policies to integrate individual information to health care systems and the eMask ordering system.3–6 What other measures did Taiwanese public do with additional contributions to the significant reduction of severe influenza burden, invasive S. pneumoniae disease activity and the death toll from pneumonia? We herein sum up the preparedness and response to the Taiwan essential bundles according to published literature as follows: traffic flow control in hospitals to separate patients who were infected; alcohol sanitizer dispensers broadly used for hand washing and disinfection; isolation and quarantine persons confirmed or suspected to be infected; wearing a mask in public for everyone while entering a hospital or in the crowd; aerosol transmission reduced by social distancing; and no touching the face by hand and keeping safe on mask removal.3–6
The limitation of the study included retrospective data analysis and thus we are unable to discern which measure of the disease prevention bundles, such as universal masking practice or hand hygiene was an independent factor responsible for the successful containment of other respiratory infections. During fighting COVID-19, patients might avoid visiting a hospital for relatively mild respiratory tract infections. However, this would not influence reported severe influenza cases requiring ICU admission.
ConclusionsWe found collateral benefits of a significant reduction of weekly cases from severe influenza, invasive S. pneumoniae disease and the death toll from pneumonia during fighting COVID-19 in Taiwan. People raising public awareness, participating in disease prevention measures, together with hospital preparedness and response, helped the Taiwan government to contain transmission of respiratory infectious diseases and the outcome of pneumonia during the epidemic of COVID-19. The collateral benefit of nearly eradicating severe influenza supports to further study on the critical step of the disease prevention bundles, which may offer enormous help to prevent the epidemic influenza burden in the future.
Author contributionsDr Yu had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Dr Yu.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Financial supportNone declared.
Conflict of interestNone reported.