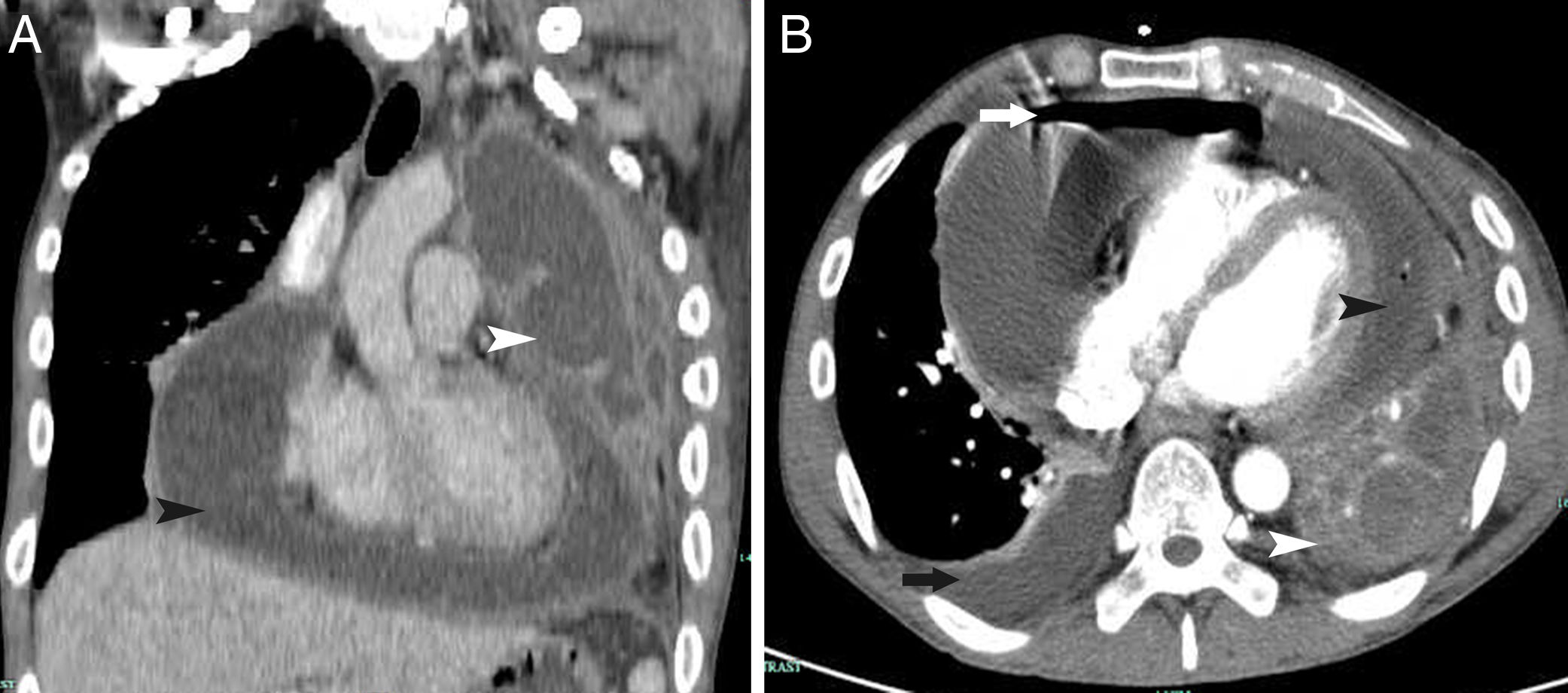
A 37-year-old man with a history of a left unilateral destroyed lung presented to the thoracic surgery department with a 2-week history of cough, dyspnea, and fever. The left unilateral destroyed lung was identified 3 years previously, and he received antituberculosis treatment for 1 year. Physical examination revealed the disappearance of respiratory sounds of the left lung, weakening of heart sounds, and severe edema of the lower limbs. Chest computed tomography revealed a left unilateral destroyed lung (Fig. 1, Panel A and B, white arrowhead), right pleural effusion (Panel B, black arrow), massive pericardial effusion (Panel A and B, black arrowhead), and pneumatosis (Panel B, white arrow). He underwent pericardiocentesis and drainage. His dyspnea and lower extremity edema worsened over the following 3 weeks. Constrictive pericarditis was diagnosed because of a significant increase in central venous pressure and clinical manifestations. Pericardiectomy and left pleuropneumonectomy were performed via only median sternotomy. Pathological examination did not suggest tuberculosis. Aspergillus fumigatus was identified in the drainage fluid by culture. Therefore, he received voriconazole for 3 months. A destroyed lung with hemoptysis and pulmonary infection is common; however, complication with constrictive pericarditis is rare. At the 2-year follow-up after surgery, he had recovered well.
Información de la revista
Vol. 155. Núm. 10.
Páginas 471 (noviembre 2020)
Vol. 155. Núm. 10.
Páginas 471 (noviembre 2020)
Image in medicine
Open Access
Destroyed lung with constrictive pericarditis
Pulmón destruido con pericarditis constrictiva
Visitas
1154
Zhejiang Chinese Medicine and Western Medicine Integrated Hospital, China
Este artículo ha recibido
Información del artículo
Texto completo
Copyright © 2019. The Author(s)